Abstract
The aim of this systematic review was to present and assess the quality of evidence for learning curve, component positioning, functional outcomes and implant survivorship for image-free hand-held robotic-assisted knee arthroplasty.
Searches of PubMed and Google Scholar were performed in line with the Preferred Reporting Items for Systematic Review and Meta-Analysis statement. The criteria for inclusion was any published full-text article or abstract assessing image-free hand-held robotic knee arthroplasty and reporting learning curve, implant positioning, functional outcome or implant survival for clinical or non-clinical studies.
There were 22 studies included. Five studies reported the learning curve: all were for unicompartmental knee arthroplasty (UKA) – no learning curve for accuracy, operative time was reduced after five to 10 cases and a steady surgical time was achieved after eight cases.
There were 16 studies reporting accuracy: rate of outliers was halved, higher rate of joint line and mechanical axis restoration, supported by low root mean square error values.
Six studies reported functional outcome: all for UKA, improvement at six to 52 weeks, no difference from manual UKA except when assessed for lateral UKA which showed improved clinical outcomes.
Two studies reported survivorship: one reported an unadjusted revision rate of 7% at 20 months for medial UKA and the other found a 99% two-year survival rate for UKA.
There was evidence to support more accurate implant positioning for UKA, but whether this is related to superior functional outcomes or improved implant survivorship was not clear and further studies are required.
Cite this article: EFORT Open Rev 2020;5:319-326. DOI: 10.1302/2058-5241.5.190065
Keywords: arthroplasty, image free, knee, Navio, outcomes, robot
Introduction
Robotic-arm-assisted knee arthroplasty has been shown to enable more accurate implant positioning for both unicompartmental knee arthroplasty (UKA) and total knee arthroplasty (TKA) when compared to manual surgery.1,2 Robotic-arm-assisted surgery is also associated with reduced intraoperative trauma to the soft tissue envelope when performing the bone cuts compared to manual performed knee arthroplasty.3 This has been associated with improved early outcomes, such as shorter length of hospital stay, improved range of movement and better patient-reported outcomes.4–6 Robotic-arm-assisted UKA has been shown to be a cost-effective intervention, with the increased costs of the robot being balanced against improved outcomes, relative to TKA, and lower early revisions costs when compared to manually performed UKA.7
A disadvantage of robotically assisted knee arthroplasty is that some systems, such as the robotic-arm-assisted Mako (Stryker) knee, need a preoperative computed tomography (CT) scan to enable intraoperative shape matching of the scan onto the real bony anatomy. This exposes the patient to radiation which is potentially associated with an increased risk of developing life-threatening cancer.8 In addition, there is also an extra financial cost for the scan.7 Image-free robotically assisted knee surgery, by definition, does not require a preoperative CT scan and averts any increased risk of cancer and the associated cost of the scan. Current systematic reviews of robotic-assisted knee surgery often amalgamate the outcomes of both image-based and image-free systems.9 Despite the advantages of image-free hand-held robotic-assisted knee arthroplasty surgery, the authors are not aware of any published review reporting the evidence for this in isolation from image-based systems.
The aim of this systematic review was to present and assess the quality of evidence for learning curve, component positioning, functional outcomes and implant survivorship for image-free hand-held robotic-assisted knee arthroplasty.
Methods
A search of PubMed and Google Scholar was performed in September 2019 in line with the 2009 Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement.10 Titles and abstracts identified were independently reviewed by two authors (NDC and MA) and those not meeting the inclusion criteria were excluded prior to full-text review. On occasions when it was not clear from the abstract whether studies were of relevance, the full text of the article when possible was subsequently reviewed. Unanimous consensus was met on the inclusion of proposed studies for full-text review amongst the authors (NDC and MA). Full-text studies were further evaluated against the inclusion and exclusion criteria. A search of the references was performed of the selected studies to ensure no other relevant studies were overlooked.
Search terms and criteria for inclusion
Search terms included “robot” or “robotic” and “knee”. A single search of PubMed using the search term ((Robot) OR Robotic) AND (Knee) yielded 1235 abstracts. Two searches of Google Scholar using the search terms (1) allintitle: robot Knee and (2) allintitle: robotic Knee yielded 420 and 321 articles, respectively. The criteria for inclusion were any published research article studying robotic total or unicompartmental (medial, lateral, or patellofemoral) knee arthroplasty and reporting on functional outcomes or component positioning or learning curve or survivorship including clinical, cadaveric or dry bone studies. Studies were excluded if they were case reports, review articles or were not available in the English language.
