Abstract
Background
Recently, we reported a strong, disease-independent relationship between accumulated preadult environmental risks and violent aggression later in life. Risk factors were interchangeable, and migration was among the explored risks. Alarmed by these data, we assessed collected risk load in young ‘healthy’ refugees as a specific subgroup of current migration streams and evaluated first signals of behavioral abnormalities.
Methods
In 9 German refugee centers, n = 133 young refugees, not previously in contact with the health system, were recruited, many of them unaccompanied minors. Risk factors experienced apart from migration/refuge were carefully assessed: Traumatic experiences before/during/after flight (including war, genocide, human trafficking, torture, murder, slavery, terrorist attacks), urbanicity, physical and sexual abuse, problematic alcohol and cannabis use (lifetime). Evaluation comprised physical exam and psychopathology screening.
Findings
Refugees arrived in Germany via Eastern Mediterranean/Balkan route (34.6%), from Africa via Central Mediterranean route (39.1%), by plane (17.3%) or other routes, such as Western Mediterranean or Atlantic (9.0%). Flight reasons were war/expulsion (25.6%), persecution/threats to life (51.9%), economical/others (22.5%). On top of migration/refuge, 42.8% of subjects had ≥3 risk factors; only 4.5% of refugees had no additional risks. Global level of functioning and severity of psychopathology were strongly associated with number of accumulated risks (Jonckheere–Terpstra trend-test: p = 7.61 × 10−7 and p = 3.62 × 10−7, respectively).
Interpretation
Young refugees, arriving in hosting countries with alarming 'risk burden', should be considered as highly vulnerable towards development of global functional deficits, behavioral abnormalities, and neuropsychiatric disorders. Rapid proactive integration or sustainable support of those who will return to rebuild their countries are mandatory.
Funding
The Max Planck Society supported this work.
Keywords: Migration, Flight routes, Trauma, Refugee minors, Psychopathology, Functioning
Research in context.
Evidence before this study
In 2005, we started assembling a neuropsychiatric disease population with thus far unprecedented level of phenotyping accuracy, including environmental risk factors. This deep phenotyping provided the ground for our recent discoveries that preadult accumulation of environmental risk factors is associated with a ∼10-year earlier onset of mental illness, and very robustly with the development of violent aggression/criminality in schizophrenia as well as in the general population. Migration was among the explored risks in these retrospective studies. This in turn led to the present work, aiming at a more prospective assessment of accumulated risks in young refugees and their immediate consequences for behavior, function and psychopathology. Conducting systematic literature searches (Medline, Google Scholar) in preparation of this publication revealed that an appreciable number of papers exists on psychological distress and mental disorders of migrants/refugees, mainly of earlier refuge waves, based on self-reports and questionnaires, but studies specifically targeting accumulation of environmental risk factors in the current refuge situation are rare, and definitely non-existing for young ‘healthy’ refugees.
Added value of this study
In a situation where migration/refuge has become a major socio-political issue in whole Europe, and where nearly two million individuals sought asylum in Germany over the last 5 years, the present study demonstrates that young ‘healthy’ refugees carry a considerable load of accumulated early risk factors. Only 6/133 (4.5%) of our young refugee cohort had no additional risks on top of migration. Global functioning and severity of psychopathology were strongly associated with the number of accumulated risks. Importantly, as we report, the risks are all interchangeable, just the number counts, still leaving room for prevention even after the flight.
Implications of all the available evidence
Considering the strong association of preadult risk accumulation with violent aggression and criminality later in life, communities and society in general are challenged to proactively find ways of more efficient integration or to sustainably support the potential of those who will return to their native countries. Re-evaluation of these individuals in several years – in case they are still contactable – will allow to estimate the predictable consequence of societal inactivity, namely a threatening number of subjects that will have developed violent aggression, criminality and radicalism, or severe mental illness.
Alt-text: Unlabelled box
1. Introduction
The impact of environmental risk on neuropsychiatric phenotypes has long been recognized [1], [2], [3], [4], [5], [6], [7]. However, studies on accumulation of risk factors, their impact in relation to genetic risk, and their effects on human behavior are sparse. When we started working on preadult accumulation of environmental risk factors, first in schizophrenic individuals, we made several surprising discoveries. Accumulation of ≥3 risk factors before the age of 18 years led to a nearly 10-year earlier onset of schizophrenia; the environmental risk factors were interchangeable, i.e. they could all replace each other, just the number was important; the impact of environmental risk was definitely stronger as compared to any common genetic risk [8,9]. From these robust findings, we moved on to compare extreme groups for exploring potential epigenetic alterations. Whereas epigenetic findings turned out to be minor, we encountered another unexpected observation during this follow-up study, namely that early accumulation of environmental risk was associated with violent aggressive and criminal behavior in adulthood [9]. This finding was obtained in 6 independent samples, including healthy cohorts. Migration, both first and second generation, was again among the environmental risk factors [9]. In fact, even once migrants have settled and formed families, their children, the second generation migrants, have an increased and even more pronounced risk of behavioral abnormalities and mental health problems [10].
