Abstract
Sacral fractures are a heterogeneous group of fractures occurring in young people following road traffic accidents and falls from height, or in the elderly with osteoporosis following trivial trauma.
This heterogeneity, combined with the low incidence of sacral fractures, determines a lack of experience amongst physicians, often leading to misdiagnosis, underestimation and inadequate treatment. The diagnosis should be made by assessing specific features during the clinical presentation, while computed tomography (CT) scan continues to be the choice of investigation.
Sacral fractures can be treated non-operatively or surgically. Non-operative treatment is based on rest, pain relief therapy and early mobilization as tolerated. Surgical techniques can be split into two main groups: posterior pelvic fixation techniques and lumbopelvic fixation techniques. Anterior pelvic fixation techniques should be considered when sacral fractures are associated with anterior pelvic ring injuries, in order to increase stability and reduce the risk of posterior implant failure. To improve fracture reduction, different solutions could be adopted, including special positioning of the patient, manipulation techniques and use of specific reduction tools. Patients suffering from spinopelvic dissociation with associated neurologic lesions hardly ever recover completely, with residual lower-limb neurologic sequelae, urinary problems and sexual disfunction.
Herein, we present issues, challenges and solutions related to the management of sacral fractures.
Cite this article: EFORT Open Rev 2020;5:299-311. DOI: 10.1302/2058-5241.5.190064
Keywords: fixation, lumbopelvic fixation, neurological lesion, sacral fracture
Introduction
The os sacrum is the hinge between the vertebral column and the pelvic ring, supporting the upper body weight and playing a fundamental role in giving stability to the pelvic ring during load-bearing.1 It is in contact with several critical structures such as nerves, blood vessels, urogenital and other pelvic organs. A fracture of the sacrum is therefore troublesome as it determines an impairment in ambulation and it may present various associated lesions.
Sacral fractures are a heterogeneous group of fractures occurring in young people following road accidents and falls from height or in the elderly with osteoporosis following trivial trauma. The incidence of non-osteoporotic sacral fractures has been reported as 2.1 cases per 100,000 people, while osteoporotic fractures have been reported to have an incidence of 1–5% in elderly patients at risk.2–4 Both fracture groups are reported to be increasing: non-osteoporotic has tripled in the decade between 2002 and 2011 and the incidence of osteoporotic fractures is also increasing because of the aging of the population, with the prospect of continuing to further increase in the coming years.1,2,5 However, the reported growth must also be attributed to the greater and more widespread use of computed tomography (CT) scan, which allows a higher rate of diagnosis.6 This heterogeneity, combined with the low incidence of sacral fractures, determines a lack of experience amongst physicians, often leading to misdiagnosis, underestimation and inadequate treatment.7 Good knowledge of sacral fractures and their characteristics is therefore essential to correctly diagnose and manage these patients, in order to competently deal with both simple and complex fractures.
This review aims to highlight recent advances in diagnosis, management and treatment of this challenging fracture group.
Classification
Many classifications have been proposed to describe sacral fractures; however, being a heterogeneous group of injuries, none of these is really able to take into account all the possible variables that could characterize a sacral fracture.8 Current classification systems can be presented in terms of:
a) The energy of trauma sustained: high-energy (young patients) or low-energy fractures (elderly);7 insufficiency fractures (secondary to radiation or frailty)9 and stress fractures (young athletes).10
b) Association with pelvic ring injuries (isolated accounting for up to 10–13% of all sacral fractures11,12 or associated with pelvic injury (up to 80–90%).13 The classification systems broadly utilized to describe sacral fractures in the context of pelvic ring injuries are the Arbeitsgemeinschaft für Osteosynthesefragen/Orthopaedic Trauma Association ( AO/OTA) modified Tile (AO/OTA) classification13 and Young–Burgess (YB) classification,14 for high-energy fractures, and the Fragility Fracture of Pelvic ring (FFP) classification,15 for low-energy fractures. The AO/OTA classification classifies the fracture according to pelvic ring stability, while the YB takes into account the fracture resulting from the different displacing vectors: anterior-posterior compression (APC), lateral compression (LC), vertical shear (VS). FFP classification divides fractures according to morphology and instability.
