Abstract
Fractures of the anterior tibial tuberosity during childhood are an infrequent pathology (around 3% of all proximal tibial fractures), but the incidence of this injury has risen over recent years, likely due to the increased involvement of this age group in sports activities.
This fracture is more commonly seen in children 12–14 years old.
It is vital to identify the anatomical structures associated with this type of fracture, along with the pathophysiological mechanisms involved.
Treatment includes non-operative and operative options, with the goal of achieving articular congruency, restoring the extensor mechanism function, and avoiding damage to the proximal tibial physis.
Understanding the management of this fracture, and the complications that might arise, is critical. The provision of an appropriate clinical management plan and the avoidance of complications are vital in the prevention of disability.
Cite this article: EFORT Open Rev 2020;5:260-267. DOI: 10.1302/2058-5241.5.190026
Keywords: growth plate, paediatrics, tibial fractures
Introduction
The proximal epiphysis of the tibia is the second largest epiphysis of the human body, followed by the epiphysis of the distal femur. In most newborns, the epiphyseal secondary ossification centre (SOC) develops in the first few days after birth (Fig. 1).1 The SOC is present in 95% of female and male newborns at two and five weeks, respectively;2 three months after birth, the SOC is present in all infants (Fig. 2). Initially, the SOC is spherical and located in a central position, but with growth it expands to adopt an elliptical shape. Gradual ossification of the SOC ultimately creates the final shape of the concavity of the tibial plateau; this is usually achieved by the age of 10 years (Fig. 3). The anterior tibial tuberosity possesses a centre of ossification that is separated from the rest of the proximal tibia. During normal development, this centre of ossification appears between the ages of seven and 12 years (Fig. 4).3–6 These two ossification centres have different functions and attributes. The first has the characteristics of an epiphyseal ossification centre in that it is perpendicular to the longitudinal axis of the bone. This centre provides growth and shapes the proximal epiphysis, which articulates with the femur and has no muscle–tendon insertion. In contrast, the ossification centre of the tuberosity is an apophysis that is located tangential to the longitudinal axis of the bone. This centre does not contribute to growth, and does not play a functional role in the joint; rather, it is the site where the patellar tendon inserts. With time, these two ossification centres fuse together, and then merge with the metaphysis; on average, this occurs by the age of 14 years in females and 16 years in males (Fig. 5). The closure and fusion of these ossification centres have an established pattern, beginning in the central zone and then expanding to the periphery and posterior. The ossification centre of the tuberosity is the last to merge with the metaphysis.
Fig. 1.

Anteroposterior and lateral X-ray views of the knee of a 12-day-old female showing the epiphyseal secondary ossification centre of the distal femur and proximal tibia.
Fig. 2.

Anteroposterior and lateral X-ray views of the knee of a three-month-old male with the secondary ossification centres presents.
Fig. 3.

Anteroposterior and lateral X-ray views of the knee of a 10-year-old female showing concavity of the tibial plateau.
Fig. 4.

Anteroposterior and lateral X-ray views of the knee of a 12-year-old male showing separation of the ossification centre of the anterior tibial tuberosity from the rest of the proximal tibia.
Fig. 5.

Anteroposterior and lateral X-ray views of the knee of a 15-year-old male showing that the two centres of ossification have merged.
When the tibia is viewed in the sagittal plane, the patellar tendon is seen to insert directly into the tuberosity. This tendon insertion mechanics represents the main component of anterior tibial tuberosity fractures, both before and after the ossification centre of the tuberosity fully fuses with the proximal epiphysis. The vascular supply for this epiphyseal anatomical zone is provided by arteries that penetrate the physis from different directions, much like the spokes of a bicycle wheel,7 thus providing a significant blood supply and therefore, very low risk of ischemia following fracture. An important vascular structure in this area is the popliteal artery which lies adjacent to the posterior capsule of the knee and descends between the two muscular bellies of the gastrocnemius and ends at the same level as the most distal area of the tuberosity before dividing into the anterior and posterior tibial arteries. Given its narrow nature, this area is prone to popliteal artery entrapment syndromes, even without fractures.8
Fractures of the tibial tuberosity are uncommon and are involved in less than 1% of epiphyseal injuries and approximately 3% of all proximal tibial fractures.9 This type of fracture is more frequent in male adolescents.9 The Osgood-Schlatter lesion has been described as a predisposing factor for avulsive fractures of the tuberosity, and has been reported to occur in up to 23% of cases; however, further studies are still needed to fully determine this association (Fig. 6).10 The proximal physis of the tibia begins to close in a posterior to anterior fashion; therefore, a fracture pattern will depend upon the extent of skeletal maturity, as well as the degree of knee flexion at the time of injury. Generally, when an injury occurs with the knee in full extension, or close to 30° of flexion, avulsive fractures of the tuberosity occur without involvement of the proximal epiphysis of the tibia; when flexion exceeds 30°, both structures tend to sustain injury.10,11
Fig. 6.

