Abstract
Objectives
The aim of this study was to increase the knowledge level of community pharmacists in Croatia to identify and resolve drug-related problems (DRPs).
Design
Before/after survey study.
Setting
University of Split School of Medicine.
Participants
115 community pharmacists from all over the Croatia.
Interventions
An interactive 3-day clinical pharmacy workshop with the goal of increasing the knowledge level of community pharmacists in Croatia to identify and resolve DRPs in routine practice. Teaching methods were based on interactive clinical case solving.
Outcome measure
Change of the community pharmacists’ knowledge based on preworkshop and postworkshop evaluation. A survey-based clinical knowledge measurement tool was used in order to evaluate the efficacy of the workshop. The lowest possible total score was 0 and the highest was 80. A higher survey score indicates a higher level of clinical knowledge to identify and resolve DRPs.
Results
Participating pharmacists had significantly higher postworkshop mean survey score (49.1±8.0) than the preworkshop mean survey score (42.9±8.2), with the mean score difference of 6.2 (95% CI 4.3 to 8.1). Furthermore, it was found that community pharmacists significantly increased their survey scores, regardless of their age.
Conclusions
Interactive and case-based clinical pharmacy workshop could be a valuable tool to increase the knowledge of community pharmacists about identification and management of DRPs in routine practice. However, further studies are necessary to evaluate the long-term knowledge maintenance and the improvement in patients’ clinical outcomes.
Keywords: education & training (see medical education & training), therapeutics, primary care
Strengths and limitations of this study.
This study included 115 community pharmacists from all over the country, and out of them 88 completed the survey both times, which is about 4% of all community pharmacists in Croatia.
Educational intervention was interactive and case based, and a survey-based clinical knowledge measurement tool was validated previously and successfully used in Australia.
Follow-up evaluations are needed in order to evaluate the long-term efficacy of the educational intervention.
The participation was voluntary and this could compromise the representativeness of the sample.
Introduction
Drug-related problems (DRPs) represent a public health problem, both in terms of patient outcomes and healthcare expenditures, as they can ultimately lead to drug-related complications, such as drug-related morbidity or mortality. Community pharmacists, as contributors to patient care, should assess data concerning untoward effects of drugs and be well skilled to recognise and prevent these drug-related complications, which result from unidentified or unresolved DRPs.1 2 The pharmaceutical care concept, as one of the pillars of modern pharmacy services, assumes clinical interventions which lead to optimal health outcomes. Identification, prevention or resolution of DRPs improve patient’s health outcomes, and therefore it should be integrated within pharmaceutical care.3 4 However, community pharmacists must have the extensive clinical knowledge and the sufficient training in order to identify and resolve DRPs. Therefore, knowledge and training are important prerequisites to efficiently provide pharmaceutical care.5–9
In our previous study, it was suggested that the additional education of community pharmacists in Croatia is associated with the higher level of clinical knowledge to detect and resolve DRPs (β=0.272, p<0.001).10 It was concluded that the additional education could increase the community pharmacists’ knowledge level and thus probably make pharmaceutical care implementation more effective. Furthermore, using the same knowledge measurement tool, it was found that community pharmacists from Australia compared with the colleagues from Croatia seem to have a higher level of clinical knowledge to detect and resolve DRPs.11 This finding indicated a general need for the improvement in the knowledge level of community pharmacists in Croatia. This was not an unexpected finding, since clinical pharmacy and pharmaceutical care models are still in the initial stages of development in Croatia. First, Centre for Applied Pharmacy was established at the University of Zagreb Faculty of Pharmacy and Biochemistry in 2004. Afterwards, clinical pharmacy was the first subject to be introduced to the revised pharmacy curricula. Patient-oriented subjects such as pharmacotherapy, communication skills, pharmacy practice and pharmaceutical care were introduced between 2006 and 2009.12 At that time, University of Zagreb Faculty of Pharmacy and Biochemistry was the only faculty for education of pharmacists in Croatia. Consequently, the majority of today’s practicing community pharmacists did not attend courses on these disciplines as a part of their graduate education due to the unavailability of such courses. Furthermore, the most of available education for licensed community pharmacists was aimed at promoting the products and consequently was without significant benefits to pharmacists’ knowledge about DRPs.