Data extraction
The collected data from each study included the authors, year of publication, title, where it was published, type of publication (full article, abstract only or case report), compartment replaced (medial, lateral, patellofemoral, or total), study design (prospective or retrospective), type (clinical, cadaver or saw bones), age, number of patients/specimens, follow up (if applicable), the type of implant used, type of tibial prosthesis, and depending on the aims of the study: implant survival, functional outcome, implant alignment and learning curve. In addition, the main conclusion from each study was also recorded.
Outcome measures
Our primary objectives were to report learning curve, component positioning, functional outcomes and implant survivorship within the included studies. Secondary objectives included presenting the demographic data as well as the type of robots and implants used across the included articles.
Quality assessment
All studies were quality assessed by two authors (NDC and MA) using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies.11 The assessment tool uses 14 questions to enable allocation of a score to each article (poor, fair or good). If there was disagreement regarding the scoring of a study, consensus was met after discussion between both assessors.
Results
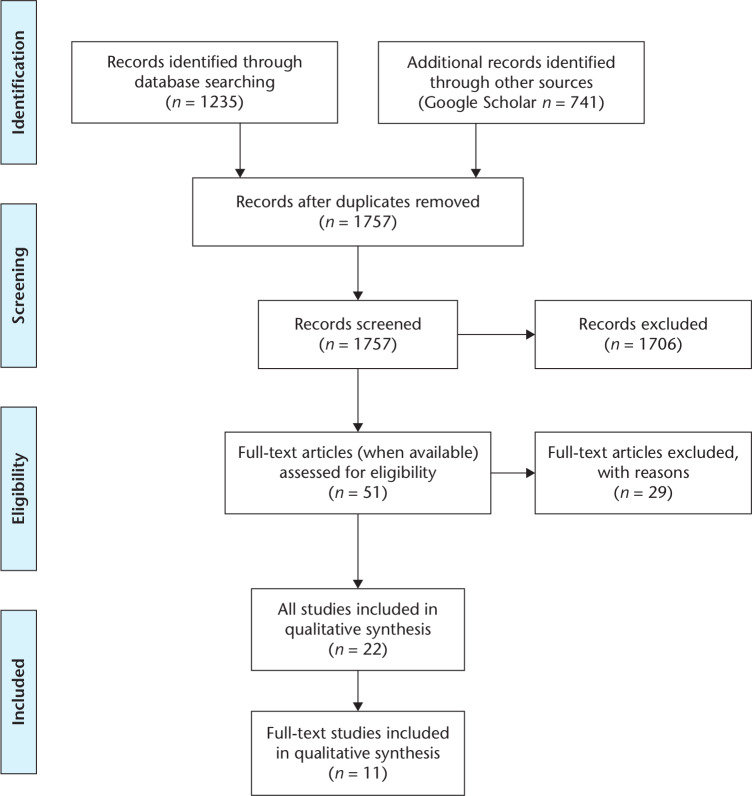
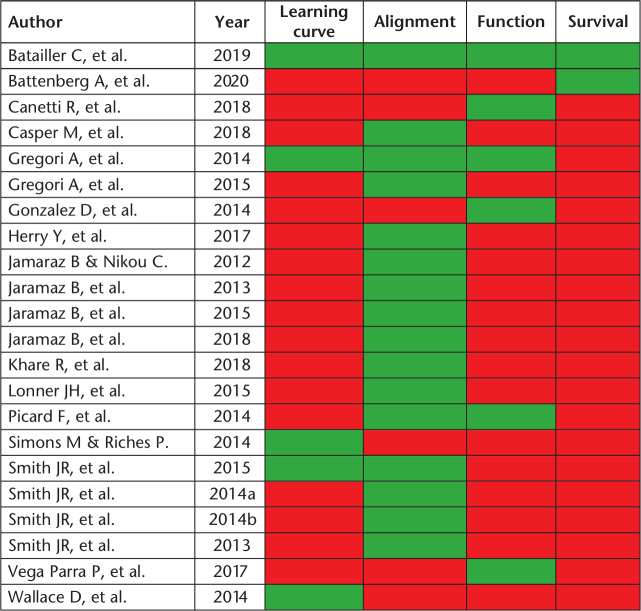
There were 1976 articles identified in the initial search of databases and reference lists. After initial screening of titles and abstracts, 51 articles met the inclusion criteria for review. On full-text screening (when available), a further 29 studies were removed as they represented review articles or duplicate studies (Fig. 1). A list of the 22 studies which met the inclusion criteria are presented in Table 1.12–33 Nine studies were identified from PubMed, three additional studies from Google Scholar and 10 more through the reference lists of the identified studies (Table 1). The year of publication ranged from 2012 to 2020. There were 11 clinical studies of which one was prospective and the remainder were retrospective cohort studies. There were 11 non-clinical studies of which six involved only cadavers, three involved only saw bone models and two were a mix of both specimen types. There were no randomized controlled trials or cost-analysis studies identified. There were 11 full-text published articles included and the remaining 11 were published abstracts from scientific meeting presentations (Table 1). Fig 2 illustrates the outcomes reported by the 22 studies included in this review.
