The coronavirus disease 2019 (COVID-19) pandemic has strained healthcare systems through increased care complexity, need for staff and patient safety, and surges in patients suspected or known to be infected with severe acute respiratory syndrome-coronavirus 2 (SARS-CoV2). Previous infectious disease outbreaks and natural disasters have altered clinical operations and ED performance in different manners depending on the disaster type and duration. During the 2009 H1N1 Influenza pandemic, total ED patient visits increased [1], and measures of ED performance such as patient length of stay (LOS), waiting time, left without being seen (LWBS) and boarding time were negatively affected [2,3]. Following a severe wildfire in San Diego, ED volumes decreased while rates of admission and LWBS increased [4]. Immediately following Hurricane Harvey, visits to free-standing EDs in Houston increased [5]. Conversely, after Hurricane Sandy, ED visits in New York plummeted but quickly returned to pre-disaster rates [6].
This retrospective review examines ED volumes and operational metrics of a health system in the Chicagoland area from January 1, 2020 to April 22, 2020. The seven hospitals analyzed were categorized by annual ED volumes and include: one very-high volume urban academic ED, one high-volume suburban community ED, and five average to low-volume community sites (Table 1 ). The following operational metrics were collected: median daily visits, COVID-19 specific visits, patients LWBS, door to diagnostic evaluation by a qualified medical professional (“door-to-doc” time), hospitalization rate, decision to admit to ED departure (boarding time), and median ED LOS.
Table 1.
Characterization of sites within the hospital system.
| Community class | Volume class | Inclusion/exclusion reason |
|---|---|---|
| Urban | Very high-volume (80–100 k) | Included |
| Suburban | High-volume (60–80 k) | Included |
| Suburban | Average-volume (40–60 k) | Included |
| Suburban | Moderate-volume (20–40 k) | Included |
| Suburban | Moderate-volume (20–40 k) | Included |
| Rural | Moderate-volume (20–40 k) | Included |
| Rural | Low-volume (<20 k) | Included |
| Rural | Low-volume (<20 k) | Excluded, insufficient data prior to 2/28/2020 |
| Rural | Low-volume (<20 k) | Excluded, insufficient data prior to 2/28/2020 |
| Rural | Low-volume (<20 k) | Excluded, insufficient data prior to 2/28/2020 |
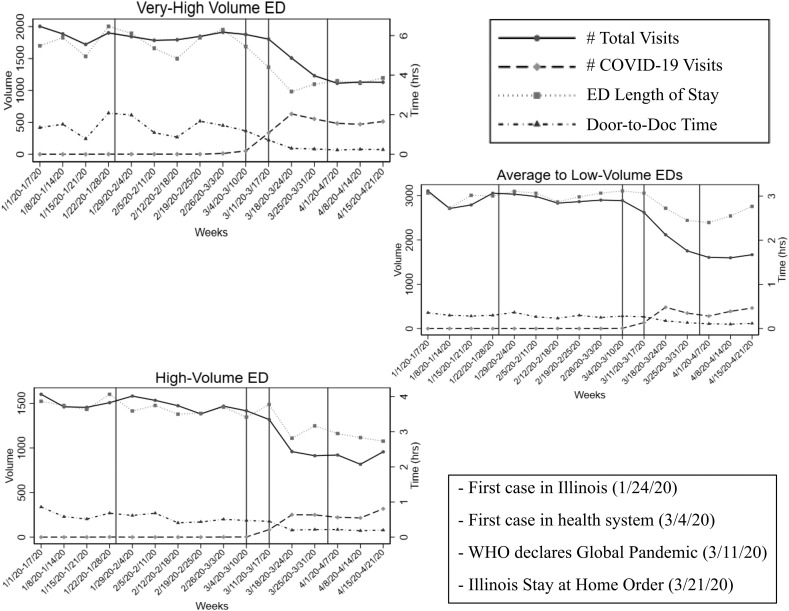
The study described three time periods determined by public health messaging and initial local cases: pre-COVID-19 (1/1/2020–3/3/2020), response (3/4/2020–3/24/2020), and post-response (3/25/2020–4/22/2020) (Fig. 1 ). Operational metrics were compared using the Wilcoxon Rank Sum Test. The Institutional Review Board approved this study.