Previously, Meštrović et al also identified that community pharmacists in Croatia lack skills in the areas of monitoring drug therapy, patient consultation and the evaluation of outcomes, and that they believe they need to complete supplemental educational programmes to be able to efficiently provide pharmaceutical care.13
Therefore, there seems to be a need for an additional education programme that could fill the gap in community pharmacists’ knowledge about DRPs, and presumably improve patients’ health outcomes. Highly interactive and multifaceted learning methods, such as workshops, are reported to be highly effective strategies to improve knowledge, professional practice and healthcare outcomes.14–17 Furthermore, continuing education programmes in the form of an educational workshop have shown to improve community pharmacists’ knowledge and clinical skills in practice.5 12 18–20 Hence, we planned an educational intervention in the form of a workshop with the goal of improving the clinical knowledge level of community pharmacists in Croatia.
Methods
Workshop setting
A 3-day clinical pharmacy workshop for community pharmacists in Croatia was organised. Workshop was advertised nationwide, with the help of Croatian Chamber of Pharmacists and Croatian Pharmaceutical Society. Participation was voluntary and community pharmacists from all over Croatia participated. The workshop lasted for a total of 20 hours, and during that time various topics in the area of clinical pharmacy and pharmacotherapy were discussed, as shown in table 1.
Table 1.
Curriculum of the workshop
| Topic | Teaching hours (n) | Main teaching method |
| Pharmaceutical care in practice | 1 | Formal lectures |
| Rational pharmacotherapy and drug-related problems | 1 | Formal lectures |
| Clinical pharmacy and evidence-based medicine | 1 | Formal lectures |
| Routine laboratory tests | 1.5 | Clinical case solving |
| Food and drug interactions | 1 | Clinical case solving |
| Pharmacokinetic and pharmacodynamic interactions | 1 | Clinical case solving |
| Hormone therapy | 1.5 | Clinical case solving |
| Psychotropic drugs and antidepressants | 1.5 | Clinical case solving |
| Antimicrobial drugs | 1.5 | Clinical case solving |
| Rare diseases | 1.5 | Clinical case solving |
| Hypertension and anticoagulants | 1 | Clinical case solving |
| Dyslipidaemia and diabetes | 1 | Clinical case solving |
| Narrow therapeutic index drugs | 1.5 | Clinical case solving |
| Medication errors | 2 | Clinical case solving |
| Priority assessment in pharmacotherapy | 2 | Clinical case solving |
The workshop was held in a lecture hall at University of Split School of Medicine with the help of assistants and pharmacy students. They supervised all participants during the workshop, and participants who did not attend all sessions were considered to have dropped out from the study. A pharmacist and a pharmacologist were trainers who prepared and presented workshop materials and discussions. Both trainers have appropriate education and qualifications, for example, the pharmacist is a competency development manager and lecturer of pharmaceutical care with a PhD and ambulatory care specialisation from American College of Clinical Pharmacy and the pharmacologist is a professor of pharmacology and clinical pharmacy at University of Split School of Medicine. Furthermore, key elements of an effective educational activity, like formal lectures and interactive clinical case solving and exercises, were incorporated into the programme. The workshop was designed to provide a brief overview about each topic, but then clinical cases were solved and discussed for the most of the workshop time. Cases were prepared according to the clinical case models available in the literature.21 22 By lifting the letter card, each participant had to answer for which of the four statements in each case he thought was the most correct. After all participants had revealed their answers, discussion on each statement followed. Participants were also invited to present a few of their own cases from routine practice. From 150 clinical cases, one of the most important learning objectives was increasing the knowledge through the identification and resolution of DRPs in the presented cases. Other learning objectives included developing skill of a decision-making process in routine practice, priority assessment in pharmacotherapy and general introduction to the concept of pharmaceutical care.
