Abstract
Geriatric patients seem to be the most vulnerable group in COVID-19. These patients are usually characterized by impaired mobilization and malnutrition. In addition, obesity has been correlated with increased mortality rates after COVID-19 infection, highlighting the role of nutrition in prognosis of COVID-19 as well. In the past, several indices of nutritional status (GNRI) and functional status (ECOG performance status, Barthel Index, Handgrip Strength) have demonstrated a prognostic ability for hospitalized patients with influenza-like respiratory infections from coronavirus, metapneumovirus, parainfluenza and rhinovirus. Our hypothesis suggests that the previously mentioned nutritional and functional status indices, combined with the pneumonia severity index (CRB-65), could be useful in prognosis of morbidity and mortality of the elderly after the novel COVID-19 infection. Our hypothesis, is the first in the literature, which suggests a prognostic association between nutritional status of patients and COVID-19 infection, offering a quick and low-cost prognostic tool for COVID-19 in the elderly.
Keywords: COVID-19, Malnutrition, Frailty, Elderly, Functional status
Background
Since the new corona virus pandemic outburst, a plethora of research studies have been conducted and published in an impressively short period of time, emphasizing on potential risk and prognostic factors for the development and severity of corona virus disease 2019 (COVID-19). Age seems to be a significant predictor of death in patients admitted to the hospital, particularly due to the presence of comorbidities, such as cardiovascular disease and chronic obstructive pulmonary disease [1]. Nevertheless, little is known regarding the use of nutritional and functional status of patients as potential prognostic factors for COVID-19 outcome.
The hypothesis
Recent data support a strong relationship between malnutrition, either in the form of undernutrition or overnutrition, and infectious diseases. This association becomes stronger in specific populations, such as in older adults. The elderly constitute a more vulnerable group of patients due to immunosenescence and increased malnutrition rates [2], which in turn might result in a greater risk of developing severe complications after serious infections.
Even though data concerning patients’ nutritional status and COVID-19 are still lacking, the scientific community could take into account the results of previous research focused on respiratory viruses, in order to better define groups of patients who are at greater risk of infection-related mortality. More specifically, the impact of obesity on the severity of COVID-19 has garnered considerable attention, given that obese individuals are considered to have increased risk of obesity-driven chronic diseases (such as hypertension, diabetes mellitus etc.) that are related to severe complications of COVID-19 [3]. However, the effect of compromised nutritional status on COVID-19 progression has been underreported up to date.
Evaluation of the hypothesis
According to an observational cohort study of hospitalized and outpatient participants with influenza-like illness, underweight adults with influenza exhibited higher rates of hospitalization compared to their normal-weight counterparts. Moreover, in adults with coronavirus, metapneumovirus, parainfluenza and rhinovirus, underweight participants had four times higher risk of hospitalization compared to normal-weight adults [4]. Another interesting finding was observed in the study of Johnstone et al. [2], who investigated T-cell and natural killer cell phenotypes within nursing home elderly, as well as the impact of impaired nutrition and frailty on these parameters. Frailty and malnutrition significantly influenced participants’ regulatory T-cells and senescent natural killer cells, thus making them more prone to develop infectious diseases. Furthermore, frailty is a measure of overall health and due to its relevance to immune function and risk of respiratory viral infection [5], could be also used as a significant prognostic factor for COVID-19.
In addition, functional status could be a promising prognostic factor for patients suffering from COVID-19, as impaired physical function was independently associated with worst outcomes in hospitalized patients with community-acquired pneumonia, according to a recent prospective study [6]. In particular, Eastern Cooperative Oncology Group performance status (ECOG) ≥ 3 successfully predicted 30-days mortality rates, while the addition of ECOG performance status to the CRB-65 score (confusion, respiratory rate, blood pressure and age ≥ 65) significantly enhanced prognostication. This result is in accordance to the findings of Sanz et al. [7], who demonstrated that patients’ functional status, measured by the Barthel Index, was a stronger predictor of mortality than pneumonia severity index in patients aged ≥ 65 years who suffered from severe pneumonia. Moreover, a combined assessment using the pneumonia severity index and the Barthel Index, predicted more accurately mortality rates in these patients compared to the use of each index separately. The aforementioned findings suggest that the incorporation of patients’ functional status measurement into patient assessment may improve the prognostic ability of current risk classification systems to predict mortality from COVID-19 pneumonia.
The assessment of functional status is an indirect method to assess sarcopenia, which has emerged as a significant risk factor for pneumonia in older adults [8]. Sarcopenia is characterized by loss of muscle mass and strength and is influenced by the presence of chronic diseases, immobility and nutritional status. Sarcopenia is highly prevalent in older adults and is associated with higher risk of pneumonia, being an indicator of generalized muscle strength loss, including respiratory and oropharyngeal muscles. This evidence is supported by Altuna-Venegas et al. [9], who investigated the relationship between sarcopenia and incidence of community-acquired pneumonia in 1598 older adults. According to their results, an elevated risk of pneumonia in sarcopenic patients was observed, particularly in adults with higher rates of malnutrition.
Last but not least, Geriatric Nutritional Risk Index (GNRI) is a screening index of nutrition-related risk that correlates with the degree of nutritional deficit. GNRI is a combination of serum albumin level and the ratio of body weight to ideal body weight, according to the following formula: GNRI = [1.489 × albumin (g/L)] + [41.7 × (weight/WLo)], with lower levels of GNRI being indicative of severe malnutrition. GNRI has been reported as an independent prognostic factor for short-term hospital mortality in older patients with sepsis [10], since very high-risk patients (GNRI < 82) exhibited a six-fold increase in 28-day hospital mortality [11]. Moreover, Wang et al. highlighted that GNRI should attract the attention of the clinicians as a potential predictive factor for COVID-19 prognosis, based on recently published preliminary results [12]. Given that GNRI is a simple, objective, and fast method that links patients’ nutritional status to short and long-term outcomes, it should be considered as a potential predictor of COVID-19 severity and survival, irrespective of patients’ comorbidities.