Fig. 1.
Graphical representation of total number of patient encounters (weekly), COVID-19 related encounters (weekly), and median ED length of stay (hours) and door to doc time (hours). Hospitals were categorized by annual ED volumes into very-high volume (80–100 k), high-volume (60–80 k) and average to low-volume (<60 k). Noted are key dates including first case of COVID-19 in Illinois (1/24/2020), first case of COVID-19 in health system (3/4/2020), WHO declaration of global pandemic (3/11/2020) and State of Illinois Stay at Home order (3/21/2020).
Compared to the pre-COVID time period, median daily ED volume decreased in the post-response time period by 37.9%, 39.0% and 41.9% at very-high volume, high-volume and average to low-volume hospitals respectively (all p < 0.001) (Table 2 ). The median percentage of visits related to COVID-19 increased to 44.4%, 27.3%, 17.4% respectively (Table 2).
Table 2.
ED Operational Performance Metrics Across the Health System. Performance was subcategorized into three time periods: pre-COVID-19 (1/1/2020–3/3/2020), response (3/4/2020–3/24/2020), and post-response (3/25/2020–4/22/2020). LWBS, left without being seen; LOS, length of stay; D2D, door-to-doc time. Visits relating to COVID-19 were identified by any of the following criteria: SARS-CoV2 test ordered, presence of COVID-19 infection prevention flags (COVID-19, COVID-19 rule-out or COVID-19 presumed positive) in the electronic health record (EHR), or positive ED triage screen for COVID-19.
| Very high-volume academic |
High-volume suburban |
Average to low-volume community |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Pre-COVID | Response | Post-response | Pre-COVID | Response | Post-response | Pre-COVID | Response | Post-response | |
| Daily volume (#) | 265 (243–285) | 244 (229–277) | 164.5 (150–179) | 213 (198–227) | 181 (158–203) | 130 (116.5–141.5) | 93 (60–113) | 77 (39–102) | 54 (24–67) |
| LWBS (#) | 19 (7–27) | 8 (4–27) | 2 (1–3) | 6 (3–9) | 3 (1–6) | 3 (1.5–7) | 1 (0–2) | 1 (0–2) | 0 (0–2) |
| Admit (%) | 31.08 (27.43–32.94) | 24.78 (22.75–28.03) | 35.46 (33.6–37.33) | 26.43 (23.33–28.13) | 24.55 (21.26–26.79) | 29.04 (23.98–32.69) | 16.3 (9.68–24.3) | 16.81 (9.86–22.22) | 18.47 (11.22–25.54) |
| ED LOS (hrs) | 5.9 (5.18–6.81) | 4.4 (3.17–5.45) | 3.77 (3.42–3.91) | 3.74 (3.46–4.02) | 3.5 (3.05–3.78) | 2.9 (2.69–3.14) | 3 (2.43–3.7) | 2.98 (2.35–3.47) | 2.56 (2.14–2.88) |
| Boarding LOS (hrs) | 4.43 (3.45–5.77) | 3.03 (2.57–5.45) | 2.24 (2.11–2.56) | 1.8 (1.6–2.22) | 1.59 (1.42–1.88) | 1.62 (1.49–1.73) | 1.91 (1.42–2.92) | 1.75 (1.31–2.55) | 1.51 (1.25–2.41) |
| D2D (mins) | 91 (61–125) | 31 (19–71) | 14.75 (13–16) | 35 (26–44.5) | 24 (19–29) | 13 (11–14) | 18 (11−31) | 13 (8–23) | 7 (5–10) |
| COVID-19 (%) | 1 (0–1) | 16 (4–36) | 44.4 (41–46) | 0 (0–0) | 13 (2–25) | 27.3 (24–30) | 0 (0–0) | 10 (3−22) | 17.4 (12–28) |
The evaluation of operational metrics revealed the very high-volume urban academic ED experienced the greatest improvements, with LWBS, ED LOS, boarding time, and door-to-doc time decreasing by 89.5%, 36.1%, 49.4% and 83.8% respectively (all p < 0.001) (Table 3 ). Median daily and COVID-specific visits, median ED LOS, and waiting time (door-to-doc) are also displayed graphically (Fig. 1).