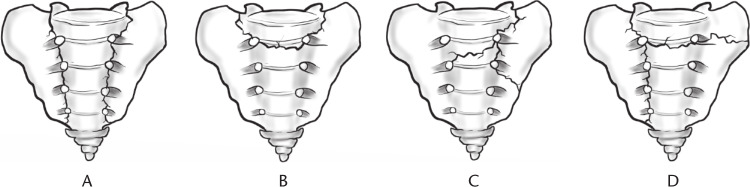
c) Morphology describes the orientation of the fracture lines with regard to the sacral bone (longitudinal, transverse or combined as H-, U-, lambda- or T-shaped). Longitudinal fractures are the most common (90%),11 transverse fractures represent only 3–5% (divided into high or low),16 combined fractures such as U-, H-, lambda- or T-shaped (3–6%)17,18 characterize a specific condition known as spinopelvic dissociation, also described in cases of bilateral longitudinal fractures (Fig. 1).19 Normally the transverse fracture line is high and the longitudinal is transforaminal or medial to the foramina.18,20 Occasionally fractures can result from low-energy trauma, causing a U- or H-shaped insufficiency fracture still with a high level of intrinsic instability.21 Recently, a new classification for insufficiency fractures of the sacrum has been proposed, which divides fractures according to morphology, in order to predict the risk of cement leakage during sacroplasty.22
d) Location of fracture: Denis classification,23 divides the sacrum into three zones. Zone I includes the sacral ala lateral to the foramina, zone II the foramina and zone III the sacral canal medial to the neural foramina (Fig. 2). Zone I fractures (most common location for low-energy fractures)24 have a 6% risk of neurologic injury (L5 radiculopathy). Zone II fractures (can be haemodynamically unstable because of the damage to the lateral and medial sacral arteries)25 have a 28% risk of neurologic injury. Zone III fractures have a 56% risk of neurologic injury (cauda equina syndrome).23 The modified Roy-Camille classification26 describes transverse fractures of the upper sacrum above S4 and divides them according to their displacement. These fractures have been typically considered to affect Zone III.16 Modified Roy-Camille includes four different types of fractures with different risks of neurologic lesions, types I and II being the most common (93%), types III and IV less common (7%) (Fig. 3).27 Isler also classified sacral fractures following the location criteria, in particular with respect to the L5–S1 facet, which together with lumbosacral posterior ligaments and sacroiliac joints, determines spondilopelvic stability.28 He identified longitudinal transforaminal fractures and divided them into three types: type I stable lateral to the facet, type II unstable at the level of the facet, and type III highly unstable medial to the facet constituting a sort of spinopelvic dissociation.29
Fig. 1.
The four combined sacral fracture types: (A) H-shaped; (B) U-shaped; (C) Lambda-shaped (λ); (D) T-shaped.
Fig. 2.
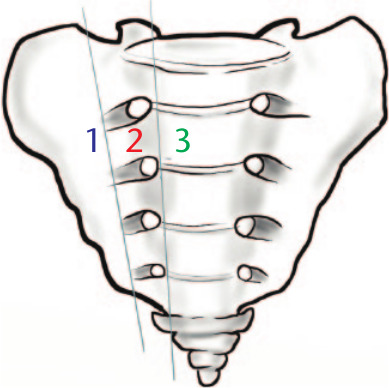
The Denis classification: zone I fracture involves the sacral ala lateral to the foramina; zone II fracture at the level of the foramina; zone III fracture affects the sacral canal medial to the neural foramina.
Fig. 3.
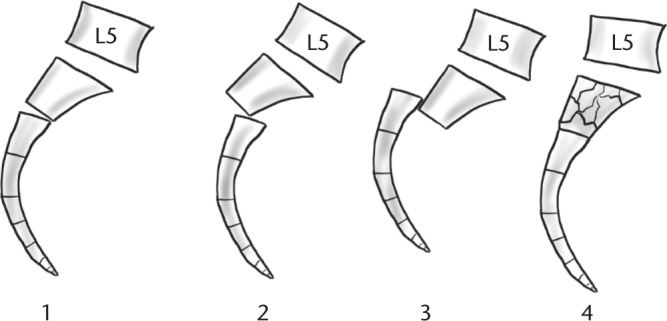
The Roy-Camille classification: type I fractures show kyphotic angulation only; type II fractures demonstrate both kyphosis and retrolisthesis; type III fractures have complete anteriorlisthesis; type IV fractures characterized by severe comminution of the S1 body.