In recent years, refuge, a specific subgroup of migration, has become a major socio-political issue in Europe. Since 2014, nearly 2 million individuals sought asylum in Germany, thus attributing to this country the by far biggest share among EU nations [11,12]. Furthermore, the overall number of refugees is highest ever worldwide and likely to increase further [11]. Reports speak about an enormous burden of mental health disorders in young refugees [12], [13], [14], [15], [16]. Similar information is available for earlier migration/refuge waves, all based on self-reports and questionnaires [17], [18], [19], [20], [21], [22], [23], [24], [25]. However, data on load of accumulated risks and its consequences are completely lacking.
In our previous work, we integrated retrospective data on migration (first and second-generation) as risk factors [8,9]. The present study was designed to start prospectively evaluating across German refugee asylums the accumulated environmental risk load of young migrants, many of them unaccompanied minors, who were not in previous contact with the health system. We demonstrate here a dramatic risk burden of these individuals on top of migration, and its stair-pattern like association with global functional deficits, behavioral abnormalities, and neuropsychiatric disorders. A follow-up study in several years will reveal data on the development of violent aggression, criminality and radicalism or of severe mental illness in this cohort.
2. Methods
2.1. Subjects and recruitment
The Ethic Committee of the Georg-August-University, Göttingen, approved the present study, complying with the Helsinki Declaration. All subjects gave written informed consent. For recruitment, we approached refugee centers and asked for their willingness to support our study. Of 15 centers contacted, only 9 felt able to provide us with suitable and willing participants (whom they pre-selected and informed). Upon positive feedback, we provided handouts, posters, flyers or other material (e.g. information and consent forms) for announcement through e.g. social workers/group meetings. Involved refugee centers (with refugee characteristics comparable all across) were: Waldkraiburg (34), Göttingen (24), Bad-Fallingbostel-Oerbke (22), Mühldorf am Inn (18), Heilbad Heiligenstadt (18), Braunschweig (13), Würzburg (2), Duderstadt (1), Heidelberg (1). Inclusion criteria were recent flight at young age, age at examination ≤30 years, no previous contact with the health system (individuals considered ‘healthy’), and the ability to communicate in English or German to widely avoid the need of interpreters as a potential source of uncertainty.
2.2. Sociodemographic data, level of functioning, and psychopathology parameters
An examination booklet was composed for the purpose of the present study to assure a standardized procedure for evaluation (compare GRAS manual [26]). This manual included semi-structured interviews regarding sociodemographic and flight-related parameters, extracts from questionnaires, as well as ratings using established instruments, available in German and English and validated/routinely used across cultures. They comprised the Positive and Negative Syndrome Scale (PANSS) [27], both the Hamilton and Montgomery–Åsberg Depression Scales [28,29], the Child Trauma Questionnaire (CTQ) [30], Global Assessment of Functioning (GAF) [31], Clinical Global Impression Scale (CGI) [32], as well as a brief, language-independent cognition test (performance test system subtest-3; 'Leistungsprüfsystem Untertest-3′ [33]), and physical including neurological examination guidelines. As experienced neurologist and psychiatrist and recruiting expert since 2004 (GRAS study [26]), MB performed all recruitment travel, refugee explorations and examinations in collaboration with local institutions.
2.3. Environmental risk exposure
Specific information was derived from history-taking and semi-structured interviews. In 8 cases (6%) the support of an interpreter turned out to be necessary. Each subject, having immigrated to Germany, was dichotomously classified as having/not having been exposed to: (1) traumatic experiences before and (2) during flight (war, genocide, slavery, kidnapping, human trafficking, torture, assaults, murder, threats to physical integrity, terrorist attacks, witnessed death of others). Further risk factors were also dichotomously determined according to our previous studies [8,9]: (3) Urbanicity was operationalized using information on places of residence and relocation. Each city the subjects lived in was allocated to one of four categories according to its total population. The category was then multiplied by the number of years that the person had spent living there. In cases of relocation, the same procedure was repeated for each new place of residence and values were added up to one urbanicity score per individual which was dichotomously grouped into rural and urban places of residence [8]. Moreover, (4) severe physical abuse (comprising unpredictability of violence, injury due to physical reprimand or objects for corporal punishment by family member or close persons), (5) sexual abuse (forced touches, kissing, attempted or real rape; any kind of clear sexual actions against the participant's will including negative sexual experiences during flight), (6) any cannabis consumption, and (7) alcohol abuse (lifetime) were assessed. In case of contradictory or missing information, subjects were rated ‘negative’ for the respective risk factor analysis. This conservative approach ultimately led to the exclusion of ‘perinatal/birth complications’ [8,34] as an originally planned, yet unreliable risk factor in the present cohort, but did not apply to any other risk information. Single risk factors were then accumulated to obtain the combined influence on level of global functioning, behavior and mental state. To test for multicollinearity between the risk factors included in the accumulation model, we calculated the variance inflation factor (VIF). Our results suggest that none of the included factors significantly collinears with any other (VIF ≤ 1.38, tolerance > 0.72), allowing us to include them in our models.