Table 3.
Changes in ED Operational Performance Metrics Across the Health System. Data are percent changes comparing the pre-COVID-19 (1/1/2020–3/3/2020) and the post-response (3/25/2020–4/22/2020) time periods. LWBS, left without being seen; LOS, length of stay; D2D, door-to-doc time.
| Very high-volume %Change | High-volume %Change | Average to low-volume %Change | |
|---|---|---|---|
| Daily volume (#) | −37.9%⁎⁎⁎ | −39.0%⁎⁎⁎ | −41.9%⁎⁎⁎ |
| LWBS (#) | −89.5%⁎⁎⁎ | −50.0%⁎ | −100.0%⁎ |
| Admit (%) | 14.1%⁎⁎⁎ | 9.9%⁎ | 13.30% |
| ED LOS (hrs) | −36.1%⁎⁎⁎ | −22.5%⁎⁎⁎ | −14.7%⁎⁎⁎ |
| Boarding LOS (hrs) | −49.4%⁎⁎⁎ | −10.0%⁎⁎ | −20.9%⁎⁎⁎ |
| D2D (mins) | −83.8%⁎⁎⁎ | −62.9%⁎⁎⁎ | −61.1%⁎⁎⁎ |
p < 0.05.
p < 0.01.
p < 0.001.
This analysis describes how a single pandemic can have a differential impact on individual hospitals, even within the same region and health system. Despite the higher proportion of COVID-related encounters, the very high-volume center saw greatest improvements in operational performance metrics. This is consistent with previous studies that have identified patient acuity and ED volume as strong predictors of ED performance [7]. Disaster preparedness efforts targeted at hospital decompression and reduction of ED demand, such as cancellation of elective surgeries, expansion of ICU capacity and dedicated outpatient COVID-19 testing areas may have the greatest impact at the more congested, urban academic center.
Prior studies have examined changes in ED volumes and associated operational measures during disasters. In contrast to volume surges seen in NYC urban EDs by a mean of 60.7% during the 2009 H1N1 outbreak [8], during the COVID-19 pandemic we describe decreased daily volumes by 37.9% in the urban ED and 41.9% in the community EDs. During the same H1N1 outbreak Atlanta experienced ED overcrowding as a result of the pandemic [9], whereas in this analysis, an improvement was seen in ED crowding metrics. These findings are, however, similar to those during the initial stages of the 2003 SARS epidemic in Hong Kong and Hurricane Sandy in NYC, when mean daily ED patient visits significantly decreased [6,10]. Evaluating the complex and temporal contributing factors driving these similarities and differences is beyond the scope of this analysis; however, hypothesized factors include the novelty of the disease, media coverage, presence of social distancing mandates, and messaging about when and where to seek care.
There are several study limitations. The analysis of a single health system limits generalizability to other regions and disasters. Specific conclusions on the nature of the ED visits other than those related to COVID-19 complaints cannot be drawn based on aggregate data. The retrospective, descriptive nature of this analysis limits the conclusions on causation or singular associations of variables.
The above data demonstrate a trend of decreased ED patient visits across a single health system during the initial stages of the COVID-19 pandemic, in conjunction with greater improvements in ED operational metrics observed at a large urban academic center compared to smaller community hospitals within the same health system. Although further data are needed to best characterize these patterns nationally, this early work points to a unique volume and metric impact in comparison to previous pandemics and natural disasters.