Evaluation of the workshop efficacy
In order to assess the level of the clinical knowledge of participating community pharmacists preworkshop and postworkshop, we used a validated survey-based clinical knowledge measurement tool developed by Williams et al11 (online supplementary file 1, survey). Also, the same tool was used in a cross-sectional study with the aim of determining the clinical knowledge level of community pharmacists in Croatia to identify, evaluate and resolve DRPs, as it was previously reported.10 The survey was structured on nine clinical cases with a total of 40 statements. Clinical cases were based on scenarios that were found to occur frequently in community pharmacies in Australia. Each clinical case was supposed to assess a pharmacist’s ability to identify, resolve and evaluate a DRP. The survey was originally validated in Australia, and only validation verification has been carried out in Croatia. Since the same clinical cases with the same DRPs can be routinely found in Croatian community pharmacy practice, authors agreed that the survey was transferable and appropriate for use in Croatia. Therefore, survey was translated to Croatian, and afterwards to confirm the validity of translation, the back translation from Croatian to English was carried out by a fluent English speaker and experienced biomedical scientist, blinded to the study details and the original wording. The survey was composed in a manner that all participants were asked to read short case scenarios and select how relevant, likely or appropriate they found each of the proposed statements using a seven-point Likert scale. In the first three clinical cases, each statement was about additional information that would be relevant to acquire for that case, while the next three cases consisted of statements which described potential DRPs in each case and the final three cases consisted of statements about possible recommendations for the patients. Since the clinical cases were supposed to assess pharmacists’ ability to manage DRPs, the type of knowledge that was measured is mostly procedural knowledge, as it includes decision-making and problem-solving in routine practice. However, to be able to effectively perform these procedures in practice, pharmacists’ procedural knowledge must be based on extensive declarative knowledge.
bmjopen-2019-034674supp001.pdf (143.3KB, pdf)
All participating community pharmacists were invited on-site to independently complete the survey twice: at the beginning of the workshop and 3 days later at the end of the last session of the workshop. Participating pharmacists were supervised to complete the survey independently and without access to additional resources or literature. The survey was anonymous, providing only the participant’s age, gender and a simple code to match the participants’ results before and after the workshop. Study size calculation was not applicable because survey score difference which is associated with significant changes in routine practice is still not known. Therefore, all participating pharmacists were included in this study, except pharmacists who participated in the previous nationwide cross-sectional study, which was the only exclusion criteria.10
Data collection and statistical analysis
Afterwards, all data were collected in a Microsoft Excel worksheet (V.15) and each completed survey was evaluated and scored (online supplementary file 2, dataset). All statements were scored individually and each statement received a score of 2, 1 or 0 depending how far away the answer was from the correct answer. The lowest possible total score was 0 and the maximum possible 80. A higher score indicates a higher level of clinical knowledge to detect, evaluate and resolve DRPs, as previously described.11
bmjopen-2019-034674supp002.pdf (169.6KB, pdf)
Statistical calculations and analyses of the data were performed using the IBM SPSS statistical package (V.20). The graphical figure was prepared with the GraphPad Prism software (V.6, La Jolla, California, USA). Mean scores of the study participants were analysed with the independent samples and paired samples t-test. Normality of data was checked with the Kolmogorov-Smirnov and the Shapiro-Wilk tests. Pearson’s correlation was used to correlate pharmacist’s score with age. For all tests, a p<0.05 was considered to be statistically significant. All values are presented as mean±SD.
Aim of the study
The aim of this study was to increase the knowledge level of community pharmacists in Croatia to identify and resolve DRPs. Primary research outcome was the change of the community pharmacists’ knowledge based on preworkshop and postworkshop evaluation. In addition, age and gender subgroup analysis was performed.
Patient and public involvement
No patients were involved in the design, recruitment and conduct of the study. The study participants voluntarily accepted to participate in this study, and they were familiarised with all the risks and benefits. They accepted the possibility that results of the study could be published.
Results
Overall, 115 community pharmacists attended the workshop, 9 were excluded due to having previously completed the survey and in total 88 pharmacists completed the survey both times. This represents about 4% of all community pharmacists in Croatia.23 The response rate, as shown in table 2, was satisfactory because participation was voluntary and some participants dropped out before the end of the workshop. Matching method with the simple code was effective, which resulted in the successful matching of study participants for further data extraction and evaluation.
Table 2.
