Abstract
The optimal management and long-term outcomes of olecranon fractures in the paediatric population is not well understood. This systematic review aims to analyse the literature on the management of paediatric olecranon fractures and the long-term implications.
A systematic review of several databases was conducted according to PRISMA guidelines. English-language studies evaluating the management of isolated paediatric olecranon fractures were included. Data extracted included demographics, classifications, conservative and operative treatment methods and outcomes.
Fifteen articles fitting the inclusion criteria were included. There were 11 case series and four retrospective comparative series. The reported studies included 299 fractures in 280 patients.
The mechanism of injury was predominantly low energy. Fractures displaced < 4 mm were treated non-operatively with almost universally good results, with the majority being treated with cast immobilization. Fractures displaced > 4 mm were commonly treated operatively with generally good results, with tension band wire and suture fixation being the most common treatment modalities. Weight > 50 kg was associated with failure of suture fixation.
In those studies that reported olecranon fractures with associated elbow injuries (e.g. radial head fractures) outcomes were poorer. Forty-six fractures were in patients with osteogenesis imperfecta, who sustained a higher rate of re-fracture after removal of metalwork and contralateral olecranon fracture.
Despite a relatively low evidence base pool of studies, the aggregate data support the non-operative treatment of isolated undisplaced olecranon fractures with good results, and support the operative treatment of fractures displaced ≥ 4 mm.
Cite this article: EFORT Open Rev 2020;5:280-288. DOI: 10.1302/2058-5241.5.190082
Keywords: fracture, olecranon, paediatric
Introduction
Olecranon fractures account for 4% of all paediatric elbow fractures, and are associated with other ipsilateral elbow injuries up to 20% of the time, which in turn are associated with poorer outcomes.1 In adults, olecranon fractures are more common, representing 10% of all elbow fractures.2
The surgical indications in adult patients have been well studied, with only patients with truly undisplaced fractures (Mayo Type I), patients unfit for surgery, or elderly patients being treated non-operatively.3–5 Those being treated operatively are typically treated with either tension band techniques, or plate fixation.5 Surgical indications in paediatric patients, however, are less clear, and often confusion arises as to the optimal surgical technique to employ in the growing skeleton across an open physis in this population. The long-term implications of an olecranon fracture involving the physis and surgical hardware such as wires potentially crossing the physis are also unclear.
This systematic review aims to provide a concise update on the literature of isolated paediatric olecranon fractures, summarizing surgical indications, treatment options and expected outcomes.
Materials and methods
Search strategy
We conducted an online systematic literature search in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. It was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO; CRD42019122459).
PubMed, MEDLINE, EMBASE and The Cochrane Library were searched in December 2018 using the terms “olecranon”, “fracture”, “p(a)ediatric or child(ren)”. Our search was not limited by year of publication, journal type, or level of evidence. All bibliographies of included articles were checked for further relevant studies.
Eligibility criteria
The inclusion criteria were: any original article (all levels of evidence); children < 18 years old with isolated olecranon fractures; English-language articles. The exclusion criteria were: case reports; review articles/basic science research (e.g. biomechanical studies); patients > 18 years old and studies with associated elbow injuries where it was not possible to differentiate isolated olecranon fracture data.
Two authors reviewed all abstracts for inclusion according to the above criteria, and where a study met all the criteria, or where there was uncertainty, the full texts were obtained and reviewed by both authors to assess eligibility. In cases of disagreement over study inclusion, a senior author was consulted and disagreement resolved by consensus.
Data extraction and analysis
The following data were extracted: demographics (age at time of injury, sex); mechanism of injury; associated conditions i.e. osteogenesis imperfecta (OI); fracture classification used; criteria for surgical intervention; non-operative treatment details; operative intervention details; post-operative rehabilitation protocol; length of follow up; clinical outcomes (patient/clinician reported – including pain, range of motion, time to returning to activity/sport, muscle bulk, strength, complications such as failure of fixation/revision); radiological outcomes (union, degenerative changes, apophyseal changes, deformity, loss of fixation). Risk of bias of the studies was assessed according to Murad et al6 for case series, and ROBINS-I7 for non-randomized interventional studies. This method was designed to evaluate the study design of the included articles.
Statistical analysis
All continuous data were pooled, and a descriptive data analysis performed.