Consequences of the hypothesis
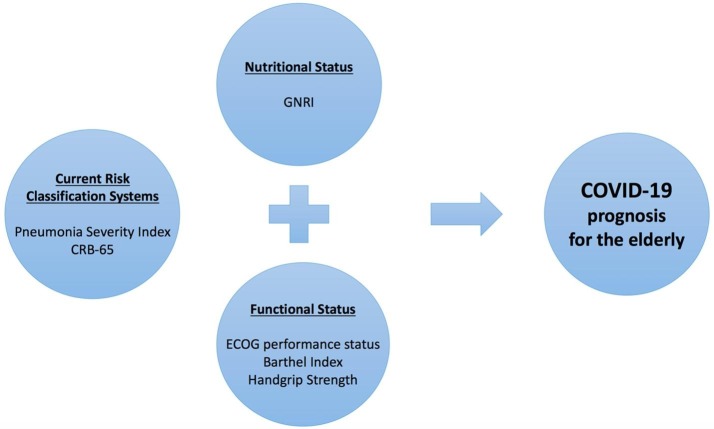
The present hypothesis is the first in the literature that proposes a prognostic association between nutritional and functional status of patients and prognosis after COVID-19 infection. Therefore, we strongly encourage the use of patients’ functional assessment measured either by the ECOG performance status, the Barthel Index or handgrip strength, as well as the evaluation of patients’ nutritional status based on the GNRI, since they are effective, non time-consuming methods that could be implemented in the clinical setting as the first step of detecting frail individuals (Fig. 1 ). These factors should be considered for risk stratification in order to prevent severe complications in older patients diagnosed with COVID-19. Nonetheless, further studies should be conducted in order to shed light on this promising approach.
Fig. 1.
Nutritional and functional assessment of the elderly patient presented with COVID-19. CRB-65, confusion, respiratory rate, blood pressure, age ≥ 65; GNRI, Geriatric Nutritional Risk Index; ECOG, Eastern Cooperative Oncology Group.
Conclusion
Nutritional status of patients seems to be associated with the novel COVID-19. The elderly, which are generally characterized by malnutrition, are more vulnerable to this virus and obesity has been proved as a risk factor for increased morbidity and mortality after COVID-19 infection. Several indices such as GNRI, ECOG and Barthel Index, have been used to assess the nutritional and functional status of elderly with similar viral respiratory infections. The combination of these indices with the traditional scores of respiratory infections’ severity, like PSI and CRB-65, may offer a quick and low-cost prognostic tool for COVID-19 in the elderly.
Source of funding
The authors received no specific funding for this work.
References
- 1.Wang L. Coronavirus Disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020 doi: 10.1016/j.jinf.2020.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnstone J. Immunosenescence in the nursing home elderly. BMC Geriatrics. 2014;14(1):50. doi: 10.1186/1471-2318-14-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ryan D.H., Ravussin E., Heymsfield S. COVID 19 and the patient with obesity-the editors speak out. Obesity. 2020 doi: 10.1002/oby.22808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moser J.A.S. Underweight, overweight, and obesity as independent risk factors for hospitalization in adults and children from influenza and other respiratory viruses. Influenza Other Respir Viruses. 2019;13(1):3–9. doi: 10.1111/irv.12618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnstone J. Immune biomarkers predictive of respiratory viral infection in elderly nursing home residents. PLoS ONE. 2014;(10):9. doi: 10.1371/journal.pone.0108481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jeon K. Functional status and mortality prediction in community-acquired pneumonia. Respirology. 2017;22(7):1400–1406. doi: 10.1111/resp.13072. [DOI] [PubMed] [Google Scholar]
- 7.Sanz F. A composite of functional status and pneumonia severity index improves the prediction of pneumonia mortality in older patients. J Gen Intern Med. 2018;33(4):437–444. doi: 10.1007/s11606-017-4267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lidoriki I., Schizas D. Are body mass index and performance status enough to assess the nutritional and functional status of elderly patients undergoing gastric cancer surgery? Surg Today. 2018;48(12):1100–1101. doi: 10.1007/s00595-018-1685-0. [DOI] [PubMed] [Google Scholar]
- 9.Altuna-Venegas S. Risk of community-acquired pneumonia in older adults with sarcopenia of a hospital from Callao, Peru 2010–2015. Arch Gerontol Geriatr. 2019;82:100–105. doi: 10.1016/j.archger.2019.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee J.S. Performance of the Geriatric Nutritional Risk Index in predicting 28-day hospital mortality in older adult patients with sepsis. Clin Nutr. 2013;32(5):843–848. doi: 10.1016/j.clnu.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Lidoriki I. GNRI as a prognostic factor for outcomes in cancer patients: a systematic review of the literature. Nutr Cancer. 2020:1–13. doi: 10.1080/01635581.2020.1756350. [DOI] [PubMed] [Google Scholar]
- 12.Wang N., Ou X. Caution should be exercised for the detection of SARS-CoV-2, especially in the elderly. J Med Virol. 2020 doi: 10.1002/jmv.25796. [DOI] [PubMed] [Google Scholar]