Consistency and truth of answers was systematically ensured by various questions targeting the same topic throughout the interview as well as by careful crosschecking of all obtained information including our extensive physical examination. The Rey Memory Test (RMT) [35] was used as additional indicator of simulating or aggravating behavior. RMT suggests that individuals with low score (i.e. <9 out of 15 correct answers) may simulate or aggravate severity of neurocognitive symptoms. In our sample, only 5 out of 133 participants (<4%) performed with such low score. However, in these cases, the following systematic examination and the use of all obtained information led us to the conclusion that their answering throughout our examination (including information on previous contact with the mental health system) was consistent and true.
2.4. Statistical analysis of environmental risk
Group differences for continuous variables were assessed using Mann–Whitney-U or Kruskal–Wallis-H test for comparison of >2 groups. Frequency differences between groups were assessed using Fisher's exact test. As trend tests, Jonckheere–Terpstra or Cochran–Armitage tests were applied. Bonferroni correction accounted for multiple testing (p-values withstanding correction denoted). All statistical analyses as well as the creation of Fig. 1(A) have been carried out using R v3.5.2 (R-Foundation for Statistical Computing, Vienna, Austria) with RStudio v1.1.463 (RStudio Inc., Boston, United States).
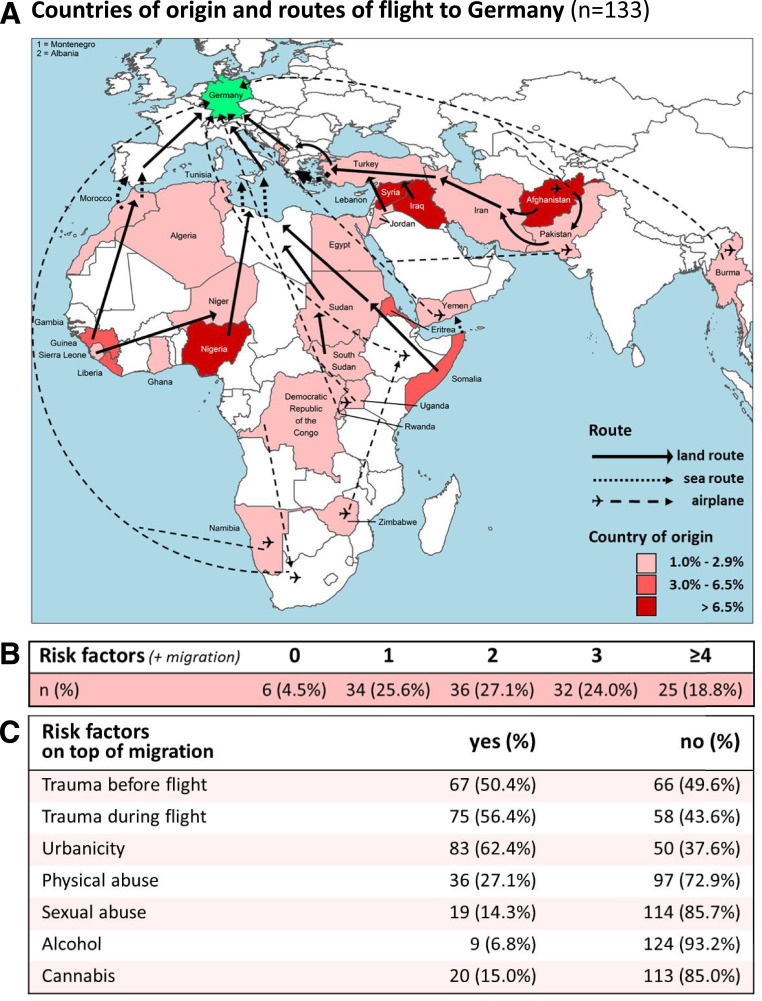
Fig. 1.
Countries of origin and routes of flight to Germany as well as overview of the number of experienced risk factors. (A) Map integrating information on countries of origin and routes of flight to Germany (n = 133). (B) Number of experienced risk factors. Note that 43% of subjects have an accumulation of 3 or ≥4 risk factors on top of migration. (C) Dichotomous presentation of experienced risk.