Fig. 1.
PRISMA flow diagram outlining article/abstract selection process.
Source: Moher D, Liberati A, Tetzlaff J, Altman DG; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. PLoS Med 2009;6:e1000097. doi:10.1371/journal.pmed1000097. For more information, visit www.prisma-statement.org
Table 1.
Studies included in the systematic review according to how they were identified, where they were published, design, patient demographics, follow up and type of implant
| Authors | Year | Search | Journal | Compartment (n) |
Design | Clinical/ non-clinical |
Patients (n) |
Age | FU (months) |
Implant | Tibial prosthesis |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Batailler et al12 | 2019 | PM | Yes | M57 L23 | Retrospective case control | Clinical | 80 vs. 80 | 69 | 20 | HLS Uni evolution, Tornier® | All poly |
| Battenberg et al13 | 2020 | PM | Yes | M124 L4 | Retrospective | Clinical | 128 | 64 | 28 | ? | |
| Canetti et al14 | 2018 | PM | Yes | Lateral | Retrospective case control |
Clinical | 11 vs. 17 | 66 vs. 59 | 37 | HLS Uni Evolution, Tornier® | All poly |
| Casper et al15 | 2018 | PM | Yes | TKA | Prospective | Cadaver | 18 | N/A | N/A | Journey II, Genesis, Legion | ? |
| Gregori et al16 | 2014 | REF | No | M | Retrospective | Clinical | 57 | 63 | 6 weeks | ? | All poly |
| Gregori et al17 | 2015 | REF | No | M | Prospective | Clinical | 92 | ? | N/A | ? | ? |
| Gonzalez et al18 | 2014 | REF | No | ? | Retrospective | Clinical | 18 | 61 | 6 weeks | ? | Metal backed |
| Herry et al19 | 2017 | PM | Yes | M23 L17 | Retrospective case control | Clinical | 40 vs. 40 | 69 vs. 68 | N/A | HKS Uni Evolution Tornier | All poly |
| Jaramaz and Nikou20 | 2012 | PM | Yes | M | Prospective | Saw bone | 5 | N/A | N/A | ? | ? |
| Jaramaz et al21 | 2013 | REF | No | ? | Prospective | Cadaver | 4 knees | N/A | N/A | ? | ? |
| Jaramaz et al22 | 2015 | REF | No | PF | Prospective | Saw bone & cadaver | 24 | N/A | N/A | ? | ? |
| Jaramaz et al23 | 2018 | GS | Yes | TKA | Prospective | Saw bone & cadaver | ** | N/A | N/A | Journey II XR | ? |
| Khare et al24 | 2018 | PM | Yes | M | Prospective comparison | Cadaver | 6 vs 6 | N/A | N/A | Stride Uni S&N | ? |
| Lonner et al25 | 2015 | PM | Yes | M | Prospective | Cadaver | 25 | N/A | N/A | HLS Uni Evolution, Tornier® | ? |
| Picard et al26 | 2014 | GS | No | M | Retrospective | Clinical | 65 | 63 | 6 weeks | ? | ? |
| Simons and Riches27 |
2014 | REF | No | M | Prospective | Saw bone | 25 | N/A | N/A | HLS Uni Evolution, Tornier® | ? |
| Smith et al28 | 2015 | REF | No | ? | Retrospective | Clinical | 298 | ? | N/A | ? | ? |
| Smith et al29 | 2014 | PM | Yes | M | Prospective | Saw bone | 20 | N/A | N/A | Blue Belt Technologies | ? |
| Smith et al30 | 2014 | REF | No | ? | Prospective | Cadaver | 25 | N/A | N/A | ? | ? |
| Smith et al31 | 2013 | REF | No | ? | Prospective | Cadaver | 9 | 71 | N/A | Tornier Uni | ? |
| Vega Parra et al32 | 2017 | REF | Yes | M | Retrospective | Clinical | 47 | 67 | 12 | Stride Uni S&N | ? |
| Wallace et al33 | 2014 | GS | No | ? | Retrospective | Clinical | ? | ? | N/A | ? | ? |
Note. PM: PubMed; GS: Google Scholar; REF: references; M: medial; L: Lateral; TKA: total knee arthroplasty; PF: patellofemoral; ?: not stated; FU: follow up; N/A: not applicable.