Demographics of the matched study participants
| Community pharmacists | |
| Age (mean±SD) | 36.6±9.2 |
| Female (%) | 90.9 |
| Male (%) | 9.1 |
| Response rate (%) | 83.0 |
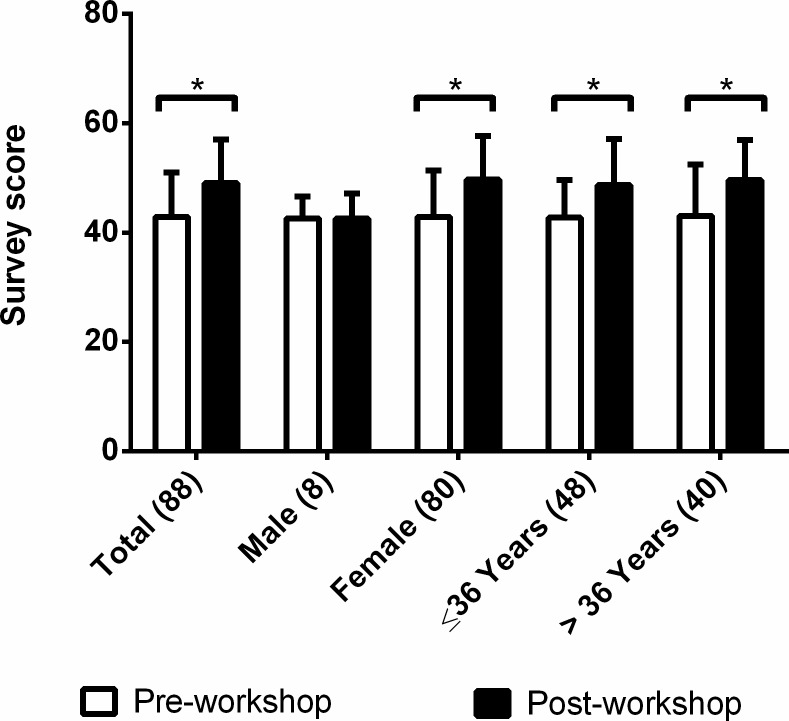
Participating pharmacists had a preworkshop mean score of 42.9±8.2, and postworkshop mean score of 49.1±8.0, as presented in figure 1. The mean score difference of 6.2±9.0, which represents a 14.5% relative increase, was found to be significant with the paired samples t-test (t=6.488, p<0.001).
Figure 1.
Preworkshop and postworkshop survey scores of participating community pharmacists by age and gender subgroups. All values are presented as mean±SD. Statistically significant differences between preworkshop and postworkshop scores are marked with a * symbol (paired samples t-test, p<0.001). Median age of the study participants is 36 years. The number of participants in each subgroup is specified in parentheses.
Furthermore, male pharmacists had a preworkshop mean score of 42.6±4.2, while female pharmacists had a preworkshop mean score of 42.9±8.5, with no significant difference between the scores with the independent samples t-test (t=−0.09, p=0.93). However, after the workshop, only female pharmacists significantly increased their mean score (paired samples t-test, t=6.744, p<0.001), with the mean score difference of 6.9±9.1.
Pharmacists in both age subgroups significantly increased their mean scores after the workshop (paired samples t-test, t=4.786, t=4.342, p<0.001) with nearly the same improvement, as presented in figure 1. Interestingly, there was no significant difference in the survey scores between age subgroups and we found no correlation between pharmacists’ survey scores and their age (Pearson’s r=0.009, n=88, p=0.933).
Discussion
The intensive 3-day educational workshop on clinical pharmacy seemed to significantly increase the clinical knowledge of community pharmacists in Croatia to detect and resolve DRPs. This finding implies that an intensive case-based educational intervention could potentially fill the gap in community pharmacists’ knowledge about DRPs.