2.5. Role of funding
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
3. Results
In 9 German refugee centers, a total of n = 133 young refugees (∼80% males), not previously in contact with the health system, were recruited from June 2018 to May 2019, many of them unaccompanied minors (age at flight: 18.3 ± 4.1 years; age at arrival in Germany: 20.2 ± 4.3; age at examination: 22.1 ± 3.4). Those who agreed in the first place to participate in the study did complete it (no dropouts among the individuals pre-selected by the refugee centers). Flight routes and countries of origin of this sample of young ‘healthy’ refugees are displayed in Fig. 1(A). Refugees arrived in Germany via Eastern Mediterranean/Balkan route (34.6%), from Africa via Central Mediterranean route (39.1%), by plane (17.3%) or other routes, such as Western Mediterranean or Atlantic route (9.0%). Flight reasons were war/expulsion (25.6%), persecution and threats to life (51.9%), economical and others (22.5%). Most individuals had a passport from Afghanistan (27), or came from Nigeria (23), Syria (12) and Iraq (11). Distribution of countries of origin and sample composition may be somewhat biased by our request to avoid the need of interpreters, mainly to assure transparency of information. Except for 8 individuals, where interpreters had finally to be involved, communication in German or English was sufficiently possible. Around 60% of refugees traveled alone, 40% together with family or friends, but the accumulation of risks did not seem to be influenced by this fact (p = 0.292), nor the degree of psychopathology or level of functioning (all p > 0.3). Similarly, being post-flight in a close and stable relationship as a potentially protective factor (only 25%) did not affect accumulated risks nor outcome (all p > 0.3).
We assumed that the route, e.g. the highly dangerous African/Central-Mediterranean versus the Middle East/Eastern-Mediterranean route, would prime flight experiences. Nevertheless, there was no appreciable difference in assessed risk accumulation or outcome measures dependent on the flight route. Evaluation of experienced risks on top of migration identified 42.8% of subjects with ≥3 risk factors; only 4.5% of refugees had no additional risks (Fig. 1(B)).
Fig. 1(C) gives a dichotomous overview of the presence of risk factors. Over 50% of subjects suffered traumatic experiences before and during the flight, with most individuals coming from urban environment as an additional risk factor. Physical exam uncovered that many asylum seekers had suffered not only from psychological injuries. In fact, 54 individuals (40%) exhibited severe scars/wounds from externally inflicted injuries, such as gunshots, shrapnel or stab wounds, bomb explosions, burning or electrical shocks. All other readouts of physical exam were unremarkable; none of the subjects had any detectable neurological symptoms including soft signs.
Additional physical and sexual abuse (apart from flight experiences) became evident in 27% and 14%, respectively. Drug consumption was, in good agreement with recent literature [36], relatively low, with cannabis and alcohol amounting to 15% and 7%. Importantly, however, among the consumers of cannabis, 4 unaccompanied male refugees (3%), still minors during the flight, revealed clear and thus far undetected psychotic symptoms, 2 of them with suicidality.
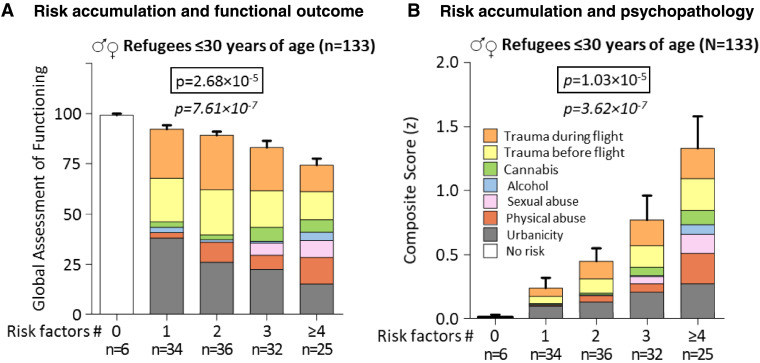
Neuropsychiatric and functional outcome evaluation disclosed highly significant associations between accumulation of risk factors on top of migration and global functioning (GAF; Fig. 2(A)) as well as degree of psychopathology (Fig. 2(B)). These findings are illustrated using a psychopathology composite score, consisting of Clinical Global Impression (CGI), PANSS total, Hamilton Depression Scale, and Montgomery–Åsberg Depression Scale (Cronbach's alpha 0.952). Striking stair-patterns arise upon graphical presentation (Fig. 2). We tested our risk accumulation models additionally via linear regression and found comparable results for both GAF (intercept = 99.45; amount of risk = −5.85; F(1; 131) = 29.64; p = 2.48 × 10−7; R2 = 0.185) and psychopathology composite score (intercept = −0.76; amount of risk = 0.34; F(1; 131) = 28.07; p = 4.81 × 10−7; R2 = 0.177). Importantly, essentially all single psychopathology readouts by themselves were already significant (Table 1).