X-ray of the knee of a 13-year-old boy presenting with an Ogden type IIIA fracture of the tibial tuberosity. The patient presented with Osgood-Schlater’s symptoms for three months prior to the injury.
Evaluation
The symptoms of tibial tuberosity fracture include the sudden onset of pain, usually during the start of a jump or sprint, an inability to move the knee and an inability to load and ambulate. Upon physical examination, swelling, effusion (haemarthrosis in Ogden type III fractures) and ecchymosis are normally evident. It is also important to identify the locations of specific pain and tenderness since the tibial plateau and the anterior tibial tuberosity are easy to palpate due to the minimum coverage of soft tissue.12,13 Deficiency of the extensor mechanism is usually present in Ogden type II and III fractures, but retinacular fibres and strong periosteal coverage can allow active extension. If possible, the stability of the knee should be evaluated with specific tests (including varus/valgus stress, anterior/posterior drawer and pivot-shift), taking into consideration that ligament injuries are uncommon. Owing to the anatomical proximity to the popliteal artery, evaluation of the vascular structures is mandatory. Popliteal artery entrapment syndromes have also been described following trauma in this area. Finally, it is important to monitor for increasing pain, which might be suggestive of compartment syndrome, taking into consideration the potentially fatal consequences of a delay in treatment.
Associated injuries
Several different lesions have been associated with this type of fracture, including meniscal injury, anterior cruciate ligament injury, patellar or quadriceps tendon avulsion and compartment syndrome (reports from 3–4%);14–16 these incidences were described in the literature prior to the use of arthroscopy or advanced imaging such as magnetic resonance imaging (MRI), with low incidence in clinical practice. Most meniscal injuries occur in type III and IV fractures, that is, with intra-articular involvement. Consequently, this type of injury should be investigated using additional techniques, such as MRI and mini-arthrotomy in order to manage the injury effectively.
The incidence of compartment syndrome is low, but can be devastating if not detected and treated properly. The mechanism involved has been described as a lesion of the recurrent branch of the anterior tibial artery that runs along the lateral border of the anterior tuberosity of the tibia (Fig. 7). Studies by Frey et al, and Palokoff et al, report that compartment syndrome occurs in 17–20% of cases.14,16 In contrast, in their systematic review, Pretell-Mazzini et al described an incidence of up to 4% preoperatively and 0% postoperatively, without association with fracture pattern.12 However, some studies have reported an association between compartment syndrome and both type III and IV fractures.12,13,15,16 We strongly recommend that physicians search directly for any evidence of compartment syndrome in any fracture during treatment.
Fig. 7.
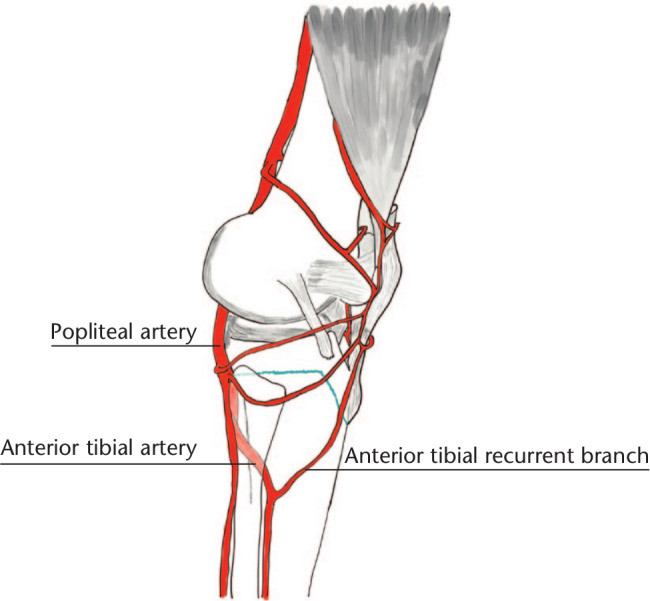
A schematic showing the relationship between proximal tibial fracture and the vascular bundle. The close relation with the popliteal artery explains the possible entrapment syndromes, while the lesion of the recurrent branch of the anterior tibial artery is associated with the incidence of compartment syndrome.