**Cadaveric: 24 femurs and 2 tibias. Synthetic saw bone: 8 femurs and 10 tibias.
Fig. 2.
Heatmap illustrating the reporting of outcomes for the included studies.
Green: yes, red: no.
Learning curve (weak evidence)
There were five studies reporting the learning curve, all of which were for UKA (Table 2). There was only one published full-text article reporting the learning curve which assessed 27 lateral and 53 medial robotically assisted UKA and concluded there was no learning curve.12 They stated, ‘There was no learning curve for the robotic-assisted group (implant position, revision rate or clinical outcomes)’, but do not describe the methods used to assess these endpoints or how these were defined. Of the remaining four abstract publications there was no learning curve found for accuracy (n = 2),27,28 and the operative time was reduced by 15 to 37 minutes after five to 10 cases and a steady state surgical time was achieved after eight cases.16,33
Table 2.
Evidence for learning curve
| Author | Year | Findings |
|---|---|---|
| Batailler et al12 | 2019 | No learning curve for position/revision/function* |
| Gregori et al16 | 2014 | Learning curve reduced by 15 minutes after ten cases* |
| Simons and Riches27 | 2014 | No learning curve for accuracy, and a significant decrease in surgical time after five cases (37 minutes) |
| Smith et al28 | 2015 | No learning curve for accuracy* |
| Wallace et al33 | 2014 | Eight procedures (range 5–11) to reach a steady state surgical time* |
Studies in italics signifies an abstract publication only
*Signifies a clinical study
Implant accuracy (fair evidence)
There were 16 studies identified that reported implant position accuracy, of which six were clinical studies and 10 were cadaver/saw bone studies (Table 3). The six clinical articles included two full-text published papers which found the rate of outliers to be half that of manually performed UKA and that joint line restoration was more accurate with robotically performed UKA.12,19 The four clinical abstract publications supported these findings with a higher rate of restoration of planned mechanical axis to within 1 to 3 degrees 89% to 99% of the time.16,17,26,28 There were six published full-text non-clinical studies of which two assessed TKA15,23 and four assessed UKA,17,20,24,29 all of which demonstrated low root square mean (RMS) error values. Khare et al24 compared manual with robotic-assisted UKA, finding a lower error rate in the robotically assisted group. Lonner et al25 demonstrated the RMS error of the Navio-assisted UKA to be similar to the published figures of the image-based Mako UKA system. An abstract publication by Jaramaz et al (2015) was the only study assessing patellofemoral arthroplasty position, which was accurate with a maximal RMS error of less than 0.9 mm.22
Table 3.
Evidence for implant accuracy
| Author | Year | Findings |
|---|---|---|
| Batailler et al12 | 2019 | Fewer outliers (> 2 degrees) with robotic UKA compared to manual UKA: medial UKA 16% vs. 32% and lateral UKA 26% vs. 61%* |
| Casper et al15 | 2018 | RMS error (degrees): femoral flexion 2.0, varus/valgus 0.1, rotation 0.5, and for tibial slope 0.2 and varus/valgus 0.2 |
| Gregori et al16 | 2014 | 91% within 1 degree of planned mechanical axis* |
| Gregori et al17 | 2015 | 89% within 3 degrees of planned coronal mechanical axis* |
| Herry et al19 | 2017 | Less distal joint line with robotic UKA (1.4 mm vs. 4.6 mm)* |
| Jaramaz and Nikou20 | 2012 | Average distance from the planned implant position was 0.54 mm and the average angular difference was 1.08 degrees |
| Jaramaz et al21 | 2013 | Within 1.5 mm of target position (8 divots) |
| Jaramaz et al22 | 2015 | All implants were placed within a maximum RMS error of 0.87 mm from the target position |
| Jaramaz et al23 | 2018 | RMS error: femoral varus/valgus 0.7 degrees, rotation 0.7 degrees and distal resection 0.86 mm and for the tibial slope 0.9 degrees, varus/valgus 0.7 degrees and resection depth 0.68 mm |
| Khare et al24 | 2018 | RMS error less with robotic UKA compared to manual UKA: femoral flexion 1.2 vs. 7.5 degrees, varus/valgus 2.8 vs. 6.3 degrees, and rotation 1.6 vs. 5.0 degrees, and for the tibia slope 2.4 vs. 4.0 degrees and varus/valgus 3.0 vs. 1.8 degrees |
| Lonner et al25 | 2015 | RMS error: femoral flexion 1.3 degrees, varus/valgus 2.3 degrees, rotation 1.6 degrees and for the tibial slope 2.0 degrees, varus/valgus 2.4 degrees and rotation 1.9 degrees |
| Picard et al26 | 2014 | 91% within 1 degree of planned mechanical axis* |
| Smith et al28 | 2015 | Tibiofemoral angle with 1, 2 and 3 degrees of planned 89%, 97% and 99% of the time* |
| Smith et al29 | 2014 | RMS error: femoral flexion 1.1 degrees, varus/valgus 1.5 degrees, rotation 1.3 degrees and for the tibial slope 0.7 degrees, varus/valgus 1.2 degrees and rotation 1.3 degrees |
| Smith et al30 | 2014 | RMS error: femoral rotation 2.3 degree and translation 1.6 mm, and tibial rotation 2.6 degrees and translation 1.7 mm |
| Smith et al31 | 2013 | RMS error: femoral rotation 2 degree and translation 1.1 mm, and tibial rotation 2.6 degrees and translation 2.0 mm |
Note. UKA, unicompartmental knee arthroplasty; RMS, root square mean.