Diagnosis
Clinical
Sacral fracture diagnosis is often troublesome, with a rate of missed or delayed diagnosis ranging from 25% to 70%.30,31 Overall the diagnosis should be made by assessing specific features during the clinical presentation particularly after high-energy trauma (buttock pain, bruising, swelling and laceration over the sacral area, perineal and genitalia sensibility, sphincter tone malfunction, neurological deficit of lower extremities, presence of Morel-Lavallée lesion). Patients suffering from a sacral low-energy fracture are characterized by an unspecific clinical presentation (complain about ambiguous low back pain, which increases with axial load or activities, mimicking the pain from lumbar stenosis or metastasis, generally without radiculopathy).32,33 Sacral stress fractures are typically seen in athletes reporting low back pain in absence of trauma.34
Active bleeding must be promptly identified and addressed (derives from medial and lateral sacral arteries, presacral venous plexus, superior gluteal artery and iliac arteries).25,35 Pelvic stabilization with a pelvic binder, a sheet or an external fixator is essential if bleeding is related to pelvic instability. In the case of persistent haemodynamic instability or bleeding from isolated sacral fractures, pelvic packing or embolization must be considered.36
Of note is that 62% of transverse fractures are associated with spine lesions, 25% with thoracolumbar lesions, and 11% with lumbosacral lesions, particularly related to high-energy trauma, able to disrupt the robust lumbosacral ligaments.31 Insufficiency fractures could be associated with vertebral compression fracture.37
Radiological
Plain radiographs (anteroposterior [AP] pelvis, inlet/outlet views) are the first line of investigation, but could miss up to 50% of sacral fractures. Inlet and outlet views could be combined with standard AP view in order to improve the X-ray sensitivity. Both direct and indirect signs of sacral fractures must be looked for on X-rays, such as paradoxical sign, an AP view resembling an inlet view due to an inclination of the proximal sacrum following a transverse fracture, and fracture of the L5 transverse process, indicative of pelvic instability, respectively.38 If the X-ray is negative, and pain persists, a CT scan should always be performed, or a magnetic resonance imaging (MRI) scan. Nowadays in our institution the first line of investigation in patients presenting with fractures of the anterior elements of the pelvic ring is a CT scan, which is able to detect sacral fractures with a reported sensitivity of 68-88%.39,40 MRI has the highest sensitivity (98%).40,41 It is able to diagnose occult fractures missed by CT because of intact cortices.34 It can detect bone edema of the cancellous bone, bone-bruise and fracture line as a line of hypointensity.33,42 Furthermore, sacral insufficiency fractures could be associated with malignancy, in some series in up to 45% of cases.43 MRI could help in differential diagnosis by detecting the bone edema which is sign of infection or tumour which must be excluded.44 When a stress fracture is suspected, MRI is the indicated exam, followed by a bone scan and CT scan respectively.45 Bone scintigraphy can help in the diagnosis of low-energy sacral fractures, having high sensitivity but lower specificity than MRI.46 Single Photon Emission Computed Tomography (SPECT/CT) allows not only identification of the fracture but also diagnosis of its age.47–49
Principles of management