Imaging
In terms of imaging, frontal and lateral plain X-rays of the knee can provide important information with regard to the type of fracture and associated bony lesions. Radiological comparisons to the contralateral knee are also helpful in cases where the bone is immature and the specific features of fracture are doubtful or difficult to discern. When evaluating the lateral radiograph, it is important to verify the position of the patella, since a high position would indicate a potential tibial tuberosity fracture (Fig. 8). In a previous article, Pandya et al recommended the use of computer tomography (CT) for the preoperative evaluation of this type of fracture to determine the extent of the fracture, potential intra-articular involvement and to gain a better understanding of fragmentation (Fig. 9).17 MRI evaluation is not routinely used, but can be helpful in cases where there is a suspicion of non-displaced fractures or meniscal injuries.
Fig. 8.
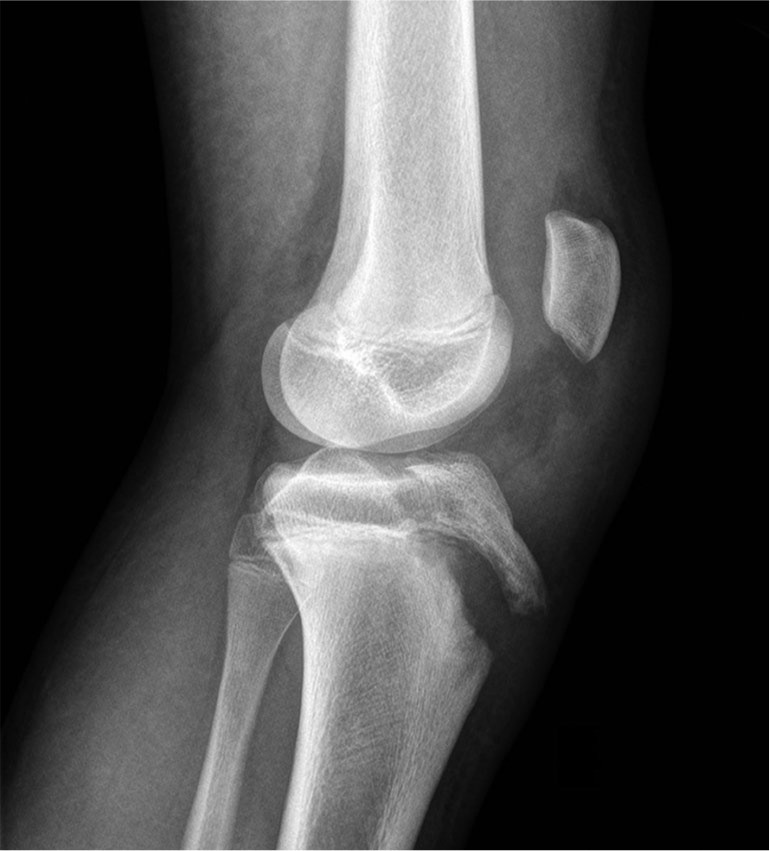
X-ray of the knee of a 14-year-old female presenting with an Ogden type IIIA fracture of the tibial tuberosity showing high patella positioning, haemarthrosis and intra-articular involvement.
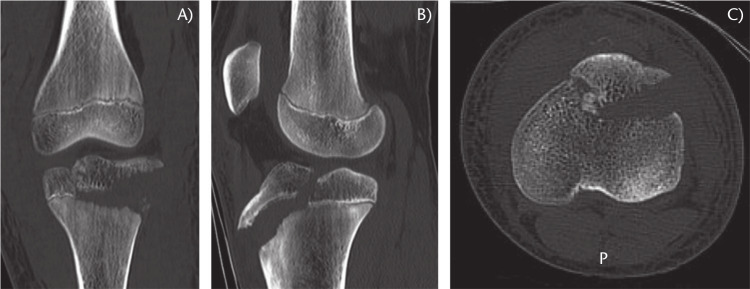
Fig. 9.
Computerized tomography (CT) scan of the knee of a 13-year-old male with an Ogden type IIIA fracture of the tibial tuberosity. Coronal (A), sagittal (B) and axial views (C) all demonstrate intra-articular involvement.