Results
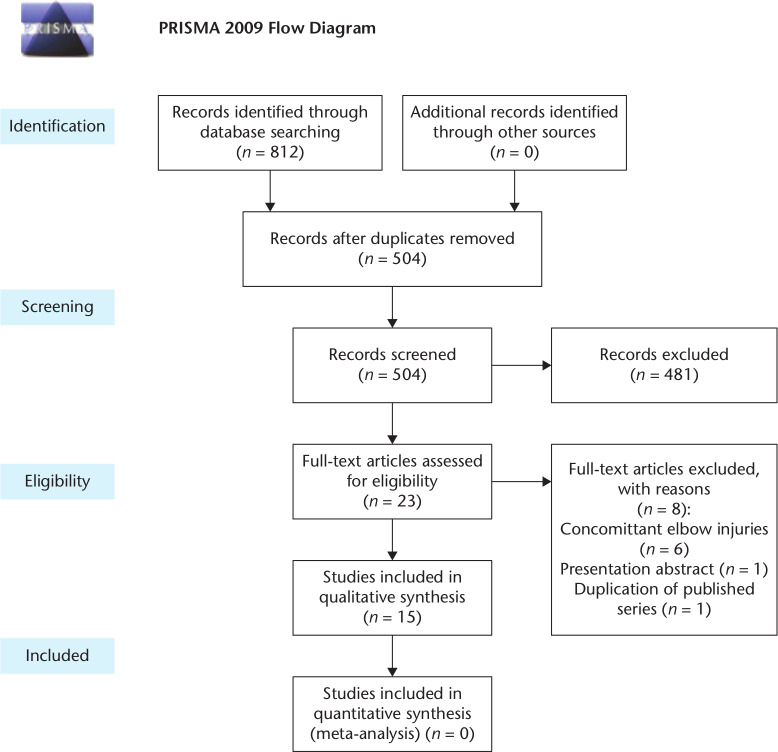
The initial literature search resulted in a total of 812 articles. Fig. 1 shows the PRISMA flowchart for study selection. A total of 15 studies met all inclusion criteria and were analysed. There were four retrospective comparative series, and 11 case series. The bias assessment for all 15 articles is shown in Appendix 1.
Fig. 1.
Flow diagram of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) process.
Patient demographics (Table 1)
Table 1.
Study/patient characteristics
| Authors | Study type | Fractures | Mean age (years) | Mechanism | Fracture classification | Indication for surgery | Mean follow up |
|---|---|---|---|---|---|---|---|
| Caterini et al15 | Case series | 23 | 7.4 | Not stated | Morphology and displacement | > 2 mm displacement | 25 years |
| Corradin et al9 | Retrospective comparative study | 22 | 10.5 | Not stated | AO PCCF | > 2 mm displacement | 18 months |
| Gaddy et al16 | Case series | 28 | 8.5 | Low energy: 29; High energy: 6 | Displacement | ≥ 3 mm displacement | 5 years |
| Gicquel et al10 | Case series | 4 | 9.9 | Not stated | Bracq | Not stated | 13 months |
| Gwynne-Jones11 | Retrospective comparative study (OI and non-OI patients) | 12 | OI: 12.1; Non-OI: 14.3 | OI: 8 low energy; Non-OI: 4 high energy | Salter Harris and displacement | Not stated | 28 months |
| Karlsson et al12 | Case series | 23 | 11.0 | Low energy: 13; High energy 10 | Horne and Tanzer and displacement | ≥ 4 mm displacement | 19 years |
| Kim et al8 | Case series | 10 | 11.7 | Not stated | AO PCCF | > 2 mm displacement or step off | 6–12 months |
| Maffulli et al32 | Case series | 12 | 13.5 | All apophysitis/overuse injuries | None | Not stated | 6 years |
| Maity et al13 | Case series | 7 | 7.3 | Not stated | Evans | > 2 mm displacement | 30 months |
| Matthews1 | Case series | 24 | Not stated | Not stated | Displacement and associated injuries | > 4 mm displacement or step off | 12 weeks to 3 years |
| Newell23 | Case series | 35 | Not stated | Low energy: 20 | None | Not stated | Not stated |
| Papavasiliou et al17 | Case series | 15 | Not stated | High energy: 15 | Intra/extra-articular | Not stated | Not stated |
| Perkins et al19 | Retrospective comparative study | 46 | 12.3 | Not stated | None | ≥ 2 mm displacement | 9 months |
| Persiani et al14 | Retrospective comparative study (OI patients) | 21 | 12.0 | Low energy: 13; High energy: 8 | Mayo | Not stated | 3 years |
| Zionts et al18 | Case series (OI patients) | 17 | 10.0 | Low energy: 14 | Morphology | Not stated | 53 months |
Note. AO PCCF, AO Pediatric Comprehensive Classification of Long-Bone Fractures; OI, osteogenesis imperfecta.
The 15 included studies contributed a total of 280 patients with 299 olecranon fractures; 46 of these fractures were in patients with OI; 68% of patients were male, with mean ages ranging from 7.3 to 13.5 years with the youngest patient being 2 months old, and the eldest 17 years old.
Follow up
In all, 13 studies reported their follow up period, ranging from 6 months to 25 years.
Mechanism of injury
Mechanism of injury was not widely reported, but of the 110 non-OI fractures where it was reported, 74 had a low-energy mechanism (e.g. fall from standing height, stress injuries) and 36 had a high-energy mechanism (e.g. fall from bicycle, motor vehicle accident). Of the 46 OI fractures, 35 fractures had a low-energy mechanism, and seven had a high-energy mechanism.