Presence of instability, displacement, association with pelvic ring damage and neurologic injury determine the need for operative treatment.30,50 Non-displaced isolated high transverse fractures, or fractures below the sacroiliac joint level (S3/S4–S5) are normally considered stable, along with longitudinal incomplete fractures. Complete longitudinal fractures and displaced transverse fractures are considered unstable and require surgical fixation.7 The same is true for U-shaped fractures characterized by spinopelvic instability, and U-shaped insufficiency fractures, which would usually require surgical fixation as they present an intrinsic instability which could lead to a progressive kyphotic deviation and delayed neurological sequelae.21,51 A displacement greater than 10 mm indicates surgical treatment.36 As for association with high-energy pelvic ring injury, AO/OTA type A injuries, and some non-displaced cases of LC injuries are considered stable and should be managed conservatively.52,53 AO/OTA type B displaced and type C injuries, however, require surgical fixation since they are unstable.36 In the elderly, according to the FFP classification, FFP II injuries could be conservatively treated as the fractures are usually stable enough to permit early mobilization of the patient, while FFP III and IV are unstable and should be surgically stabilized.5 Surgical treatment of neurologic injury is controversial. A lesion above S4 presenting with cauda equina syndrome, often owing to zone III fractures, would call for direct or indirect surgical decompression, even if diagnosed late. Indeed, when faced with fracture fragments encroaching onto the sacral canal or compressing neural roots, responsible for neurologic deficit, surgical reduction is indicated. However, with regard to other neurologic lesions, a surgical decompression is not guaranteed to produce a better outcome than non-surgical treatment.36,54
Recently, a lumbosacral injury classification system (LSICS) has been developed to help clinical decision. It focusses particularly on complex injuries, giving each fracture a score ranging from 0 to 10, based on fracture morphology, ligament injury and neurologic injury, where less than 4 indicates conservative treatment and above 4 indicates surgical stabilization.55
Treatment
Sacral fractures can be treated non-operatively or surgically. Non-operative treatment is based on rest, pain relief therapy and early mobilization as tolerated. In high-energy fractures, it is indicated in the case of low transverse fractures, marginal avulsions or stable non-displaced longitudinal fractures of the sacral ala, isolated or associated with stable LC pelvic injuries.52,53 Nonetheless, some authors have proposed the surgical treatment of anteriorly displaced low transverse fractures associated with neurologic injury.56 Conservative treatment of insufficiency fractures is considered for stable non-displaced or incomplete fractures, isolated or associated with anterior pubic rami fractures in the context of FFP II. If conservative treatment fails, surgical treatment must be considered.5 The use of calcium and vitamin D drug supply, bisphosphonates, and teriparatide enhances the healing process and improves pain relief.5,42,57
Treatment of stress fractures consists of rest for around six weeks from high-impact sports or activities and benefits from medical therapy such calcium or vitamin D intake in some cases associated with Parathyroid hormone (PTH) over a period of 3–6 months.58
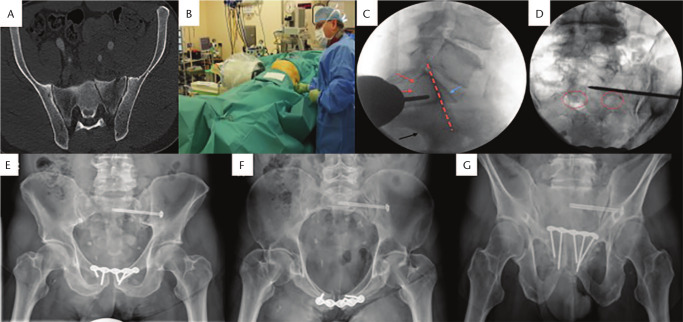
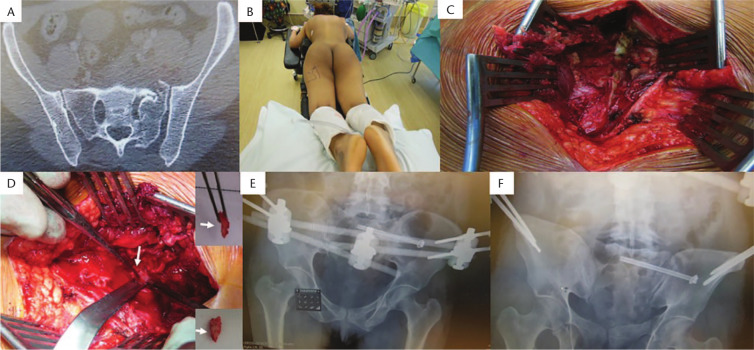
Surgical techniques can be split into two main groups: posterior pelvic fixation techniques and lumbopelvic fixation techniques (Figs 4, 5, 6, 7 and 8).59 If the fracture is associated with pelvic ring injury, anterior pelvic fixation techniques can be performed.60 Posterior pelvic fixation techniques connect the ilium to the sacrum. They can be performed either percutaneously or in an open manner. Among the percutaneous techniques, iliosacral screw fixation is the most common technique used.61 It is characterized by cannulated screw insertion through the safe corridor of S1 or S2 body, the latter being associated with higher malpositioning rates.62 In some cases, where required, the use of the S3 corridor has been described.63 In osteoporotic fractures, iliosacral screws can be augmented with cement to increase the stability of the implant.1,64,65 Sacroplasty is an alternative to iliosacral screw for sacral ala incomplete insufficiency fractures and consists of percutaneous cement injection into the fracture site for pain relief and stability restoration.66
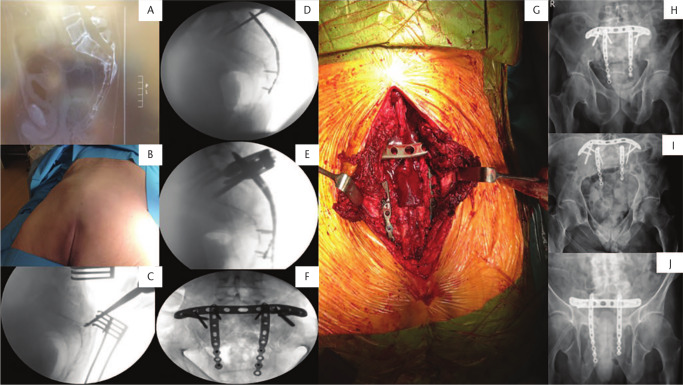
Fig. 4.