Classification
A variety of classification systems are available for this form of fracture (Fig. 10). The original classification system was put forward by Watson-Jones;18,19 however, the most popular system is currently the Ogden classification, which categorizes fractures according to the Watson-Jones criteria, but with additional ‘A’ and ‘B’ sub-modifiers.20 In 1985, Ryu et al added an additional sub-type (type IV) into the classification system; this relates to cases involving complete avulsion fracture of the proximal physis of the tibia (Fig. 11).21 In 2003, McKoy also added a ‘type V’ fracture to further classify an Ogden IIIB fracture which was associated with a Salter–Harris type IV fracture of the proximal tibia.22
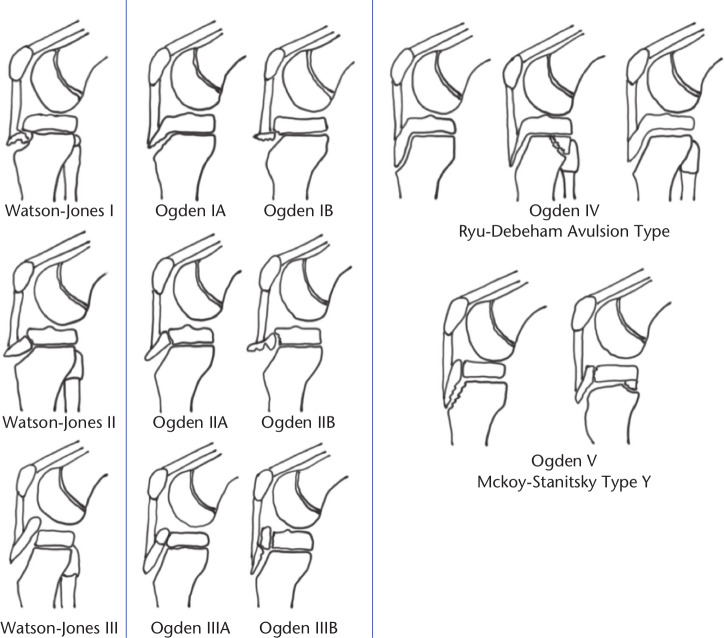
Fig. 10.
Classifications scheme for tibial tuberosity fractures.12,18–21 The Watson-Jones classification groups tibial tuberosity fractures into three types: type I, a small fragment with superior displacement; type II, a larger fragment involving the secondary centre of ossification and the proximal tibial epiphysis; type III, a fracture that passes proximally and posteriorly across the epiphyseal plate and proximal articular surface of the tibia (Salter–Harris type III). Ogden provided two further sub-classifications: type I, when only the distal portion of the tuberosity is injured; while type IA is a fracture through the tuberosity ossification centre with mild anterior displacement of the fragment, in type IB the fragment is separated from the metaphysis and may or may not also be separated from the rest of the secondary ossification centre. Type II injury involves the cartilaginous junction between two secondary ossification centres and usually leads to avulsion of the tuberosity ossification centre with variable involvement of the proximal tibial ossification centre. In type IIA, the tuberosity segment may fracture (usually a compression–impaction mechanism) at the juncture of the main tibial and tuberosity ossification centres. In type IIB, the fracture line propagates through a variably sized anterior portion of the proximal tibial ossification centre. Type III injuries involve significant separation of the fragments and propagation of the fracture line into the articular surface. Type IIIA is a unitary fracture while type IIIB is a comminuted fracture. Type IV is an avulsion of the entire tuberosity and proximal tibia epiphysis. Type V, as described by Mackoy, is an Ogden type III fracture associated with a Salter–Harris type IV fracture of the proximal tibia.