Studies in italics signifies an abstract publication only.
*Signifies a clinical study.
Functional outcomes (weak evidence)
There were six clinical studies reporting the function outcome of UKA (Table 4), of which three were published articles and three were abstract publications. Batailler et al12 found no significant difference in functional outcome between robotic-assisted and manual UKA. However, in contrast, when assessing lateral UKA, Canetti et al14 found a significantly greater improvement in the clinical component of the Knee Society Score (KSS) of 8 points, which was also clinically significant being greater than the minimally important difference of 5 points,34 for robotic-assisted compared to manual UKA. Neither of these studies were powered to the KSS, nor did they correct for multiple statistical testing. Vega Parra et al32 demonstrated a significant improvement in function at one year after medial robotic UKA but did not compare this to a manual UKA cohort. There were three published abstracts identified by the same research group from 2014, all of which demonstrated a 14 to 15-point improvement in the Oxford Knee Score six weeks following robotic UKA,16,18,26 but again this was not compared to a control/manual group.
Table 4.
Evidence for functional outcome. Studies in italics signifies an abstract publication only
| Author | Year | Findings |
|---|---|---|
| Batailler et al12 | 2019 | No difference in the KSS (clinical and functional) at a mean of 20 months of manual (n = 80) versus robotic (n = 80) UKA |
| Canetti et al14 | 2018 | Significantly greater improvement in the clinical component of the KSS for robotic-assisted lateral UKA (n = 11) compared to manual lateral UKA at a mean of three years follow up, but no difference in the functional component of the KSS |
| Gregori et al16 | 2014 | OKS 22 to 36 at six weeks (14-point improvement) |
| Gonzalez et al18 | 2014 | OKS 38 to 23 at six weeks (15-point improvement) |
| Picard et al26 | 2014 | OKS 38 to 24 at six weeks (14-point improvement) |
| Vega Parra et al32 | 2017 | Significant improvement in all six components of the KOOS 12-months post medial UKA (n = 47) |
Note. KSS, Knee Society Score (Insall CORR 248, 1989, 13-14); UKA, unicompartmental knee arthroplasty; OKS, Oxford Knee Score; KOOS, Knee Osteoarthritis Outcome Score.
Survival (weak evidence)
Only two survivorship studies were identified.12,13 Batailler et al12 found no revisions at a mean of 20 months follow up in the those undergoing lateral robotic-assisted UKA but did identify four (n = 4/57, 7%) revisions of robotic-assisted medial UKA. However, they did not use standard survival analysis. In contrast, Battenberg et al13 used Kaplan–Meier survivorship analysis and demonstrated a 99% two-year survival for a cohort of 128 robotically assisted UKA. Battenberg et al13 did not state what type of implant was assessed or whether it was an all polyethylene tibial component (Table 1).
Discussion
The key findings of this systematic review of image-free hand-held robotic-assisted knee arthroplasty were: (1) currently there was limited evidence to support the use of such robotic-assisted surgery, (2) the majority of the evidence relates to UKA, (3) evidence for learning curve, functional outcome and survival is weak, (4) the evidence for the clinical accuracy of implant position is fair, (5) there is poor reporting of implant type/design, and (6) there were no data reporting patient expectations or cost-economic analysis and there were no randomized controlled trials.
A limitation of this systematic review was the inclusion of the published abstract data from scientific presentations, which were not able to be assessed fully for the quality of the data presented and they had to be assumed to represent weak evidence. To have excluded this data would have resulted in losing half of the included studies. The abstract data were thought to represent supporting evidence for the full-text published articles that were included, as they were found to present weak to fair evidence. In addition, no meta-analysis was undertaken in this review. This would have been possible using the reported RMS errors identified; however, all were of a similar accuracy and would have likely not offered any additional new information. A meta-analysis of learning curve, functional outcome and survival would not have been possible due to the poor quality of evidence and heterogenicity of the reported data.