(A) Axial CT scan showing Dennis I fracture over left sacral ala; (B) Patient in supine position, under fluoroscopic control and left buttock stab incision, surgeon tries to identify correct position of guide wire for sacral body 1 screw insertion; (C) Lateral fluoroscopic image demonstrating upper end of the first sacral vertebra (blue arrow), the iliac cortical density (red line), the greater sciatic notch (black arrow) and the upper nerve root tunnel (red arrows); (D) S1 sacral foramina are demonstrated by red circles. Guide wire for screw insertion is positioned above left S1 foramen; (E) Postoperative anteroposterior (AP) pelvic radiograph; (F) inlet and (G) outlet views demonstrating fixation of the pelvic ring (injury to pubis symphysis was addressed with a plate).
Fig. 5.
(A) Axial computed tomography (CT) pelvic slice showing Denis II fracture with a small bone fragment in the Sacral 1 (S1) foramen causing S1 nerve root compression. (B) Patient positioned in prone position. (C) Midline exposure and for decompression of the nerve root. (D) Bony fragment removal (arrows). (E and F) Pelvic ring fracture was fixed with left SI sacroiliac screw and an anterior external fixator frame for the pubic rami fracture.
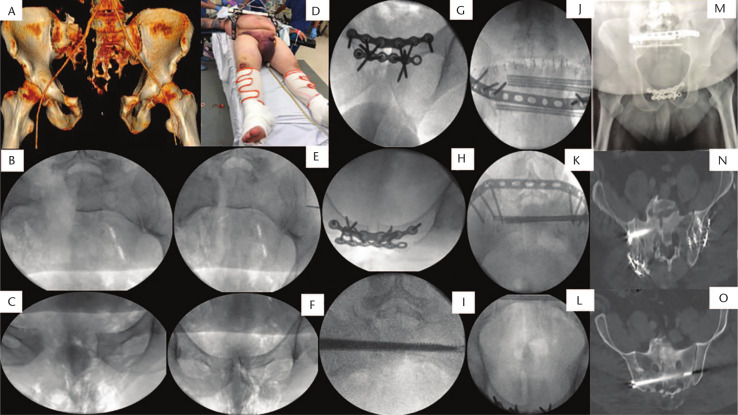
Fig. 6.
(A) Three-dimensional pelvic image of a male patient sustaining after motorcycle accident an anteroposterior (AP) III injury with sacral fracture through body of S1 (Dennis III sacral fracture). (B) Fluoroscopic inlet view showing sacral fracture displacement. (C) Fluoroscopic AP pelvic view showing pubis diastasis anteriorly. (D) Intraoperative picture showing application of C-clamp and anterior external fixator for initial temporarily stabilization of the pelvic ring. (E) Fluoroscopic pelvic inlet view showing reduction of the sacral fracture. (F) Fluoroscopic AP pelvic view showing reduction of the pubic diastasis anteriorly. (G) Fluoroscopic AP view showing fixation of the pubis symphysis with two plates. (H) Fluoroscopic inlet pelvic view showing fixation of pubis symphysis with two plates. (I) Fluoroscopic inlet pelvic view showing insertion of S1 sacroiliac (SI) screws. (J) Fluoroscopic pelvic outlet view showing fixation of the sacrum with two SI screws and one S2 screw and a tension band plate. (K) Fluoroscopic pelvic inlet view showing fixation of the sacrum with two SI screws and one S2 screw and a tension band plate. (L) Fluoroscopic pelvic inlet view showing symmetric pelvic ring. (M) AP postoperative pelvic radiograph showing reconstruction of the ring anteriorly and posteriorly. (N) Axial cut of pelvic computed tomography (CT) scan showing reduction of the sacral fracture and safe placement of S1 screws. (O) Axial cut of pelvic CT scan showing safe placement of S2 screw.
Fig. 7.