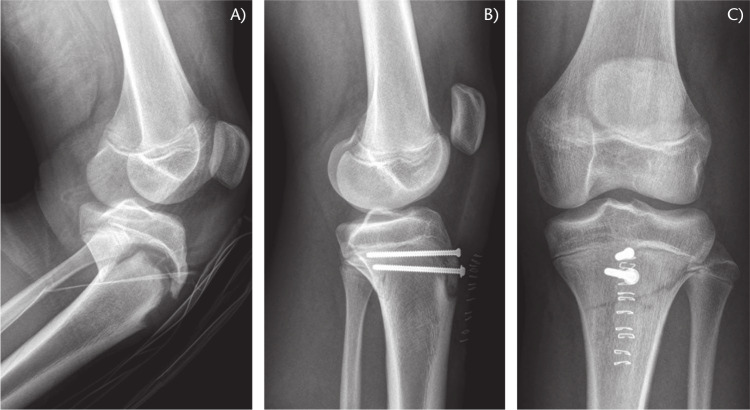
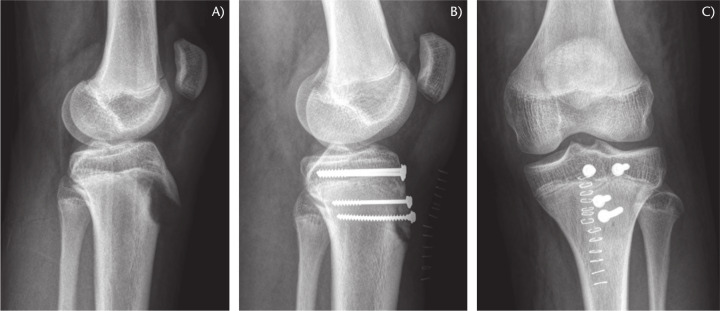
Fig. 11.
X-ray of the knee of a 14-year-old male presenting with an Ogden type IV fracture of the tibial tuberosity with complete proximal tibial epiphysis avulsion (A). Treatment involved open reduction and fixation with cannulated screws (B-C) and repair of the detached periosteum sleeve.
Treatment
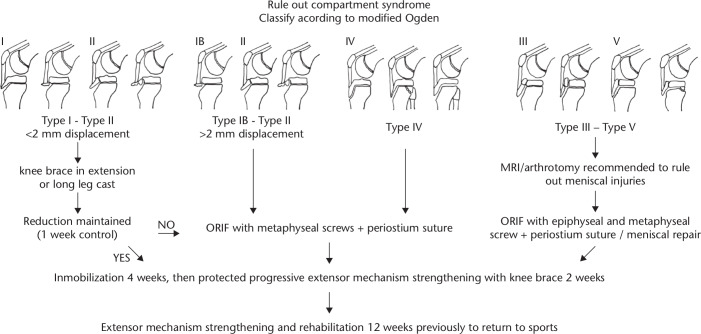
The objective of treatment is to restore the extensor mechanism of the knee, the joint surface and the meniscal anatomy when it is compromised. There are two possibilities for treatment: conservative management and surgical management (Fig. 12). When analysing the literature for the management of this type of fracture, we found that 88% of published cases were treated using surgical management, mostly via open reduction. This is because the decision-making process goes beyond the location of the fracture line, and also needs to consider displacement and associated injuries. Conservative management is performed by immobilizing the knee, in extension, for six weeks, using a knee brace in extension or a long leg cast. This treatment is usually deployed for Ogden type I or type II fractures with minimal displacement (< 2 mm), minimal displacement after closed reduction and cast application,22,23 or in very young children.
Fig. 12.
Suggested treatment algorithm for tibial tuberosity fracture.
Regardless of the system used to classify the fracture pattern, if an adequate reduction is not achieved, surgical management is advisable. There are several alternative treatments; the most commonly used option is open reduction with internal fixation. Another option is to use arthroscopy to facilitate anatomical reduction. Soft tissue repair is an option for cases involving only soft tissue avulsion fractures, or very young children.
Open reduction and internal fixation are performed through a midline incision in the knee, thus providing direct access to the fracture site.12,20,24 Direct evaluation and debridement of the fracture site, and the removal of any soft tissue interposition (mainly the periosteum) is mandatory to achieve complete anatomical reduction of the fracture fragments. Internal fixation with cancellous partially threaded screws is recommended in order to achieve good compression of fracture lines (Fig. 13). Ideally, 4.0 mm screws are recommended as they reduce the soft tissue irritation which can occur with larger screws over the long term. A K-wire is a useful option for children who are less than three years of age. The use of cannulated screws as a method of fixation for avulsed fractures has been shown to be superior to the use of percutaneous K-wires.12 These screws offer greater compression and rigidity than the fixation method, thus allowing an earlier joint range compared with immobilization in conservative management. However, these screws are associated with soft tissue irritation that requires hardware removal.12,13 We always recommend suturing the periosteum and the compromised extensor mechanism in cases involving extensive avulsion of the anterior tibial tuberosity, as this may allow earlier rehabilitation.