From similar studies, Currie et al proved that the intensive educational programme in pharmaceutical care skills and implementation of these skills in practice successfully increased the rate of identified DRPs.24 They used the 40-hour training programme in two parts with the focus on the improvement of problem-solving and communication skills. Their training programme did not include clinical pharmacy topics and was solely focused on pharmaceutical care. In addition, Currie et al evaluated the impact of an educational intervention directly on patients and found that education of pharmacists in pharmaceutical care improves patient outcomes through identification of DRPs. Kimberlin et al reported that pharmacists who engaged in an educational intervention programme more likely assessed DRPs than pharmacists without the educational intervention and this difference held in the 3-month follow-up period.25 Their training programme included day-long workshop and home study using a training manual. Furthermore, they evaluated the effectiveness of an intervention by interviewing the patients which indicates better outcomes in routine pharmacy practice. In contrast to this study, results of Kimberlin et al study are based on elderly patients. Furthermore, recently Lalonde et al demonstrated that having provided community pharmacists with a short disease-specific training and essential clinical information successfully increased pharmacists’ knowledge and clinical skills as well as reduced DRP frequency in community pharmacy practice.26 Lalonde et al used short 90 min interactive web-based training programme on use of medications in chronic kidney disease. Pharmacists in their study completed self-administered questionnaire 12 months later, which showed that pharmacists improved knowledge by 4.5% and clinical skills by 7.4%. Compared with this study, it is a smaller relative knowledge increase; however, it is maintained a year after educational intervention. According to the Obreli-Neto et al, the majority of continuing education programmes were reported to be effective based on the studies’ outcome measures.27 It is therefore difficult to compare study results without standardisation of outcome measures. Also, studies with similar duration of training and evaluation of participants reported heterogeneous relative knowledge increasement, which ranged from 19% to higher or even 5%, as satisfying.28 29
Interestingly, this study also implies that community pharmacists’ age does not correlate with their clinical knowledge of detecting and resolving DRPs, while Meštrović et al study in the community pharmacy setting in Croatia revealed that the age of participants, presumably through experience, improved competency for recognising and identifying DRPs.12 However, the two studies used different tools to assess the pharmacist’s ability to manage DRPs, and one study primarily evaluated knowledge while the other study evaluated competency, which further involves skills and attitudes of participants. Competency is the ability of pharmacist to make deliberate choices for handling situations and tasks in professional pharmacy practice by using and integrating knowledge and personal values.30 Assessment of attitudes, skills and personal values requires more sophisticated evaluation methods, for example, direct observations and objective structured clinical examinations. Therefore, it is possible that age of pharmacists through experience in practice impacts mostly skills, attitudes and personal values of community pharmacists. As opposed to, pharmacists’ knowledge could stagnate over time, especially if it is not renewed with continuous education. This could be the reason for the different findings between the studies, but further research is required in order to clarify this difference. Also, it is interesting that there was no significant difference in the survey scores between age subgroups. It could have been expected that the participants in the younger subgroup should have higher survey scores, considering that this subgroup included pharmacists who studied after the revision of pharmacy curricula. However, first generations of pharmacists who studied under revised programme have started working 5–6 years later, including the obligatory internship; therefore, it is very likely that their number was not large enough to detect differences between subgroups. It should be further investigated in the future to verify if the curricular revision led to an improvement in pharmacists’ knowledge about DRPs.
Furthermore, it was found that after the workshop only female pharmacists significantly improved their clinical knowledge about DRPs, while male pharmacists retained the same level of knowledge as before the workshop. This potentially could be due to a greater emphasis on pharmaceutical care which as a topic could be more appealing to female pharmacists.31 However, it is also possible that a small number of male participants (n=8) were not sufficient to show statistical significance, and therefore this finding is questionable and should be further investigated.
Surprisingly, even after the workshop, the overall survey scores were also lower than the scores from the original study in Australia.11 Survey was based on clinical cases and DRPs which are relevant in Australian community pharmacy setting. However, the same cases with the same DRPs can be routinely found in Croatian community pharmacy practice, so this could not be the reason for such a difference. As mentioned, this most probably arises from different educational backgrounds and different role of community pharmacists in healthcare systems.10 Community pharmacists in Croatia are still mostly oriented on traditional pharmacy services like dispensing and supplying of medicines, while additional services, which could expand their role as healthcare providers, are not available in practice. It is only in the last few years that work has begun to introduce advanced services, like medication review in pharmacy practice. Furthermore, preworkshop survey scores were also lower than scores in previous nationwide study.10 However, pharmacists who participated in previous nationwide study were excluded and the only relation with this study is that previous study revealed community pharmacists’ general lack of knowledge about DRPs. Also, in previous study, participants were community pharmacists from large pharmacy chains while this study presumably included more pharmacists who believed that they lack knowledge in this area, since the participation was voluntary. Authors of the workshop expected this since they knew about community pharmacists’ general lack of knowledge about DRPs. Therefore, they decided to use the same survey to evaluate the efficacy of educational intervention.