(A) Lateral sacral radiograph showing a U-type fracture. Patient presented with full sacral plexus neurological symptoms, incontinence. Underwent diverting stoma post decompression of spinal canal and orif with tension band plate and bilateral sacral wing locking plates to address vertical fracture plane at levels of S1–S3. (B) Prone position of patient. (C) Fluoroscopic image for identification of the fracture level and decompression. (D) Lateral fluoroscopic image showing application of sacral wing plates and insertion of sacroiliac (SI) body screw. (E) Lateral fluoroscopic view showing fixation of sacral fracture with tension band plate and bilateral sacral wing locking plates. (F) Fluoroscopic outlet view showing fixation of fracture. (G) Intraoperative picture showing midline incision and application of plates. (H) Anteroposterior, (I) inlet, and (J) outlet pelvic postoperative radiographs showing stabilization of the ring posteriorly.
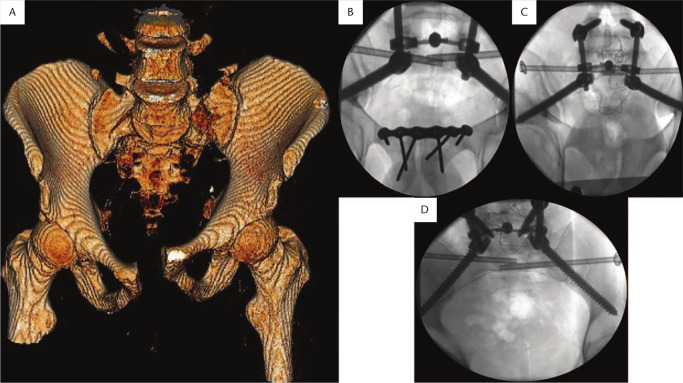
Fig. 8.
(A) Three-dimensional pelvic model showing bilateral sacral fractures and pubis diastasis anteriorly. (B) Anteroposterior, (C) outlet, and (D) inlet fluoroscopic views showing stabilization of the fracture with spinopelvic fixation and sacroiliac screws to S1 body (triangular configuration). Pubis symphysis was stabilized with plating anteriorly.
Transsacral implants, such as transiliac-transsacral screws or transsacral bars, are alternative percutaneous techniques in which a long-threaded implant passes all the way across the S1 or S2 corridor to the contralateral ilium.67 Transiliac bridging systems are minimally invasive techniques which connect the back side of the left and right ilium with a plate fixed with screws or a bar fixed with pedicle screws and introduced subcutaneously behind the sacrum by bilateral limited incisions, acting as transiliac internal fixators.68–71 The addition of an S1 pedicle screw in direct contact with the fracture has recently been proposed in the ‘within ring’-based sacroiliac rod fixation system.72 In addition, other minimally invasive surgical techniques, such as tension band plate, and adjustable plate, have been described to address some of the drawbacks of iliosacral screws.73 Other posterior sacroiliac open techniques that have been described include Beaujon’s sacroiliac assembly, and the Pitiè-Salpetriere shortening osteotomy.74,75
Lumbopelvic fixation techniques connect the lumbar spine to the ilium. The lumbar-iliac technique is performed in an open manner and links the lower vertebral bodies with the ilium using bilateral pedicle screws connected with bars. In cases of high degree of instability, a more stable construct is obtainable connecting both L4 and L5 to the ilium; alternatively fixation from L5 to the ilium could be sufficient.76 Similarly, the iliac screws are usually single but have also been known to be double.77 If the above-mentioned lumbar-iliac technique is combined with iliosacral screws or transiliac plate, it makes up the triangular osteosynthesis assembly, originally proposed as unilateral but also described as bilateral with greater stability, representing the most stable technique for the stabilization of the dorsal pelvic ring, especially in osteoporotic bone.78–81
Anterior pelvic fixation techniques should be considered when sacral fractures are associated with anterior pelvic ring injuries, in order to increase stability and reduce the risk of posterior implant failure. They include retrograde transpubic screw, anterior internal fixator, or plate and screws.17,82
Overall, indications and aims of surgical treatment are different depending on the energy of the fracture. In high-energy fractures, the objective of surgery is anatomic reduction and restoration of stability by rigid fixation, while in low-energy ones the objective is restoration of stability with a rigid fixation as minimally invasive as possible, with reduction becoming less relevant.5
Following high-energy trauma, longitudinal sacral fractures isolated or most commonly associated with a rotationally unstable AO/OTA B pelvic ring injury, if successfully reduced with external manoeuvres, can be treated using uni- or bilateral iliosacral screw, or transiliac bridging system in cases where iliosacral screw is not feasible.83,84 When the obtained closed reduction is not sufficient, open reduction and internal fixation is required. When longitudinal fractures are associated with vertically unstable AO/OTA C injuries, although different fixation methods have been proposed, lumbopelvic implants, associated with anterior fixation, are those which provide the highest stability to counteract shear forces.85,86 High transverse sacral fractures (U- or H-shaped) can be treated with bilateral ileosacral or transsacral-transiliac screw in the case of a transverse component classifiable as Roy-Camille type I. In Roy-Camille II or III injuries, open reduction and decompression is required if neurologic injury is present.