There is limited and poor evidence for the learning curve for image-free hand-held robotic-assisted knee arthroplasty and what exists is for UKA. The only published full-text article states no learning curve for accuracy, revision or functional outcomes but is not clear about how these were assessed.12 From an accuracy perspective this is in keeping with the image-based systems, where no learning curve is observed for UKA or TKA.35,36 The reported learning curve for operative time from the identified published abstracts is also similar to that reported for the image-based Mako system of between five to 10 cases.35,36 There is a need for improved evidence for the learning curve for UKA and especially for TKA as there is currently none with defined methods.
Most of the studies included in this review (16 of 22) focused on implant positioning, which may be expected given that the potential benefit of robotic-assisted knee arthroplasty is more accurate implant placement. The current review found a body of evidence that supported robotic-assisted over manual UKA with a reduced rate of outliers (> 2 degrees from planned) and more accurate restoration of the joint line when compared to manual UKA, and achievement of a planned mechanical axis to within 1 to 3 degrees 89% to 99% of the time. These results are supported by the non-clinical studies reporting a low RMS error. These reported RMS error rates for image-free are similar to those described for image-based systems, suggesting similar accuracy but without the need for a preoperative CT scan.1,37,38 There was no clinical paper identified that assessed the accuracy of robotic-assisted TKA for either alignment compared to a planned or in comparison to a matched manual TKA cohort.
There were two retrospective case-control studies identified that compared the functional outcome of robotic versus manual UKA; however, the results were conflicting. Batailler et al12 found no significant difference in functional outcome between robotic-assisted and manual UKA, but they included both medial and lateral UKA in each group. Canetti et al14 only assessed lateral UKA and demonstrated a statistical and greater clinically significant improvement in the clinical component of the KSS in those undergoing robotic-assisted compared to those undergoing manual surgery. Neither of these studies were powered to the KSS and their findings may represent type II and type I errors, respectively. Functional outcome studies for robotic-arm-assisted image-based systems have been shown to offer decreased postoperative pain and increased range of motion with associated shorter length of hospital stay (LOS), when compared to manual UKA and TKA.4,5 However, there is no significant difference in overall patient-reported outcome measures (PROMs) with robotic-arm-assisted image-based systems when compared to manual medial UKA.39 There were no studies identified in this review that assessed the functional outcome of TKA, nor was there any study powered to a PROM as the primary aim. There were also no studies assessing LOS, patient expectations, return to sports or generic health.
The identified evidence for implant survival was weak. Batailler et al12 reported survival as a simple percentage at a mean of 20 months, not accounting for differences in follow up that would be expected of standard survivorship analysis. Battenberg et al13 demonstrated a 99% two-year survival rate for their cohort of 128 robotically assisted UKA, but did not state what type of implant was assessed or whether it was an all polyethylene tibial component (Table 1). The type of implant is crucial when assessing survival as the all polyethylene tibial component has been associated with a higher failure rate;9,40 so despite robotic-assisted knee surgery potentially offering improved implant position it may fail due to design flaws. There were no survival studies for image-free robotically assisted TKA and what data exist for UKA are limited to two-years follow up.
Conclusion
There is weak to fair evidence for: learning curve, implant positioning, functional outcome or implant survival, of which the majority is for UKA. There is evidence to support more accurate implant positioning for UKA, but whether this is related to superior functional outcomes or improved implant survivorship was not clear and further studies are required.
Footnotes
ICMJE Conflict of interest statement: DJD reports a travel grant from Depuy to complete an unrelated project for unpaid work at Imperial College London for a one-year period.