A major limitation of this study is the fact that postworkshop clinical knowledge scores were evaluated only immediately after the workshop, so these results actually represent short-term knowledge gain and are therefore not reflective of any sustained improvement in knowledge. However, patient benefits must be continuous and not limited to certain periods of time. As expected, a majority of studies have also confirmed that training programmes increase the knowledge of pharmacists immediately after the educational intervention, and only a few studies revealed that these improvements could be maintained for a year or even longer without any further education.7 26 Therefore, follow-up evaluations are needed and these results should be supported by conducting a future survey to determine whether improvements were maintained and to further evaluate the efficacy of the educational intervention.
Another limitation is the possibility of overestimating the results to the general community pharmacist population since the workshop participation was only voluntary. It is therefore possible that only more motivated and enthusiastic pharmacists attended and thus had a greater improvement in knowledge. It is also possible that any prior training of pharmacists could have impacted the pharmacists’ knowledge, although this was the first large-scale educational intervention with the goal of increasing knowledge about DRPs in Croatia. Most of the trainings that pharmacists have previously had were in the form of lifelong learning with various topics from pharmacy practice and were not specifically focused on improving knowledge about DRPs. Therefore, since community pharmacists in Croatia have not previously received any training of this type and there were no pharmacists who have completed postgraduate studies, this was probably not a limitation. Also, since study participants were from all over the country and represent both the small privately owned pharmacies and the large pharmacy chains and participants gender distribution is representative of Croatian community pharmacists population, generalisation of these results to the community pharmacy setting is much more applicable.32 33
Finally, this study once more confirms previously reported findings that educational interventions through workshops are a useful tool to successfully improve pharmacists’ knowledge on various topics in pharmacy practice.7 19 34 35 Educational interventions can play a vital role in expanding basic pharmacy education and enhancing pharmaceutical care implementation, especially when insufficient training has been received during undergraduate or graduate studies.36 However, to evaluate the true relevance of these findings for community pharmacy practice, it is still necessary to find out if the increased clinical knowledge level of community pharmacists will result in an increased level of clinical interventions about DRPs in daily practice. For example, one of the clear indicators would be the number of reported adverse drug reactions or documented clinical interventions in this group of pharmacists. If confirmed, these findings could have an important implication for pharmacists’ continuing education about DRPs.
Conclusions
The interactive and intensive educational intervention through the 3-day clinical pharmacy workshop seems to improve the community pharmacists’ knowledge to identify, evaluate and resolve DRPs in a simulated routine practice setting. Therefore, educational interventions could be a valuable tool to fill the gap in pharmacist’s knowledge about DRP management. Further studies are necessary in order to evaluate long-term knowledge maintenance and the impact of these findings in community pharmacy practice.
Supplementary Material
Acknowledgments
The authors are grateful to all participating community pharmacists for making this study possible and to Shelly Pranic for proofreading this paper.