In low-energy fractures, sacral ala fractures are treated with iliosacral screw fixation, feasible in both the S1 and S2 corridor.87,88 Sacroplasty is indicated as an alternative to iliosacral screw in incomplete sacral ala fractures without the interruption of bone cortices.66 In the case of displaced transverse fracture or association with neurologic injury, on the other hand, treatment should be performed in an open manner using lumbopelvic fixation, triangular osteosynthesis having shown the highest stability.5,81,89
Complications
Treatment of sacral fractures is challenging as it presents a wide range of complications with reported rates of up to 40–50% of cases in certain fracture types.90 Perioperative complications include implant malpositioning (15%),91,92 neural lesions of L4–L5, S1 roots (2–15%),92 blood loss in open approaches,93 superior gluteal artery damage (1.2%), and ureteral damage and bowel lesion, which is a rare scenario.75,94 Postoperative complications include infection (low with minimally invasive or percutaneous techniques60,73,86 but rising to up to 50% with open lumbopelvic fixation, and up to 20% if treated with plates);74,95 wound healing problems;93,96,97 instrumentation failure (11–17%);85 soft tissue irritation requiring implant removal;74,98,99 cement leakage after sacroplasty100,101 and cerebrospinal fluid leakage.75
Outcomes
Functional outcome
The clinical outcome of high-energy fractures is related to the severity of initial trauma. Series of patients after spinopelvic dissociation have shown poor clinical outcome in up to 42% of cases, directly related to the degree of initial displacement and bad long-term outcomes with a patient-reported health score lower than that of the general population, with no improvement from the one-year to 10-year follow-up.102–104 Similarly, chronic residual pain is especially frequent after vertical unstable fractures or spinopelvic dissociation, where it has been found to persist in up to 100% of patients, also in long-term follow-up.96,102,103 However, after 10 years, patients have shown a significant recovery in independence of daily activities compared with at one-year follow-up.103 Regarding the fixation technique, iliosacral screws have better results in terms of early return to everyday activities compared to posterior plates, and satisfactory surgical outcomes even when treating AO/OTA type B or C unstable injuries, without the advantage of the use of a second screw.69,105 Low-energy fractures are related to high mortality rates, with a 12-month mortality of 28% and loss of pre-morbidity abilities in 34% of cases.106,107 Patients suffering from sacral insufficiency fractures, if operated, present a higher rate of return to pre-injury level than conservatively treated patients, with a significant reduction of postoperative pain.88,108 Isolated insufficiency fractures, if treated with a posterior transiliac-transsacral screw, have shown a 75% rate of returning home compared to 20% of conservatively treated patients, and a 100% ability to ambulate compared to 70% of non-operated patients.109
Fracture healing
A sacral fracture takes 8–12 weeks to heal and fusion rates following sacral fractures have been reported to be 85–90%.6,105 Malunion can occur after delayed treatment or insufficient reduction, with a consequent alteration of pelvic incidence. This is more frequent with Roy-Camille II and III fractures and in the case of spinopelvic dissociation.102,104 After spinopelvic dissociation injuries, the restoration of the lumbosacral orientation is crucial, otherwise a sagittal imbalance will occur, with a deterioration of functional outcome and chronic back pain.110,111
Neurologic recovery
As for clinical outcome, prognosis of neurologic injury is strictly related to the severity of the sacral fracture. It has recently been shown how in a sacral fracture combined with lumbar plexus injury, the higher the instability, the poorer the neurological recovery will be, with an impact on gait outcomes.112 Accordingly, patients suffering from spinopelvic dissociation with associated neurologic lesions hardly ever recover completely, with residual lower-limb neurologic sequelae, urinary problems and sexual disfunction.96,102 Here, with regard to clinical outcome, the degree of the initial displacement of the transverse component was found to be closely linked to the neurological recovery rate.104 Another factor found to be associated with neurologic deficits is postoperative reduction with more than 10 mm residual displacement and fragment encroachment into canal and post foramen.113
Regardless of the treatment, neurologic injuries often recover with time, although a complete recovery is seen in less than half of patients. Recovery is better when surgical decompression is associated, even if this is controversial.54 In the case of cauda equina syndrome, surgical decompression improves neurologic recovery.114 Indirect decompression by fracture reduction has shown better results compared to direct laminectomy.115 Also the decompression timing (< 72 h) does not have a clear influence. Although some authors state that it does not seem to influence the outcome, others say that an early decompression would improve the outcome, but it is often not feasible because of the severe condition of the patients during the acute phase.18,115