Fracture classification
Only 12 studies defined a classification system, of which seven used a previously published system (AO Paediatric Comprehensive Classification of Long-Bone Fractures (PCCF),8,9 Bracq,10 Salter-Harris,11 Horne and Tanzer,12 Evans,13 Mayo).14 Of these, the Evans system is a comprehensive paediatric olecranon specific system based upon anatomic site, fracture configuration, intra-articular displacement, and associated injuries. Bracq is a paediatric specific classification system describing the orientation of the fracture line (distal/oblique/parallel). The AO PCCF is a generic paediatric classification system based upon morphology. The Salter-Harris classification is a generic paediatric physeal classification system. The Horne and Tanzer, and Mayo systems are based upon adult fractures.
The other five studies designed their own classification systems. Caterini et al15 used morphology and displacement, Gaddy et al16 used displacement alone, Matthews1 used a combination of displacement and associated injuries, Papavasiliou et al17 used extra/intra-articular status, and Zionts and Moon18 used morphology.
Due to the wide variation in reporting of fracture type between studies it is not possible to formally aggregate the data. However, the majority of fractures seen were intra-articular with a simple split into the trochlear notch with a variety of apophyseal avulsions (younger patients), and metaphyseal fractures (older patients) with varying amounts of displacement/step off.
Indications for surgery
The indications for surgery were described in only eight studies. Five studies8,9,13,15,19 used a cut-off of 2 mm displacement, one16 used a cut-off of 3 mm, and two1,12 used a cut-off of 4 mm. Two of these studies used articular step off as well (2 mm8 and 4 mm1), but did not differentiate which cases had an articular step off or how this was evaluated.
Assessment of clinical outcomes
Five studies used recognized clinical outcome scores (Quick DASH,9 Graves and Canale,16 Mayo Elbow Performance Score (MEPS),8 Gicquel).10,13 Of these, Gicquel et al10 adapted a previously used adult scoring system to apply to the paediatric population,20 scoring three domains of pain, global function, and joint mobility on a scale out of 5 points each, combined with a radiological score out of 4 (excellent score ≥ 18, good = 17, fair = 16, and poor < 16). The Graves and Canale system21 was developed in a paediatric population describing a satisfactory outcome as having loss of elbow flexion/extension/pronation/supination of < 15 degrees and no pain with motion or infection. The Quick DASH and MEPS are adult outcome scores. The other 10 studies used a combination of pain, range of motion, strength, metalwork removal, re-fracture, residual deformities, complications and return to activity to report clinical outcomes. Of these, three studies designed their own outcome scales: Caterini et al15 graded outcomes as good, fair or poor based upon symptoms, range of motion, limb length discrepancy, muscular atrophy, neurological impairment and radiographic change in shape of the olecranon. Karlsson et al12 graded outcomes as excellent, good and severe based upon pain on loading, pain at rest, tenderness, loss of strength and range of motion compared to the uninjured elbow. Matthews1 defined a satisfactory outcome as full and painless range of motion and function.
Assessment of radiological outcomes
Two studies used a recognized radiological outcome score (Gicquel)10,13 graded out of four based upon the state of the joint space and articular surfaces. Eleven studies1,8,9,12,14-19,22 used a combination of deformity, osteoarthritis, secondary displacement, re-fracture, non-union/malunion, fracture consolidation, growth disturbances, joint space/articular surface congruity, implant loosening, and peri-articular calcification to report radiological outcomes. Two studies11,23 did not state how or whether radiological outcomes were assessed.
Conservative management (Table 2)
Table 2.
Conservative management and outcomes
| Authors | Cast | Collar and cuff or sling | Other | Clinical outcomes | Radiological outcomes |
|---|---|---|---|---|---|
| Caterini et al15 | 18 | – | – | Custom classification. Good: 18 | No evidence of OA |
| Gaddy et al16 | 18 | – | – | Graves & Canale classification – satisfactory: 18 | No evidence of growth disturbance of the olecranon apophysis |
| Karlsson et al12 | 9 | – | 3 (mobilization) | Custom classification Excellent: 12 | No non-union or elbow OA |
| Maffulli et al22 | – | – | 12 (rest, cryotherapy, physiotherapy) | Nine returned to same level of competitive gymnastics; three gave up due to other injuries | All healed uneventfully |
| Matthews1 | 8 | 16 | – | Collar and cuff 16/16 satisfied, cast 4/8 satisfied (four had temporarily restricted ROM but resolved by 24 weeks) | No non-unions |
| Newell23 | 24 | 10 | – | All regained full range of motion by 10 weeks, sling treatment had full pain-free range of motion at 3 weeks. Two treated in cast lacked 15 degrees of extension at 6 weeks but regained by 10 weeks. | Not stated |
| Papavasiliou et al17 | 10 | – | 1 (displaced fracture – mobilization as refused treatment) | Non-operative: 10 regained normal, pain-free range of motion. The one who refused treatment had 30 degrees loss of extension and 15-degree flexor lag. | Pseudoarthrosis in displaced fracture in patient refusing treatment |
Note. OA, osteoarthritis; ROM, range of motion.