Footnotes
Contributors: DM was the leader of this research. LZ interpreted and analysed the study data. LZ, AM and DM participated in the workshop preparation. ASP, JB, DL and DR participated in conducting the survey. All authors participated in preparation and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: LZ is employed by Split-Dalmatia County Pharmacy and Arijana Mestrovic is employed by Pharmaexpert LLC.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the University of Split School of Medicine Ethics Committee (003-08/15-03/0001) and each participant consented verbally to participate in the study, as approved by the ethics committee. Verbal consent was considered to be appropriate because of the favourable risk/benefit ratio for the participants. The intervention was educational and the assessment tool was the written survey so there were no particular risks for the study participants.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1.Westerlund T, Marklund B. Assessment of the clinical and economic outcomes of pharmacy interventions in drug-related problems. J Clin Pharm Ther 2009;34:319–27. 10.1111/j.1365-2710.2008.01017.x [DOI] [PubMed] [Google Scholar]
- 2.Kovačević SV, Miljković B, Ćulafić M, et al. Evaluation of drug-related problems in older polypharmacy primary care patients. J Eval Clin Pract 2017;23:860–5. 10.1111/jep.12737 [DOI] [PubMed] [Google Scholar]
- 3.Allemann SS, van Mil JWF, Botermann L, et al. Pharmaceutical care: the PCNE definition 2013. Int J Clin Pharm 2014;36:544–55. 10.1007/s11096-014-9933-x [DOI] [PubMed] [Google Scholar]
- 4.Cousins D, Kijlstra N, Walser S. Pharmaceutical Care – Policies and Practices for a Safer, More Responsible and Cost-effective Health System: European Directorate for the Quality of Medicines & HealthCare, EDQM, Council of Europe, 2012. Available: https://www.edqm.eu/medias/fichiers/policies_and_practices_for_a_safer_more_responsibl.pdf
- 5.Mehra llaV, Wuller CA. Evaluation of a pilot clinical skills workshop series for community pharmacists. Am J Pharm Educ 1998;62. [Google Scholar]
- 6.Bindoff I, Ling T, Bereznicki L, et al. A computer simulation of community pharmacy practice for educational use. Am J Pharm Educ 2014;78:168. 10.5688/ajpe789168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Basheti IA, Armour CL, Reddel HK, et al. Long-term maintenance of pharmacists' inhaler technique demonstration skills. Am J Pharm Educ 2009;73:32. 10.5688/aj730232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Westerlund T, Almarsdóttir AB, Melander A. Factors influencing the detection rate of drug-related problems in community pharmacy. Pharm World Sci 1999;21:245–50. 10.1023/A:1008767406692 [DOI] [PubMed] [Google Scholar]
- 9.Lamsam GD, Kropff MA. Community pharmacists' assessments and recommendations for treatment in four case scenarios. Ann Pharmacother 1998;32:409–16. 10.1345/aph.17287 [DOI] [PubMed] [Google Scholar]
- 10.Zekan L, Mestrovic A, Seselja Perisin A, et al. Clinical knowledge of community pharmacists in Croatia for detecting drug-related problems. Int J Clin Pharm 2017;39:1171–4. 10.1007/s11096-017-0546-z [DOI] [PubMed] [Google Scholar]
- 11.Williams M, Peterson GM, Tenni PC, et al. A clinical knowledge measurement tool to assess the ability of community pharmacists to detect drug-related problems. Int J Pharm Pract 2012;20:238–48. 10.1111/j.2042-7174.2012.00188.x [DOI] [PubMed] [Google Scholar]
- 12.Meštrović A, Staničić Z, Hadžiabdić MO, et al. Individualized education and competency development of Croatian community pharmacists using the general level framework. Am J Pharm Educ 2012;76:23. 10.5688/ajpe76223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meštrović A, Staničić Z, Hadžiabdić MO, et al. Evaluation of Croatian community pharmacists' patient care competencies using the general level framework. Am J Pharm Educ 2011;75:36. 10.5688/ajpe75236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roque F, Herdeiro MT, Soares S, et al. Educational interventions to improve prescription and dispensing of antibiotics: a systematic review. BMC Public Health 2014;14:1276. 10.1186/1471-2458-14-1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pagotto C, Varallo F, Mastroianni P. Impact of educational interventions on adverse drug events reporting. Int J Technol Assess Health Care 2013;29:410–7. 10.1017/S0266462313000457 [DOI] [PubMed] [Google Scholar]