The other authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Bell SW, Anthony I, Jones B, MacLean A, Rowe P, Blyth M. Improved accuracy of component positioning with robotic-assisted unicompartmental knee arthroplasty: data from a prospective, randomized controlled study. J Bone Joint Surg Am 2016;98:627–635. [DOI] [PubMed] [Google Scholar]
- 2. Hampp EL, Chughtai M, Scholl LY, et al. Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 2019;32:239–250. [DOI] [PubMed] [Google Scholar]
- 3. Hampp EL, Sodhi N, Scholl L, et al. Less iatrogenic soft-tissue damage utilizing robotic-assisted total knee arthroplasty when compared with a manual approach: A blinded assessment. Bone Joint Res 2019;8:495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kayani B, Konan S, Tahmassebi J, Pietrzak JRT, Haddad FS. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Joint J 2018;100-B:930–937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kayani B, Konan S, Tahmassebi J, Rowan FE, Haddad FS. An assessment of early functional rehabilitation and hospital discharge in conventional versus robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J 2019;101-B:24–33. [DOI] [PubMed] [Google Scholar]
- 6. Blyth MJG, Anthony I, Rowe P, Banger MS, MacLean A, Jones B. Robotic arm-assisted versus conventional unicompartmental knee arthroplasty: exploratory secondary analysis of a randomised controlled trial. Bone Joint Res 2017;6:631–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Clement ND, Deehan DJ, Patton JT. Robot-assisted unicompartmental knee arthroplasty for patients with isolated medial compartment osteoarthritis is cost-effective: a Markov decision analysis. Bone Joint J 2019;101-B:1063–1070. [DOI] [PubMed] [Google Scholar]
- 8. Ponzio DY, Lonner JH. Preoperative mapping in unicompartmental knee arthroplasty using computed tomography scans is associated with radiation exposure and carries high cost. J Arthroplasty 2015;30:964–967. [DOI] [PubMed] [Google Scholar]
- 9. Robinson PG, Clement ND, Hamilton D, Blyth MJG, Haddad FS, Patton JT. A systematic review of robotic-assisted unicompartmental knee arthroplasty: prosthesis design and type should be reported. Bone Joint J 2019;101-B:838–847. [DOI] [PubMed] [Google Scholar]
- 10. Moher D, Shamseer L, Clarke M, et al. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. National Heart, Lung, and Blood Institute, Bethesda, Maryland, USA, 2019.
- 12. Batailler C, White N, Ranaldi FM, Neyret P, Servien E, Lustig S. Improved implant position and lower revision rate with robotic-assisted unicompartmental knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 2019;27:1232–1240. [DOI] [PubMed] [Google Scholar]
- 13. Battenberg AK, Netravali NA, Lonner JH. A novel handheld robotic-assisted system for unicompartmental knee arthroplasty: surgical technique and early survivorship. J Robot Surg 2019;14:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Canetti R, Batailler C, Bankhead C, Neyret P, Servien E, Lustig S. Faster return to sport after robotic-assisted lateral unicompartmental knee arthroplasty: a comparative study. Arch Orthop Trauma Surg 2018;138:1765–1771. [DOI] [PubMed] [Google Scholar]
- 15. Casper M, Mitra R, Khare R, et al. Accuracy assessment of a novel image-free handheld robot for Total Knee Arthroplasty in a cadaveric study. Comput Assist Surg (Abingdon) 2018;23:14–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Gregori A, Picard F, Bellemans J, Smith J, Simone A. Handheld precision sculpting tool for unicondylar knee arthroplasty: a clinical review. 15th EFORT Congress 4–6 June, 2014; London, UK. [Google Scholar]
- 17. Gregori A, Picard F, Lonner J, Smith J, Jaramaz B. Accuracy of imageless robotically assisted unicondylar knee arthroplasty. 15th Annual meeting of CAOS 17–20 June, 2015; Vancouver, Canada. [Google Scholar]
- 18. Gonzalez D, Deakin AH, Picard F. Preliminary results of UKR implanted using an image free handheld robotic device. BASK Annual Meeting 8–9 April, 2014; Norwich, UK. [Google Scholar]
- 19. Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S. Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 2017;41:2265–2271. [DOI] [PubMed] [Google Scholar]
- 20. Jaramaz B, Nikou C. Precision freehand sculpting for unicondylar knee replacement: design and experimental validation. Biomed Tech (Berl) 2012;57:293–299. [DOI] [PubMed] [Google Scholar]
- 21. Jaramaz B, Nikou C, Simone A. NAVIO™ PFS for unicondylar knee replacement: early cadaver validation. International Society for Computer Assisted Orthopaedic Surgery; 12–15 June, 2013; Florida, USA. [Google Scholar]