Fig. 2.
Accumulation of environmental risk factors in young ‘healthy’ flight migrants and their association with level of functioning and psychopathological outcome. (A) Risk accumulation and functional outcome rated by the Global Assessment of Functioning (GAF) scale; note the stair-like decrease in daily life functioning in relation to the amount of negative environmental risk experienced. (B) Risk accumulation and severity of psychopathology, rated as composite score of Clinical Global Impression (CGI), total score of Positive and Negative Syndrome Scale, PANSS, as well as Hamilton and Montgomery–Åsberg Depression Scales; note the stair-like increase in psychopathology with increasing numbers of risks; z-scores adjusted to positive values. Two-sided Kruskal–Wallis H-test and one-sided Jonckheere–Terpstra test for trends (below; italics) presented.
Table 1.
Effects of accumulated environmental risk on functioning and psychopathology in young refugees
| Number of risk factors on top of migration: | 0 | 1 | 2 | 3 | ≥4 | p value | p value |
|---|---|---|---|---|---|---|---|
| n=6 (4.5%) | n=34 (25.6%) | n=36 (27.1%) | n=32 (24.0%) | n=25 (18.8%) | (χ2, H) | (z, J)* | |
| Global Assessment of Functioning (GAF) | 99.17 (2.04) | 92.24 (11.94) | 89.22 (11.14) | 83.19 (18.79) | 74.24 (17.03) | 2.68 × 10-5 (H=26.36) | 7.61 × 10−7 (J=2189) |
| Clinical Global Impression (CGI) | 1.00 (0.00) | 1.50 (0.93) | 1.75 (1.00) | 2.34 (1.54) | 3.04 (1.43) | 9.44 × 10−6 (H=28.60) | 4.78 × 10−7 (J=4610) |
| PANSS total | 30.17 (0.41) | 31.21 (2.17) | 33.19 (4.52) | 36.38 (11.44) | 39.08 (11.19) | 9.16 × 10−4 (H=18.66) | 4.17 × 10−5 (J=4369) |
| PANSS positive | 7.00 (0.00) | 7.03 (0.17) | 7.25 (0.76) | 7.81 (2.66) | 8.20 (2.61) | 0.024 (H=11.27) | 0.020 (J=3899) |
| PANSS negative | 7.00 (0.00) | 7.06 (0.24) | 7.33 (0.86) | 9.19 (6.18) | 9.12 (3.58) | 0.001 (H=17.80) | 0.002 (J=4094) |
| PANSS general | 16.17 (0.41) | 17.12 (2.10) | 18.61 (3.70) | 19.38 (4.89) | 21.76 (6.35) | 0.002 (H=17.23) | 7.91 × 10−5 (J=4330) |
| Diagnoses** | 0 (0.0%) | 7 (20.6%) | 9 (25.0%) | 14 (43.8%) | 18 (72.0%) | 9.19 × 10−5 (χ2=23.64) | 1.63 × 10−6 (z=-4.65) |
| Hamilton Depression Scale | 0.17 (0.41) | 1.71 (3.21) | 2.64 (3.77) | 3.69 (5.67) | 8.00 (7.69) | 3.56 × 10−5 (H=25.75) | 8.73 × 10−6 (J=4459) |
| Montgomery-Åsberg Depression Scale | 0.17 (0.41) | 1.50 (2.79) | 3.00 (4.30) | 4.59 (7.06) | 8.64 (9.72) | 2.24 × 10−4 (H=21.76) | 1.13 × 10−6 (J=4444) |
| Psychopathology composite score (z) | -0.62 (0.05) | -0.38 (0.49) | -0.17 (0.62) | 0.15 (1.08) | 0.71 (1.24) | 1.03 × 10−5 (H=28.42) | 3.62 × 10−7 (J=4624) |
| Suicidality | 0 (0.0%) | 2 (5.9%) | 1 (2.8%) | 0 (0.0%) | 6 (24.0%) | 0.009 (χ2=15.48) | 0.013 (z=-2.24) |
Urbanicity, physical abuse, sexual abuse, problematic alcohol use, cannabis use, traumatic experiences before flight, and traumatic experiences during flight are included in the accumulation model; data are uncorrected means (SD) or n (%); for statistical analysis, Kruskal-Wallis-H or Fisher's exact test was used. PANSS, Positive and Negative Syndrome Scale; psychopathology composite score consists of scores of Clinical Global Impression, PANSS total, Hamilton Depression Scale, and Montgomery-Åsberg Depression Scale, yielding a Cronbach's alpha of 0.952; suicidality, individuals with recent suicide attempts. The p values withstanding Bonferroni correction are bolded. *To test for statistical trends, one-sided Cochran-Armitage trend (qualitative traits) or Jonckheere-Terpstra trend (quantitative traits) tests were used. **’Diagnoses’ refer to mental disease diagnoses obtained during exam of refugees, previously considered ‘healthy’ (mainly PTSD).