Cast immobilization
Cast immobilization was used in 87 non-OI fractures across six studies. Thirty-four cases were described as ‘undisplaced’, nine cases < 4 mm displacement, eight cases ≤ 4 mm displacement, 18 cases < 3 mm displacement, and 18 cases ≤ 2 mm displacement. Of these, most were treated in a flexion cast (80–100 degrees), with the remaining in an extension cast. The duration of immobilization ranged from 2–6 weeks. When stiffness was present, it persisted for 10–24 weeks with no long-term functional limitations.1 One case developed Volkmann’s ischaemic contracture eight weeks post injury in a cast despite early operative decompression of the volar compartment.1 It is not clear how this occurred, and this does not seem to represent the overall experience in cast immobilization.
Cast immobilization was used in five OI fractures. Displacement was not defined in these cases. Of these, two went on to re-fracture, one displaced in the cast, and two went on to heal uneventfully.
Collar and cuff/sling immobilization
Twenty-six cases across two studies were treated with collar and cuff or sling immobilization. Sixteen were defined as displacement ≤ 4 mm, and the other 10 as ‘undisplaced’. Ten were described to be pain free with full range of motion by three weeks.23 In both studies a comparison between collar and cuff/sling and cast immobilization demonstrated increased rates of temporary stiffness in the cast immobilization groups. The rationale behind the decision to apply either cast immobilization or collar and cuff/sling immobilization was not specified in either study.
Other modalities
Four cases were treated with mobilization and 12 with rest, cryotherapy and physiotherapy (for overuse apophysitis) across three studies. The outcomes were universally good apart from one case in which the patient had a displaced fracture but refused any form of intervention.
Surgical management (Table 3)
Table 3.
Surgical management and outcomes
| Authors | TBW | TBS | Other | Post-op rehab | Clinical outcomes | Radiological outcomes |
|---|---|---|---|---|---|---|
| Caterini et al15 | – | – | 4 (cerclage wire), 1 (screw fixation) | Cast for 4 weeks | Good: 3/4 cerclage wires, 1/1 screw fixation Poor: 1/4 cerclage wires (inadequate intra-operative reduction) |
Severe radiographic OA in 1 treated with cerclage wires due to inadequate reduction |
| Corradin et al9 | – | 10 | 12 (screw fixation) | Cast for 4–6 weeks | All returned to previous levels of daily and sporting activity. TBS: Quick DASH 1.82, 1 case 15–20 degrees loss of extension. Screw fixation: QuickDASH 3.42, 3 cases 15–20 degrees loss of extension | All cases good reduction with < 2 mm residual displacement No adverse radiological features |
| Gaddy et al16 | 10 | – | – | Cast (1–4 weeks) then protected active-motion therapy | All satisfactory | No evidence of growth disturbance of the olecranon apophysis |
| Gicquel et al10 | – | – | 4 (Fixano screw fixation) | Cast for 3–4 weeks | Excellent (3), good (1 – imperfect reduction that had not remodelled by 17 months) Pins removed at 6–8 weeks |
Radiological – Satisfactory (3), poor (1 – persistence of displacement following surgery) |
| Gwynne-Jones11 | 4 | – | – | Cast for 3 weeks | Limited ROM (10 degrees loss of extension): 2/4 | Not stated |
| Karlsson et al12 | 2 | – | 6 (figure of eight wire), 1 (rushpin), 2 (closed reduction and casting) | Cast for 2–6 weeks (mean 4 weeks) | Excellent: 9 Good: 2 (figure of eight wires) |
No non-union or elbow OA |
| Kim et al8 | – | 10 | – | Hinged elbow brace (8 weeks). ROM exercises after 1 week | All had full ROM, 100% MEPS, and elective removal of pins under sedation at 12 weeks post-op | All had bony union with no loss of reduction or growth arrest |
| Maity et al13 | – | 7 | – | Cast for 4 weeks | Excellent in all patients, no complications Full painless range of motion within 6 months |
Excellent in all patients, no complications United within 6 weeks |
| Newell23 | – | – | 1 (soft tissue suture) | Cast for 1 month (extension) | The single operative case regained ROM 0-130 degrees by 3 months | Not stated |
| Papavasiliou et al17 | 4 | – | – | Cast for 3 weeks | All painless but with 20 degrees loss of extension | All had overgrowth of olecranon epiphysis |
| Perkins et al19 | 17 | 29 | – | Cast for 2–4 weeks | Hardware removal at 6 months (12/17 TBW, 17/29 TBS). Revision fixation at mean 23 days (1/17 TBW (plate), 4/29 TBS (1 TBW, 1 plate, 1 screw, 1 TBS). Revision group in TBS older and heavier | Union 89% (41/46) following initial surgery |
Notes. TBS, tension band suture; TBW, tension band wire; OA, osteoarthritis; Quick DASH, Disabilities of the Arm, Shoulder and Hand; ROM, range of motion; MEPS, Mayo Elbow Performance Score.
Tension band wiring (TBW)
Thirty-seven non-OI fractures were treated with TBW across five studies. Post-operative rehabilitation involved the use of either a cast or a brace for between 1–6 weeks. Hardware removal was routinely performed in one study at eight weeks17 with the other studies removing hardware on a case-by-case basis. Outcomes were mostly satisfactory, except for slightly reduced range of motion (up to 20 degrees loss of extension) in four patients, revision fixation to plate and screws in one patient, and one re-fracture (after a second injury one year post initial fixation).