- 16.Bellolio MF, Stead LG. Evidence-based emergency medicine/systematic review abstract. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Ann Emerg Med 2009;53:685–7. 10.1016/j.annemergmed.2008.05.034 [DOI] [PubMed] [Google Scholar]
- 17.Davis D, O'Brien MA, Freemantle N, et al. Impact of formal continuing medical education: do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA 1999;282:867–74. 10.1001/jama.282.9.867 [DOI] [PubMed] [Google Scholar]
- 18.Villeneuve J, Lamarre D, Lussier M-T, et al. Physician-pharmacist collaborative care for dyslipidemia patients: knowledge and skills of community pharmacists. J Contin Educ Health Prof 2009;29:201–8. 10.1002/chp.20038 [DOI] [PubMed] [Google Scholar]
- 19.Abdel Shaheed C, Maher CG, Mak W, et al. The effects of educational interventions on pharmacists' knowledge, attitudes and beliefs towards low back pain. Int J Clin Pharm 2015;37:616–25. 10.1007/s11096-015-0112-5 [DOI] [PubMed] [Google Scholar]
- 20.Connolly M, Rutter V, Cardiff L. Evaluation of workshop-based peer review training to support pharmacist professional development. Pharm Educ 2016;16:92–4. [Google Scholar]
- 21.Dhillon S, Raymond R. Pharmacy case studies. London: Pharmaceutical Press, 2009. [Google Scholar]
- 22.Dodds LJ. Drugs in use : clinical case studies for pharmacists. 4th edn London, Chicago: Pharmaceutical Press, 2010. [Google Scholar]
- 23.Ministarstvo Zdravlja National health care strategy 2012-2020. Zagreb: Ministry of health of the Republic of Croatia, 2012. [Google Scholar]
- 24.Currie JD, Chrischilles EA, Kuehl AK, et al. Effect of a training program on community pharmacists' detection of and intervention in drug-related problems. J Am Pharm Assoc 1997;NS37:182–91. 10.1016/S1086-5802(16)30203-0 [DOI] [PubMed] [Google Scholar]
- 25.Kimberlin CL, Berardo DH, Pendergast JF, et al. Effects of an education program for community pharmacists on detecting drug-related problems in elderly patients. Med Care 1993;31:451–68. 10.1097/00005650-199305000-00007 [DOI] [PubMed] [Google Scholar]
- 26.Lalonde L, Quintana-Bárcena P, Lord A, et al. Community pharmacist Training-and-Communication network and drug-related problems in patients with CKD: a multicenter, cluster-randomized, controlled trial. Am J Kidney Dis 2017;70:386–96. 10.1053/j.ajkd.2017.05.008 [DOI] [PubMed] [Google Scholar]
- 27.Obreli-Neto PR, Marques Dos Reis T, Guidoni CM, et al. A systematic review of the effects of continuing education programs on providing clinical community pharmacy services. Am J Pharm Educ 2016;80:88. 10.5688/ajpe80588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Minh PD, Huong DTM, Byrkit R, et al. Strengthening pharmacy practice in Vietnam: findings of a training intervention study. Trop Med Int Health 2013;18:426–34. 10.1111/tmi.12062 [DOI] [PubMed] [Google Scholar]
- 29.Chiang Y-C, Lee C-N, Lin Y-M, et al. Impact of a continuing education program on pharmacists' knowledge and attitudes toward asthma patient care. Med Princ Pract 2010;19:305–11. 10.1159/000312718 [DOI] [PubMed] [Google Scholar]
- 30.Govaerts MJB. Educational competencies or education for professional competence? Med Educ 2008;42:234–6. 10.1111/j.1365-2923.2007.03001.x [DOI] [PubMed] [Google Scholar]
- 31.International Pharmaceutical Federation Global pharmacy workforce report, 2009. Available: http://fip.org/files/fip/publications/2009_FIP_Global_Pharmacy_Workforce_Report.pdf
- 32.Croatian Chamber of Pharmacists Register of pharmacists. Zagreb: Croatian Chamber of Pharmacists, 2020. http://www.hljk.hr/Registri/RegistarljekarnikauRH/tabid/68/Default.aspx [Google Scholar]
- 33.International Pharmaceutical Federation Global pharmacy workforce report, 2012. Available: https://www.fip.org/file/1414
- 34.Elkalmi RM, Hassali MA, Ibrahim MIM. Impact of educational intervention for improving pharmacist knowledge in adverse drug reactions (ADR) reporting: experience from Malaysia. Open Drug Saf J 2011;2:47–53. 10.2174/1876818001102010047 [DOI] [Google Scholar]
- 35.Austin Z, Marini A, MacLeod Glover N, et al. Peer-mentoring workshop for continuous professional development. Am J Pharm Educ 2006;70:117. 10.5688/aj7005117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.International Pharmaceutical Federation Global pharmacy workforce and migration report, 2006. Available: http://fip.org/files/fip/publications/PharmacyWorkforceMigration.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-034674supp001.pdf (143.3KB, pdf)
bmjopen-2019-034674supp002.pdf (169.6KB, pdf)