4. Discussion
In the present investigation, a substantial load of accumulated environmental risk factors became obvious in young ‘healthy’ refugees on top of migration/refuge.
Pre-flight and flight experiences of these young individuals frequently included extreme poverty, genocide, war, experience of terror, torture, persecution for ethnic or religious reasons or sexual orientation, kidnapping, slavery, human trafficking, sexual exploitation, forced labor, physical maltreatment, separation trauma, experiencing or witnessing assaults, massacres, rape and other threats to physical integrity, as well as murder and terrorist attacks.
Post-flight experiences, i.e. problems upon arrival in the hosting country, here Germany, comprised problematic living conditions, multiple relocations, non-access to education and labor, maladaptation to language and culture, uncertain legal and residential status. In addition, social exclusion and hostility towards foreigners and refugees constitute post-flight reality. Especially in young refugees, this devastating situation adds to their already severe identity crisis with all its consequences for self and society. This may at least partly explain the increased suicidality of young migrants seen here and reported elsewhere [37].
As in our previous work [8,9], also in the present study, which directly targeted refugees, the deleterious effect of preadult risk accumulation on human behavior, level of functioning and well-being becomes drastically evident. Again, the composition of risk factors, the 'risk cocktail', is apparently less relevant for the overall outcome of individuals as compared to the number of accumulated risks, which ultimately determines the result. The harm to the juvenile brain, both psychological and physiological, seems to add up in a venomous fashion on brain functions in the sense of dosis facit venenum. It is thus not too surprising, that there was no appreciable difference in outcome measures, global functioning and psychopathology, dependent on the flight route. It appears that environmental hazards, striking at a vulnerable time of brain development, differ in their initial mechanisms of action on the brain, but likely feed into final common deleterious pathways downstream. Knowledge on hypothetical biological mechanisms underlying this accumulation effect are mainly derived from animal models. Molecular pathways and functions affected seem multifaceted, ranging from neuroendocrine and neurotransmitter systems, neuronal/synaptic plasticity and neurogenesis, to changes in the adaptive immune system and interference with developmental myelination, affecting brain connectivity and network function [5,6,38,39].
Coping and help-search strategies are to an essential degree influenced by social status, education, familial, religious, and sociocultural values. We chose mainly individuals with whom communication in German or English was sufficiently possible. This certainly introduced some bias towards higher educational level of included subjects, likely evolving as a protective factor, boosting resilience. Surprisingly, however, we did not see in our sample any appreciable effect of supposed protective factors, e.g. flight alone versus with company, or of being in a close relationship post-flight, on number of accumulated risks or on outcome. This lack of associations may be due to the still relatively small sample size, but strong effects at least are unlikely.
Empathic attitude in the host country toward young refugees, addressing health and educational needs as well as secure sheltering, will generate confidence and stability, thus ultimately contributing to a positive outcome of these individuals. However, we should not forget the strong associations shown in 6 independent cohorts of accumulated preadult risk with violent aggression and criminality later in life [9], imposing a clear threat to societal inactivity with regard to integration. Predictable consequences may include a threatening number of subjects that will have developed severe aggression, criminal behavior, and potentially even radicalism, apart from those suffering from severe mental illness.
In fact, also to prevent such consequences, communities and society in general are challenged either to find successful and proactive ways of fast integration in the German/European heritage or to swiftly but sustainably support the potential of those who will return for rebuilding and/or contributing to prosperity and welfare in their native countries. Re-evaluation of still contactable individuals in several years will allow estimating the predictable consequences of societal dormancy, namely a considerable number of high-risk subjects that will have developed violent aggression, criminality and radicalism. Reducing this number should be our common goal.
An important impulse, expected from the present study, is to inform current policies and guidelines and to encourage respective innovative strategies. These include careful initial physical examination, regular health check-ups of refugees and prevention of further risk accumulation. This might be achieved through generation of alternatives to typical refugee accommodations and ghettos, integration from scratch by distributing refugees immediately among other citizens as well as keeping them positively busy. Refugees should be enabled to move away from just being cared-for to self-help plans. A somewhat provocative but ultimately successful idea would be to provide instantaneously jobs/contracts and let them earn their own modest living by supportive work. This requires perhaps modifications of existing legislation, but could then start immediately after the refuge and should be accompanied by regular social worker visits and language training/courses, until the decision of staying or leaving has been made by the authorities. Meanwhile refugees should be free to search in parallel for more adequate jobs with respect to their education or for apprenticeships.