Twenty OI fractures were treated with TBW. There were four cases of re-fracture after removal of metalwork, and one case of re-fracture with retained metalwork. Five patients had some restriction of movement (up to 15 degrees loss of extension).
Tension band suturing (TBS)
Fifty-six non-OI fractures were treated with TBS. Vicryl, fibrewire, and unspecified absorbable sutures were used in combination with two longitudinal K-wires. Reduced range of motion (up to 20 degrees loss of extension) was noted in one case, and revision was required for re-displacement in four cases. Failure of fixation tended to be in older children weighing over 50 kg. Metalwork was routinely removed in two studies9,13 between 1–6 months post-operatively. Other studies undertook metalwork removal on a case-by-case basis. Eight OI fractures were treated with TBS with universally good results.
Screw fixation
Screw fixation was undertaken in 17 non-OI fractures. Clinical outcome was satisfactory in all but three cases, which had reduced range of motion. Metalwork was routinely removed in two studies9,10 between 2–6 months post-operatively.
Ten OI fractures underwent screw fixation. All cases had up to 15 degrees loss of extension at three years but had no pain. Five cases required revision surgery – three for screw migration and two for re-fracture. Two were revised with screw fixation, and the other three with TBW.
Other modalities
Four cases underwent cerclage wiring, one percutaneous pin fixation, two closed reduction and in five cases the surgical treatment was not specified. In one of the cases undergoing cerclage wiring, the intra-operative reduction was inadequate, resulting in poor clinical and radiological outcomes secondary to development of OA.
OI-related fractures (Table 4)
Table 4.
Management and outcomes in patients with osteogenesis imperfecta
| Authors | Treatment | Post-op rehab | Mean follow up | Clinical outcomes | Radiological outcomes |
|---|---|---|---|---|---|
| Gwynne-Jones11 | 1 cast (undisplaced), 6 TBW (displaced), 1 plate (non-union) | Cast (3 weeks) | 28 months | Cast: no refracture, ROM not noted. TBW: all healed but 2 later refractured post metalwork removal after subsequent fall. All but one limited extension 10–15 degrees. Prominent metalwork requiring wire removal in 2 cases, and TBW removal in 3 cases. | Not stated |
| Persiani et al14 | 11 TBW, 10 Screw fixation | Hinged brace (3 weeks) | 3 years | 3 years – no pain in either group, 15-degree loss of extension in screw fixation group versus no decreased ROM in TBW group. Two screws revised to new screws, one screw revised to TBW for migration, two screws revised to TBW for re-fracture. | At 3 years, complete bone healing, no implant migration in TBW group, one migration in screw fixation group, no periarticular calcification |
| Zionts et al18 | 4 cast, 3 TBW, 8 TBS, 2 not specified | Cast (3–6 weeks) | 53 months | All clinical union by 6 weeks, nine elective removal of metalwork – two TBW cases refractured over one month post removal requiring re-operation. None had pain or limitation of function at final follow up. | All radiological union by 6 weeks. Out of seven followed to skeletal maturity, no deformity of elbow, only mild irregularity of contour of proximal portion of olecranon |
Footnotes: TBW (tension band wire), ROM (range of motion), TBS (tension band suture).
Out of 46 OI-related fractures, five were treated with cast immobilization, 20 with TBW, eight with TBS, 10 with screw fixation, one with plate fixation for a delayed diagnosis with non-union, and two were unspecified. All ultimately united; however, re-fracture occurred in four TBW cases after removal of metalwork. Two cases with screw fixation re-fractured, requiring conversion to TBW, and three cases with screw fixation had to be revised for metalwork migration. A significant number of patients suffered stiffness, lacking the last 10–15 degrees of extension.
Discussion
Isolated olecranon fractures in the paediatric population represent an uncommon injury in isolation. Whilst in adults olecranon fractures represent up to 10% of elbow injuries,2 in children they represent only around 4% of all elbow injuries and are associated with concomitant elbow injuries 20% of the time.1 Concomitant injuries are thought to predispose to worse outcomes.24
This article systematically reviewed the available literature in order to evaluate the management strategies used, the impact of different types of conservative and surgical treatment on clinical and radiological outcomes, and the impact of isolated olecranon fractures affecting the growth plate on long-term outcomes. We extracted data for 299 fractures from 15 studies. The results demonstrated significant variability in the classification of fractures, indications for surgery, types of conservative and surgical intervention, and assessment of clinical and radiological outcomes. We used an age limit cut-off of 18 years to define our paediatric population. Although previous literature suggests that the olecranon physis fuses between 13–16 years of age,25 our age limit ensured that we did not miss any cases of persistent olecranon ossification centres meriting inclusion in the study.