Fig. 13.
X-ray of a 15-year-old male’s knee presenting with an Ogden type IIIA tibial tuberosity fracture (A). Treatment involved open reduction and fixation with inter-fragmentary compression screws through an anterior approach, with repair of the periosteum sleeve (B, C).
Open reduction can be achieved by either direct arthrotomy or arthroscopic view; the former method is advantageous because it offers the possibility of treating fractures with intra-articular extension and associated soft tissue injuries. The disadvantage of arthrotomy, however, is that it requires more time for immobilization and rehabilitation. When considering arthroscopy, it is important to take into account that this method is technically challenging and has been associated with a higher risk of compartmental syndrome in tibial plateau fractures.25,26
Post-treatment recommendations include protection of the knee with a non-weight-bearing long leg cast or brace for four to six weeks, progressive extensor mechanism strengthening and a three-month period of rehabilitation before returning to sports activities. Patients with a very immature skeleton can be treated using soft tissue repair for ‘sleeve’ fractures, with periosteal sutures and immobilization for eight weeks. This option requires a prolonged healing time in order to allow healing of the soft tissue but shows good to excellent results in young children.22
Results and outcomes
Independent of the type of management deployed, the literature generally shows excellent results. For example, one study reports complete consolidation in 99% of cases, with 98% of patients returning to normal activities in an average of 29 weeks; complete range of motion was achieved in 97% of patients.12 The mean incidence of complications is close to 28% with most complications (56%) related to anterior knee pain due as a result of implant irritation or bursitis. However, such complications are considered minor and a second surgical intervention for implant removal has only been described in 7% of patients suffering from complications.10 Refracture has been reported to occur in 6% of cases and is more frequent in type III, IV and V fractures due to the involvement of the entire physis. Genu recurvatum is a rare complication and occurs in less than 4% of cases,12 most likely due partial growth arrest of the proximal tibia physis.27,28
Conclusions
Fractures of the anterior tibial tuberosity can generally be treated successfully; however, the selected management plan must be correctly indicated and should respect the principles of treatment required by the particular fracture type. Fractures that compromise the joint surface have a greater association with other types of lesions; these patients should therefore be evaluated carefully, and physicians should consider the use of direct exploration. The incidence of complications is low and does not affect the functional outcome of the course of treatment. However, further studies are now required to fully investigate the treatment of these fracture types, particularly over the long term.
Acknowledgements
The authors would like to acknowledge the help provided by the Vicerrectoría de Investigación, Desarrollo y Creación Artística of the Universidad Austral de Chile in order to publish this work.
Footnotes
ICMJE Conflict of interest statement: The authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1. Peterson H. Proximal tibia. In: Peterson H, ed. Epiphiseal growth plate fractures. Berlin: Springer, 2007:651–694. [Google Scholar]
- 2. Kuhns LR, Finnstrom O. New standards of ossification of the newborn. Radiology 1976;119:655–660. [DOI] [PubMed] [Google Scholar]
- 3. Beaty JH, Kumar A. Fractures about the knee in children. J Bone Joint Surg Am 1994;76:1870–1880. [DOI] [PubMed] [Google Scholar]
- 4. Gill JG, Chakrabarti HP, Becker SJ. Fractures of the proximal tibial epiphysis. Injury 1983;14:324–331. [DOI] [PubMed] [Google Scholar]
- 5. González-Herranz P. Proximal epiphyseal tibial fractures. In: de Pablos J, ed. The immature knee. Barcelona: Biblio STM, 1998:204–211. [Google Scholar]
- 6. Nolan RA, Meyers MH, Patzakis MJ, Moore TM, Harvey JP., Jr Tibial epiphyseal injuries. Contemp Orthop 1978;1:11–22. [Google Scholar]