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
This work was supported by the Max Planck Society. The authors thank all subjects for participating in the study.
References
- 1.van Os J., Kenis G., Rutten B.P. The environment and schizophrenia. Nature. 2010;468(7321):203–212. doi: 10.1038/nature09563. [DOI] [PubMed] [Google Scholar]
- 2.Brown A.S. The environment and susceptibility to schizophrenia. Prog Neurobiol. 2011;93(1):23–58. doi: 10.1016/j.pneurobio.2010.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lederbogen F., Kirsch P., Haddad L. City living and urban upbringing affect neural social stress processing in humans. Nature. 2011;474(7352):498–501. doi: 10.1038/nature10190. [DOI] [PubMed] [Google Scholar]
- 4.Orlovska S., Pedersen M.S., Benros M.E., Mortensen P.B., Agerbo E., Nordentoft M. Head injury as risk factor for psychiatric disorders: a nationwide register-based follow-up study of 113,906 persons with head injury. Am J Psychiatry. 2014;171(4):463–469. doi: 10.1176/appi.ajp.2013.13020190. [DOI] [PubMed] [Google Scholar]
- 5.McEwen B.S., Nasca C., Gray J.D. Stress effects on neuronal structure: hippocampus, amygdala, and prefrontal cortex. Neuropsychopharmacology. 2016;41(1):3–23. doi: 10.1038/npp.2015.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nemeroff C.B. Paradise lost: the neurobiological and clinical consequences of child abuse and neglect. Neuron. 2016;89(5):892–909. doi: 10.1016/j.neuron.2016.01.019. [DOI] [PubMed] [Google Scholar]
- 7.Ehrenreich H. The impact of environment on abnormal behavior and mental disease: to alleviate the prevalence of mental disorders, we need to phenotype the environment for risk factors. EMBO Rep. 2017;18(5):661–665. doi: 10.15252/embr.201744197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stepniak B., Papiol S., Hammer C. Accumulated environmental risk determining age at schizophrenia onset: a deep phenotyping-based study. Lancet Psychiatry. 2014;1(6):444–453. doi: 10.1016/S2215-0366(14)70379-7. [DOI] [PubMed] [Google Scholar]
- 9.Pan H., Oliveira B., Saher G. Uncoupling the widespread occurrence of anti-NMDAR1 autoantibodies from neuropsychiatric disease in a novel autoimmune model. Mol Psychiatry. 2019;24(10):1489–1501. doi: 10.1038/s41380-017-0011-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cantor-Graae E., Selten J.P. Schizophrenia and migration: a meta-analysis and review. Am J Psychiatry. 2005;162(1):12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- 11.United Nations High Commissioner for Refugees (UNHCR) Author; Geneva, Switzerland: 2019. Global trends: forced displacement in 2018. [Google Scholar]
- 12.Abbott A. The mental-health crisis among migrants. Nature. 2016;538(7624):158–160. doi: 10.1038/538158a. [DOI] [PubMed] [Google Scholar]
- 13.Demazure G., Gaultier S., Pinsault N. Dealing with difference: a scoping review of psychotherapeutic interventions with unaccompanied refugee minors. Eur Child Adolesc Psychiatry. 2018;27(4):447–466. doi: 10.1007/s00787-017-1083-y. [DOI] [PubMed] [Google Scholar]
- 14.El-Awad U., Fathi A., Petermann F., Reinelt T. Promoting mental health in unaccompanied refugee minors: recommendations for primary support programs. Brain Sci. 2017;7(11):1–12. doi: 10.3390/brainsci7110146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.von Werthern M., Grigorakis G., Vizard E. The mental health and wellbeing of unaccompanied refugee minors (URMs) Child Abuse Negl. 2019;98 doi: 10.1016/j.chiabu.2019.104146. [DOI] [PubMed] [Google Scholar]
- 16.Brandt L., Henssler J., Muller M., Wall S., Gabel D., Heinz A. Risk of psychosis among refugees: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76(11):1133–1140. doi: 10.1001/jamapsychiatry.2019.1937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bean T., Derluyn I., Eurelings-Bontekoe E., Broekaert E., Spinhoven P. Comparing psychological distress, traumatic stress reactions, and experiences of unaccompanied refugee minors with experiences of adolescents accompanied by parents. J Nerv Ment Dis. 2007;195(4):288–297. doi: 10.1097/01.nmd.0000243751.49499.93. [DOI] [PubMed] [Google Scholar]
- 18.Bean T.M., Eurelings-Bontekoe E., Spinhoven P. Course and predictors of mental health of unaccompanied refugee minors in the Netherlands: one year follow-up. Soc Sci Med. 2007;64(6):1204–1215. doi: 10.1016/j.socscimed.2006.11.010. [DOI] [PubMed] [Google Scholar]