The classification systems used in the articles included in this review are of varied quality and usefulness. The Evans classification13 is the most comprehensive paediatric olecranon specific system. The other paediatric classification systems used are either not specific to the olecranon or are not of practical use in decision making. Applying adult classification systems to the paediatric population may not be appropriate as they do not take into account the physeal specific injuries this population suffer from, or the common associated injuries around the elbow.
The indications for operative intervention in olecranon fractures are not clearly defined. There is little evidence to indicate whether choosing 2 mm, 3 mm, or 4 mm displacement/articular step off is appropriate. Thirty-three fractures managed conservatively in our review were displaced up to 4 mm and had universally good outcomes, which suggests that this may well be a safe cut-off for conservative versus surgical intervention. The amount of articular step off is both less clearly defined and harder to evaluate on plain radiographs due to the thick articular cartilage and various stages of ossification.26
Conservative treatment in a collar and cuff or sling for undisplaced olecranon fractures did not result in an adverse outcome compared to cast immobilization. In fact, cast treatment was associated with temporary stiffness, with all cases resolved by 24 weeks (and most by 10 weeks). The decision to apply cast immobilization or collar and cuff/sling seemed to be arbitrary/surgeon specific in the studies in this review. The duration of immobilization ranged considerably from 2–6 weeks. Cast immobilization versus sling/collar and cuff immobilization has been studied in other undisplaced fractures around the elbow in children with results suggesting that pain control and return to function is better in the cast groups.27,28 Due to the relative rarity of isolated olecranon fractures in this age group, such studies have not been undertaken for this injury. It seems that it would be reasonable to use either modality with good medium–long-term expected outcomes.
Both TBW and TBS seem to be reliable techniques when well applied to displaced fractures (i.e. well reduced fracture, following AO tension band principles). TBS seemed to have increased rates of revision compared to wiring in one series, with the predictor of suture failure being that of a weight > 50 kg.19 Biomechanical studies support this finding as TBS have lower ultimate failure loads than TBW fixation.29 It may therefore be sensible in the heavier child to offer wiring techniques instead.
Other techniques, e.g. screw fixation or cerclage techniques, do not have sufficient evidence behind them to recommend as a routine line of treatment for displaced olecranon fractures. Caution should be paid particularly to screw fixation for OI-related fractures where in one series there was a 50% rate of migration or refracture with screw fixation. Given there are well established surgical options in TBW/TBS with relatively low morbidity, it is not clear what advantage these other techniques offer at present, although they may have their role in specific less-common fracture patterns.30 Plate fixation of acute olecranon fractures was not identified in this review (only one case of delayed diagnosis with non-union). This may be because we excluded cases with ipsilateral elbow fractures or that the types of fracture pattern requiring this fixation modality are not common in children.
The objective clinical outcome measurement tools in use are of wide variability and quality, with few studies using well established, useful measures. This concern regarding a lack of validated outcome measures for paediatric olecranon fractures in the reported literature is echoed elsewhere.30 The paediatric specific system for olecranon fractures used by Gicquel et al10 allows for rigorous reporting of results; however, this outcome system has not been validated. Variation in use of validated paediatric and disease specific outcome measures is well recognized31 and is of importance in trying to further our understanding of appropriate treatment strategies.
Provided the fracture is well reduced (whether treated surgically or conservatively), patients should gain a good clinical outcome, with minimal long-term morbidity for isolated injuries. The most common unfavourable outcome was stiffness (typically < 20 degrees loss of extension) seen in 30 patients, and associated with screw fixation, cast immobilization and malreduced fractures.
The radiological outcome tools in use are limited for olecranon fractures. Outcomes were mostly non-systematically recorded and with variation between studies. For well reduced fractures there were no long-term effects with regard to deformity or post-traumatic arthritis. Poorly reduced fractures resulted in non-union in one case (not immobilized), and post-traumatic arthritis development in another (inadequate intra-operative reduction). Olecranon epiphyseal overgrowth was only seen in one study with four fractures undergoing TBW. In all other cases the radiological follow up showed no significant abnormalities either in terms of post-traumatic arthritic changes, or abnormalities with regard to the physis whether undergoing conservative or surgical management.
Patients with OI are known to be more prone to olecranon fractures.32 The immobilization period was shorter than in those patients without OI14 due to the theoretically increased risk of immobilization-induced osteoporosis in this population. There was a significant rate of re-fracture after removal of metalwork and incidence of contralateral olecranon fracture in the series in this review. Consideration should be given to delayed removal of metalwork in this population, and appropriate counselling regarding the risk of re-fracture and contralateral fracture.