Prior presentations
None.
Funding sources
This research did not receive any specific grant funding from agencies in public, commercial, or not-for-profit sectors.
Author contributions
BAC: Analysis and interpretation of data, drafting of manuscript, revision of final manuscript, approval of final version.
EGW: Analysis and interpretation of data, drafting of manuscript, approval of final version.
PTS: Analysis and interpretation of data, drafting of manuscript, approval of final version.
DSC: Acquisition of data, approval of final version.
HSK: Concept and design, analysis and interpretation of data, revision of final manuscript, approval of final version.
DMM: Concept and design, analysis and interpretation of data, revision of final manuscript, approval of final version.
TML: Concept and design, analysis and interpretation of data, drafting of manuscript, revision of final manuscript, approval of final version.
Declaration of competing interest
BAC, EGW, PTS, DSC, HSK, DMM, TML: Declarations of interest: None.
Acknowledgments
Jennifer Chan, MD, MPH, Matthew Kippenhan, MD, and Sanjeev Malik, MD for their guidance and support of this report.
References
- 1.Schanzer D.L., Schwartz B. Impact of seasonal and pandemic influenza on emergency department visits, 2003–2010, Ontario, Canada. Acad Emerg Med. 2013;20:388–397. doi: 10.1111/acem.12111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wiler J.L., Welch S., Pines J., Schuur J., Jouriles N., Stone-Griffith S. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med. 2015;22:542–553. doi: 10.1111/acem.12654. [DOI] [PubMed] [Google Scholar]
- 3.Sivey P., McAllister R., Vally H., Burgess A., Kelly A.M. Anatomy of a demand shock: quantitative analysis of crowding in hospital emergency departments in Victoria, Australia during the 2009 influenza pandemic. PLoS One. 2019;14 doi: 10.1371/journal.pone.0222851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schranz C.I., Castillo E.M., Vilke G.M. The 2007 San Diego wildfire impact on the emergency department of the University of California, San Diego hospital system. Prehosp Disaster Med. 2010;25:472–476. doi: 10.1017/s1049023x0000858x. [DOI] [PubMed] [Google Scholar]
- 5.Pines J.M. Freestanding emergency department visits and disasters: the case of Hurricane Harvey. Am J Emerg Med. 2018;36:1513–1515. doi: 10.1016/j.ajem.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 6.Lee D.C., Smith S.W., Carr B.G., et al. Geographic distribution of disaster-specific emergency department use after hurricane Sandy in New York City. Disaster Med Public Health Prep. 2016;10:351–361. doi: 10.1017/dmp.2015.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Welch S.J., Augustine J.J., Dong L., Savitz L.A., Snow G., James B.C. Volume-related differences in emergency department performance. Jt Comm J Qual Patient Saf. 2012;38:395–402. doi: 10.1016/s1553-7250(12)38050-1. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro J.S., Genes N., Kuperman G., Chason K., Richardson L.D., Clinical Advisory Committee H1N1 Working Group NwYCIE Health information exchange, biosurveillance efforts, and emergency department crowding during the spring 2009 H1N1 outbreak in New York City. Ann Emerg Med. 2010;55:274–279. doi: 10.1016/j.annemergmed.2009.11.026. [DOI] [PubMed] [Google Scholar]
- 9.Sugerman D., Nadeau K.H., Lafond K., et al. A survey of emergency department 2009 pandemic influenza A (H1N1) surge preparedness—Atlanta, Georgia, July–October 2009. Clin Infect Dis. 2011;52(Suppl. 1):S177–S182. doi: 10.1093/cid/ciq035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Man C.Y., Yeung R.S., Chung J.Y., Cameron P.A. Impact of SARS on an emergency department in Hong Kong. Emerg Med (Fremantle) 2003;15:418–422. doi: 10.1046/j.1442-2026.2003.00495.x. [DOI] [PubMed] [Google Scholar]