- 19.Vervliet M., Lammertyn J., Broekaert E., Derluyn I. Longitudinal follow-up of the mental health of unaccompanied refugee minors. Eur Child Adolesc Psychiatry. 2014;23(5):337–346. doi: 10.1007/s00787-013-0463-1. [DOI] [PubMed] [Google Scholar]
- 20.Vervliet M., Meyer Demott M.A., Jakobsen M., Broekaert E., Heir T., Derluyn I. The mental health of unaccompanied refugee minors on arrival in the host country. Scand J Psychol. 2014;55(1):33–37. doi: 10.1111/sjop.12094. [DOI] [PubMed] [Google Scholar]
- 21.Derluyn I., Mels C., Broekaert E. Mental health problems in separated refugee adolescents. J Adolesc Health. 2009;44(3):291–297. doi: 10.1016/j.jadohealth.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 22.Derluyn I., Broekaert E., Schuyten G., De Temmerman E. Post-traumatic stress in former Ugandan child soldiers. Lancet. 2004;363(9412):861–863. doi: 10.1016/S0140-6736(04)15734-6. [DOI] [PubMed] [Google Scholar]
- 23.Hodes M., Jagdev D., Chandra N., Cunniff A. Risk and resilience for psychological distress amongst unaccompanied asylum seeking adolescents. J Child Psychol Psychiatry. 2008;49(7):723–732. doi: 10.1111/j.1469-7610.2008.01912.x. [DOI] [PubMed] [Google Scholar]
- 24.Sleijpen M., Boeije H.R., Kleber R.J., Mooren T. Between power and powerlessness: a meta-ethnography of sources of resilience in young refugees. Ethn Health. 2016;21(2):158–180. doi: 10.1080/13557858.2015.1044946. [DOI] [PubMed] [Google Scholar]
- 25.Smid G.E., Lensvelt-Mulders G.J., Knipscheer J.W., Gersons B.P., Kleber R.J. Late-onset PTSD in unaccompanied refugee minors: exploring the predictive utility of depression and anxiety symptoms. J Clin Child Adolesc Psychol. 2011;40(5):742–755. doi: 10.1080/15374416.2011.597083. [DOI] [PubMed] [Google Scholar]
- 26.Ribbe K., Friedrichs H., Begemann M. The cross-sectional GRAS sample: a comprehensive phenotypical data collection of schizophrenic patients. BMC Psychiatry. 2010;10:91. doi: 10.1186/1471-244X-10-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kay S.R., Fiszbein A., Opler L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 28.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Montgomery S.A., Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(4):382–389. doi: 10.1192/bjp.134.4.382. [DOI] [PubMed] [Google Scholar]
- 30.Bernstein D.P., Ahluvalia T., Pogge D., Handelsman L. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. 1997;36(3):340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- 31.American Psychiatric Association . 4th ed., Text Revision. Author; Washington, DC: 2000. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 32.Clinical Global Impressions . In: ECDEU assessment manual for psychopharmacology. Guy W., editor. US Department of Health, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration; Rockville, MD: 1976. [Google Scholar]
- 33.Horn W. 2 ed. Hogrefe; Göttingen: 1983. L-P-S Leistungsprüfsystem. [Google Scholar]
- 34.Mitjans M., Seidel J., Begemann M. Violent aggression predicted by multiple pre-adult environmental hits. Mol Psychiatry. 2019;24(10):1549–1564. doi: 10.1038/s41380-018-0043-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rey A. University Press of France; Paris: 1964. The clinical examination in psychology. [Google Scholar]
- 36.Harris S., Dykxhoorn J., Hollander A.C., Dalman C., Kirkbride J.B. Substance use disorders in refugee and migrant groups in Sweden: a nationwide cohort study of 1.2 million people. PLoS Med. 2019;16(11) doi: 10.1371/journal.pmed.1002944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McMahon E.M., Corcoran P., Keeley H. Mental health difficulties and suicidal behaviours among young migrants: multicentre study of European adolescents. BJPsych Open. 2017;3(6):291–299. doi: 10.1192/bjpo.bp.117.005322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Korosi A., Naninck E.F., Oomen C.A. Early-life stress mediated modulation of adult neurogenesis and behavior. Behav Brain Res. 2012;227(2):400–409. doi: 10.1016/j.bbr.2011.07.037. [DOI] [PubMed] [Google Scholar]
- 39.Nave K.A., Ehrenreich H. Myelination and oligodendrocyte functions in psychiatric diseases. JAMA Psychiatry. 2014;71(5):582–584. doi: 10.1001/jamapsychiatry.2014.189. [DOI] [PubMed] [Google Scholar]