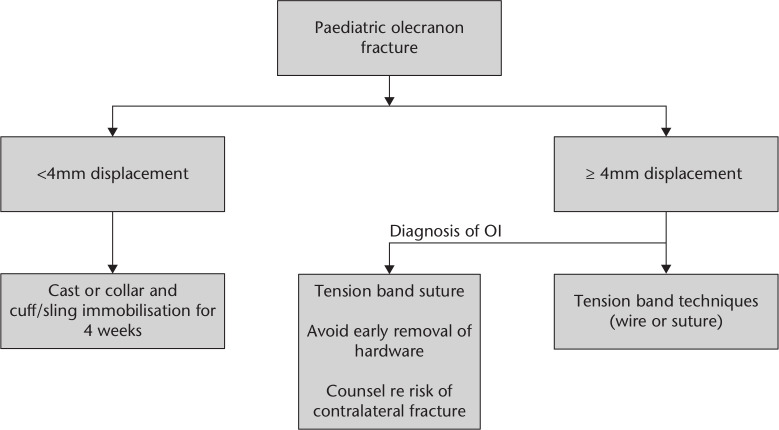
On the basis of this review and until we have a core outcome set for these fractures, we suggest the following algorithm for use in the treatment of paediatric olecranon fractures (Fig. 2). The variability in surgical indications makes it difficult to conclude an absolute value of displacement to recommend surgical intervention. However, all patients in the series treated non-operatively with < 4 mm displacement had good clinical outcomes (with either collar and cuff or cast treatment for 3–4 weeks), and those with ≥ 4 mm displacement treated surgically with an anatomical reduction using TBW/TBS techniques (with or without routine removal of metalwork) had good clinical outcomes.
Fig. 2.
Flowchart of proposed treatment algorithm.
Note. OI, osteogenesis imperfecta.
Conclusion
The reported outcomes of isolated olecranon fractures in children show predictably positive results for the well reduced fracture in terms of pain, stiffness, physeal injury, and post-traumatic OA. Special considerations should be made for the older and heavier (> 50 kg) child with OI, and the indications for the use of fracture specific treatment, e.g. with cerclage techniques or screw fixation as appropriate to the fracture pattern. Use of established clinical and radiological core outcome sets specific to the paediatric population will help improve the quality of future studies for this relatively rare injury.
Appendix
Appendix 1.
Risk of bias assessment
| Study | Risk of bias | Issues leading to risk of bias |
|---|---|---|
| Caterini et al | High | Only 39/63 patients included clinical outcomes, e.g. range of motion missing, surgical details missing |
| Corradin et al | Moderate | Short follow up period |
| Gaddy et al | Moderate | Radiographic analysis subject to bias |
| Gicquel et al | High | Unclear selection process; variable follow up periods; surgical techniques unclear |
| Gwynne-Jones | Moderate | No assessor blinding of interventions; intervention groups not clearly defined |
| Karlsson et al | Low | |
| Kim et al | Moderate | Unclear selection process |
| Maffulli et al | High | Unclear selection process; interventions and outcomes inadequately reported |
| Maity et al | Low | |
| Matthews | High | Unclear selection criteria; interventions, outcomes and follow up periods inadequately reported |
| Newell | High | Unclear selection criteria; interventions, outcomes and follow up periods inadequately reported |
| Papavasiliou et al | High | Unclear selection criteria; interventions, outcomes and follow up periods inadequately reported |
| Perkins et al | Moderate | Outcomes inadequately reported (e.g. patient-reported outcomes, range of motion) |
| Persiani et al | Low | |
| Zionts et al | High | Unclear selection criteria, interventions and outcomes inadequately reported |
Footnotes
ICMJE Conflict of interest statement: MA reports payment for patents (planned, pending or issued), outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Matthews JG. Fractures of the olecranon in children. Injury 1980;12:207–212. [DOI] [PubMed] [Google Scholar]
- 2. Veillette CJH, Steinmann SP. Olecranon fractures. Orthop Clin North Am 2008;39:229–236. [DOI] [PubMed] [Google Scholar]
- 3. Morrey BF. Current concepts in the treatment of fractures of the radial head, the olecranon, and the coronoid. Instr Course Lect 1995;44:175–185. [PubMed] [Google Scholar]
- 4. Lenz M, Wegmann K, Müller LP, Hackl M. Nonoperative treatment of olecranon fractures in the elderly: a systematic review. Obere Extremität 2019;14:48–52. [Google Scholar]
- 5. Brolin TJ, Throckmorton T. Olecranon fractures. Hand Clin 2015;31:581–590. [DOI] [PubMed] [Google Scholar]
- 6. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med 2018;23:60–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kim TH, Lee D-H, Han KJ, Choi WS, Cho JH. Early range of motion exercise in pediatric patients with olecranon fractures treated with tension band suture with double loops and double knots. J Shoulder Elbow Surg 2017;26:e227–e231. [DOI] [PubMed] [Google Scholar]
- 9. Corradin M, Marengo L, Andreacchio A, et al. Outcome of isolated olecranon fractures in skeletally immature patients: comparison of open reduction and tension band wiring fixation versus closed reduction and percutaneous screw fixation. Eur J Orthop Surg Traumatol 2016;26:469–476. [DOI] [PubMed] [Google Scholar]