- 7. Nelson GE, Jr, Kelly PJ, Peterson LFA, Janes JM. Blood supply of the human tibia. J Bone Joint Surg Am 1960;42-A:625–636. [PubMed] [Google Scholar]
- 8. Cummings RJ, Webb HW, Lovell WW, Kay G. The popliteal artery entrapment syndrome in children. J Pediatr Orthop 1992;12:539–541. [DOI] [PubMed] [Google Scholar]
- 9. Edmonds EW, Mubarak SJ. Proximal tibial physeal fractures. In: Flynn JM, Skaggs DL, Waters PM, eds. Rockwood and Wilkins’ fractures in children. Eighth ed. Philadelphia, PA: Wolters Kluwer Health, 2015:1057–1074. [Google Scholar]
- 10. Jakoi A, Freidl M, Old A, Javandel M, Tom J, Realyvasquez J. Tibial tubercle avulsion fractures in adolescent basketball players. Orthopedics 2012;35:692–696. [DOI] [PubMed] [Google Scholar]
- 11. Borch-Madsen P. On symmetrical bilateral fracture of the tuberositas tibiae and eminentia intercondyloidea. Acta Orthop Scand 1954/1955;24:44–49. [DOI] [PubMed] [Google Scholar]
- 12. Pretell-Mazzini J, Kelly DM, Sawyer JR, et al. Outcomes and complications of tibial tubercle fractures in pediatric patients: a systematic review of the literature. J Pediatr Orthop 2016;36:440–446. [DOI] [PubMed] [Google Scholar]
- 13. Little RM, Milewski MD. Physeal fractures about the knee. Curr Rev Musculoskelet Med 2016;9:478–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Frey S, Hosalkar H, Cameron DB, Heath A, David Horn B, Ganley TJ. Tibial tuberosity fractures in adolescents. J Child Orthop 2008;2:469–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Brey JM, Conoley J, Canale ST, et al. Tibial tuberosity fractures in adolescents: is a posterior metaphyseal fracture component a predictor of complications? J Pediatr Orthop 2012;32:561–566. [DOI] [PubMed] [Google Scholar]
- 16. Polakoff DR, Bucholz RW, Ogden JA. Tension band wiring of displaced tibial tuberosity fractures in adolescents. Clin Orthop Relat Res 1986;209:161–165. [PubMed] [Google Scholar]
- 17. Pandya NK, Edmonds EW, Roocroft JH, Mubarak SJ. Tibial tubercle fractures: complications, classification, and the need for intra-articular assessment. J Pediatr Orthop 2012;32:749–759. [DOI] [PubMed] [Google Scholar]
- 18. Mostofi SB. Fracture classifications in clinical practice. London: Springer-Verlag London, 2006. [Google Scholar]
- 19. Ogden JA. Skeletal injury in the child. Third ed. New York: Springer-Verlag, 2000. [Google Scholar]
- 20. Ogden JA, Tross RB, Murphy MJ. Fractures of the tibial tuberosity in adolescents. J Bone Joint Surg Am 1980;62:205–215. [PubMed] [Google Scholar]
- 21. Ryu RK, Debenham JO. An unusual avulsion fracture of the proximal tibial epiphysis. Case report and proposed addition to the Watson-Jones classification. Clin Orthop Relat Res 1985;194:181–184. [PubMed] [Google Scholar]
- 22. McKoy BE, Stanitski CL. Acute tibial tubercle avulsion fractures. Orthop Clin North Am 2003;34:397–403. [DOI] [PubMed] [Google Scholar]
- 23. Abalo A, Akakpo-numado KG, Dossim A, Walla A, Gnassingbe K, Tekou AH. Avulsion fractures of the tibial tubercle. J Orthop Surg (Hong Kong) 2008;16:308–311. [DOI] [PubMed] [Google Scholar]
- 24. Riccio AI, Wilson PL, Wimberly RL. Lower extremity injuries. In: Herring JA, ed. Tachdijan’s pediatric orthopaedics: from the Texas Scottish Rite Hospital for Children. Fifth ed. Philadelphia, PA: Elsevier Health Sciences, 2013:1353–1516. [Google Scholar]
- 25. Belanger M, Fadale P. Compartment syndrome of the leg after arthroscopic examination of a tibial plateau fracture. Case report and review of the literature. Arthroscopy 1997;13:646–651. [DOI] [PubMed] [Google Scholar]
- 26. Weinlein J, Schmidt A. Acute compartment syndrome in tibial plateau fractures—beware! J Knee Surg 2010;23:9–16. [DOI] [PubMed] [Google Scholar]
- 27. Nathan ST, Parikh SN. Genu recurvatum after tibial tuberosity fracture. Case Rep Orthop 2013;2013:952978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Olerud C, Danckwardt-Lillieström G, Olerud S. Genu recurvatum caused by partial growth arrest of the proximal tibial physis: simultaneous correction and lengthening with physeal distraction. A report of two cases. Arch Orthop Trauma Surg 1986;106:64–68. [DOI] [PubMed] [Google Scholar]