- 22. Jaramaz B, Nikou C, Casper M, Grosse S, Mitra R. Accuracy validation of semi-active robotic application for patellofemoral arthroplasty. 15th Annual meeting of CAOS 17–20 June, 2015; Vancouver, Canada. [Google Scholar]
- 23. Jaramaz B, Mitra R, Nikou C, Kung C. Technique and accuracy assessment of a novel image-free handheld robot for knee arthroplasty in bi-cruciate retaining total knee replacement. Health Sciences 2018;2:98–101. [Google Scholar]
- 24. Khare R, Jaramaz B, Hamlin B, Urish KL. Implant orientation accuracy of a hand-held robotic partial knee replacement system over conventional technique in a cadaveric test. Comput Assist Surg (Abingdon) 2018;23:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lonner JH, Smith JR, Picard F, Hamlin B, Rowe PJ, Riches PE. High degree of accuracy of a novel image-free handheld robot for unicondylar knee arthroplasty in a cadaveric study. Clin Orthop Relat Res 2015;473:206–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Picard F, Gregori A, Bellemans J, Lonner J, Smith J, Gonzalez D, Simone A, Jaramaz B. Handheld robotic-assisted unicondylar knee arthroplasty: a clinical review. 14th Annual meeting of CAOS 18–21 June, 2014; Milan, Italy. [Google Scholar]
- 27. Simons M, Riches P. The learning curve of robotically-assisted unicondylar knee arthroplasty. 8th Combined Meeting of Orthopaedic Research Societies (CORS), 13-16 October 2014; Venice, Italy. [Google Scholar]
- 28. Smith J, Gregori A, Picard F, Lonner J, Jaramaz B. Does image free robotic assisted unicondylar knee arthroplasty achieve surgeons’ specific plan? 15th Annual meeting of CAOS 17–20 June, 2015; Vancouver, Canada. [Google Scholar]
- 29. Smith JR, Riches PE, Rowe PJ. Accuracy of a freehand sculpting tool for unicondylar knee replacement. Int J Med Robot 2014;10:162–169. [DOI] [PubMed] [Google Scholar]
- 30. Smith J, Picard F, Lonner J, Hamlin B, Rowe P, Riches P, Deakin A. The accuracy of a robotically-controlled freehand sculpting tool for unicondylar knee arthroplasty. 14th Annual meeting of CAOS 18–21 June, 2014; Milan, Italy. [Google Scholar]
- 31. Smith J, Picard F, Rowe PJ, Deakin A, Riches PE. The accuracy of a robotically-controlled freehand sculpting tool for unicondylar knee arthroplasty. Congress of ISB 4–9 August, 2013; Natal, Brazil. [Google Scholar]
- 32. Vega Parra PD Barajas JDP Ambrosi RAM Duarte JR. Robotic-assisted unicompartmental knee replacement with NAVIO surigical system: outcome evaluation using knee injury osteoarthritis outcome score. Rev Chil Ortop Traumatol 2017;58:7–12. [Google Scholar]
- 33. Wallace D, Gregori A, Picard F, Bellemans J, Lonner J, Marquez R, Smith J, Simone A, Jaramaz B. The learning curve of a novel handheld robotic system for unicondylar knee arthroplasty. 14th Annual meeting of CAOS 18–21 June, 2014; Milan, Italy. [Google Scholar]
- 34. Lee WC, Kwan YH, Chong HC, Yeo SJ. The minimal clinically important difference for Knee Society Clinical Rating System after total knee arthroplasty for primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc 2017;25:3354–3359. [DOI] [PubMed] [Google Scholar]
- 35. Kayani B, Konan S, Pietrzak JRT, Huq SS, Tahmassebi J, Haddad FS. The learning curve associated with robotic-arm assisted unicompartmental knee arthroplasty: a prospective cohort study. Bone Joint J 2018;100-B:1033–1042. [DOI] [PubMed] [Google Scholar]
- 36. Kayani B, Konan S, Huq SS, Tahmassebi J, Haddad FS. Robotic-arm assisted total knee arthroplasty has a learning curve of seven cases for integration into the surgical workflow but no learning curve effect for accuracy of implant positioning. Knee Surg Sports Traumatol Arthrosc 2019;27:1132–1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dunbar NJ, Roche MW, Park BH, Branch SH, Conditt MA, Banks SA. Accuracy of dynamic tactile-guided unicompartmental knee arthroplasty. J Arthroplasty 2012;27:803–808e1. [DOI] [PubMed] [Google Scholar]
- 38. Cobb J, Henckel J, Gomes P, et al. Hands-on robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br 2006;88:188–197. [DOI] [PubMed] [Google Scholar]
- 39. Gilmour A, MacLean AD, Rowe PJ, et al. Robotic-arm-assisted vs conventional unicompartmental knee arthroplasty: the 2-year clinical outcomes of a randomized controlled trial. J Arthroplasty 2018;33:S109–S115. [DOI] [PubMed] [Google Scholar]
- 40. Scott CE, Eaton MJ, Nutton RW, Wade FA, Evans SL, Pankaj P. Metal-backed versus all-polyethylene unicompartmental knee arthroplasty: proximal tibial strain in an experimentally validated finite element model. Bone Joint Res 2017;6:22–30. [DOI] [PMC free article] [PubMed] [Google Scholar]