- 10. Gicquel P, Giacomelli M-C, Karger C, Clavert J-M. Surgical technique and preliminary results of a new fixation concept for olecranon fractures in children. J Pediatr Orthop 2003;23:398–401. [PubMed] [Google Scholar]
- 11. Gwynne-Jones DP. Displaced olecranon apophyseal fractures in children with osteogenesis imperfecta. J Pediatr Orthop 2005;25:154–157. [DOI] [PubMed] [Google Scholar]
- 12. Karlsson MK, Hasserius R, Karlsson C, Besjakov J, Josefsson PO. Fractures of the olecranon during growth: a 15–25-year follow-up. J Pediatr Orthop B 2002;11:251–255. [DOI] [PubMed] [Google Scholar]
- 13. Maity A, De C, Mukhopadhyay KK, Mondal BC, Adak S. Outcome of open reduction and internal fixation with percutaneously placed K-wires and absorbable tension-band sutures for displaced olecranon fractures in children: a prospective study. Tech Shoulder Elbow Surg 2012;13:138–141. [Google Scholar]
- 14. Persiani P, Ranaldi FM, Graci J, et al. Isolated olecranon fractures in children affected by osteogenesis imperfecta type I treated with single screw or tension band wiring system: outcomes and pitfalls in relation to bone mineral density. Medicine (Baltimore) 2017;96:e6766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Caterini R, Farsetti P, D’Arrigo C, Ippolito E. Fractures of the olecranon in children: long-term follow-up of 39 cases. J Pediatr Orthop B 2002;11:320–328. [DOI] [PubMed] [Google Scholar]
- 16. Gaddy BC, Strecker WB, Schoenecker PL. Surgical treatment of displaced olecranon fractures in children. J Pediatr Orthop 1997;17:321–324. [PubMed] [Google Scholar]
- 17. Papavasiliou VA, Beslikas TA, Nenopoulos S. Isolated fractures of the olecranon in children. Injury 1987;18:100–102. [DOI] [PubMed] [Google Scholar]
- 18. Zionts LE, Moon CN. Olecranon apophysis fractures in children with osteogenesis imperfecta revisited. J Pediatr Orthop 2002;22:745–750. [PubMed] [Google Scholar]
- 19. Perkins CA, Busch MT, Christino MA, et al. Olecranon fractures in children and adolescents: outcomes based on fracture fixation. J Child Orthop. 2018;12:497–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Murphy DF, Greene WB, Dameron TB., Jr Displaced olecranon fractures in adults: clinical evaluation. Clin Orthop Relat Res 1987;224:215–223. [PubMed] [Google Scholar]
- 21. Graves SC, Canale ST. Fractures of the olecranon in children: long-term follow-up. J Pediatr Orthop 1993;13:239–241. [PubMed] [Google Scholar]
- 22. Maffulli N, Chan D, Aldridge MJ. Overuse injuries of the olecranon in young gymnasts. J Bone Joint Surg [Br] 1992;74:305–308. [DOI] [PubMed] [Google Scholar]
- 23. Newell RLM. Olecranon fractures in children. Injury 1975;7:33–36. [DOI] [PubMed] [Google Scholar]
- 24. Evans MCMB, Graham HKFRCS. Olecranon fractures in children: Part 1: a clinical review; Part 2: a new classification and management algorithm. [Miscellaneous Article]. J Pediatr Orthop 1999;19:559–569. [DOI] [PubMed] [Google Scholar]
- 25. Miyazaki CS, Maranho DA, Agnollitto PM, Nogueira-Barbosa MH. Study of secondary ossification centers of the elbow in the Brazilian population. Acta Ortop Bras 2017;25:279–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cheng JC, Wing-Man K, Shen WY, et al. A new look at the sequential development of elbow-ossification centers in children. J Pediatr Orthop 1998;18:161–167. [PubMed] [Google Scholar]
- 27. Ballal MS, Garg NK, Bass A, Bruce CE. Comparison between collar and cuffs and above elbow back slabs in the initial treatment of Gartland type I supracondylar humerus fractures. J Pediatr Orthop B 2008;17:57–60. [DOI] [PubMed] [Google Scholar]
- 28. Oakley E, Barnett P, Babl FE. Backslab versus nonbackslab for immobilization of undisplaced supracondylar fractures: a randomized trial. Pediatr Emerg Care 2009;25:452–456. [DOI] [PubMed] [Google Scholar]
- 29. Parent S, Wedemeyer M, Mahar AT, et al. Displaced olecranon fractures in children: a biomechanical analysis of fixation methods. J Pediatr Orthop 2008;28:147–151. [DOI] [PubMed] [Google Scholar]
- 30. Flynn JM, Skaggs DL, Waters PM. Rockwood and Wilkins’ fractures in children. •••: Wolters Kluwer Health, 2014. [Google Scholar]
- 31. Truong WH, Price MJ, Agarwal KN, et al. Utilization of a wide array of nonvalidated outcome scales in pediatric orthopaedic publications: can’t we all measure the same thing? J Pediatr Orthop 2019;39:e153–e158. [DOI] [PubMed] [Google Scholar]
- 32. Peddada KV, Sullivan BT, Margalit A, Sponseller PD, Md M. Fracture patterns differ between osteogenesis imperfecta and routine pediatric fractures. J Pediatr Orthop 2018;38:e207–e212. [DOI] [PubMed] [Google Scholar]