Discussion/conclusions
Sacral fractures are complex fractures as the sacrum is considered the keystone of the pelvic girdle and thus is subjected to high stresses, being responsible for around 60% of pelvic stability. This highlights the utmost importance of restoring its anatomy and mechanics with the highest possible accuracy after a fracture, making its management extremely challenging.116
The first major issue related to sacral fracture management is the characteristics of the patients who suffer from this condition. They could be young people suffering from a high-energy trauma or elderly patients suffering from low-energy trauma. Both conditions, if not well managed, present high mortality rates. Another issue is related to fracture classification. In order to correctly identify the clinical situation, fracture characteristics and its implications, a surgeon could usually take advantage of fracture classifications. However, given the heterogeneity of sacral fractures, none of the available classifications is comprehensive of all possible aspects related to these fractures, as they are unable to really help the user better understand the fracture. For this purpose, a survey has been conducted among AOSpine/Trauma members to identify the main controversies of sacral fractures. They submitted queries to surgeons about their perceptions of different topics such as severity of different fracture patterns, risk of neurologic injury following disparate fracture location, involvement of S1–L5 facet and insufficiency fractures. Based on the variety of the answers, they concluded the need for a new comprehensive and accepted classification which is able to take into account all the relevant factors associated with this complex fracture group.8
Furthermore, the diagnosis of sacral fractures is challenging, with high rates of mis- or delayed diagnosis.30 The origin of this problem is multifactorial: first of all the low incidence of sacral fractures results in the majority of surgeons having little experience when dealing with them; the variability of clinical presentation, which differs according to the energy of fracture and associated lesions and is often arduous because of altered mental status, both in the case of high-energy trauma due to associated life-threatening conditions and in the case of insufficiency fractures due to the general impairment of the fragile patient; the variety of available imaging techniques which do not have the same diagnostic power, notably in relation to X-rays which often, being the first-line exam, are not powerful enough to detect the fracture, also because of intercurrent difficulties such as air in the bowel, non-compliance of the patient, sclerotic degeneration or arthritis of pelvic bones overlapping the sacrum. A solution to this issue could be to use more X-ray views (inlet, outlet) and to set the mandatory indication to always deepen the diagnostic process with at least a CT scan in case of X-rays showing indirect signs of sacral fractures or high clinical suspicion after a careful evaluation.7,96
Management of sacral fractures is also troublesome, since common accepted standards able to drive the treatment strategy are missing and the few that do exist, such as the stability of the fracture, are not easy to interpret. In order to address this issue, and to help the surgeon facing a sacral fracture give an indication whether to operate or not, the lumbosacral injury classification system (LSICS) has recently been proposed. It is a scoring system, which, similar to what has been done for the cervical and thoraco-lumbar spine, guides surgical management, recommending surgical treatment for each fracture with a score higher than 4, on the basis of morphology, ligament integrity and neurologic status.55
Surgical treatment represents another big challenge for surgeons facing sacral fractures, because it is related to high complication rates and poor outcomes, either related to percutaneous or closed techniques, both being characterized by benefits and drawbacks. Percutaneous and minimally invasive techniques present perioperative complications but fewer postoperative complications compared to open techniques. Furthermore, it is generally difficult to obtain a good reduction with these techniques.93 Open techniques are burdened by some perioperative complications such as a higher quantity of blood loss and longer surgical time, but their principal limitations are related to higher correlation with postoperative complications. However, they allow a more easily achievable and more accurate reduction. Therefore, to reduce complications and improve outcomes, except for cases of high vertical instability or spinopelvic dissociation in which open lumbopelvic fixation implants ensure better stability, the use of percutaneous or minimally invasive techniques should always be attempted. However, to do so, their drawbacks, such as perioperative complications and difficulty to obtain reduction, must be addressed.
Perioperative complications of percutaneous techniques such as malpositioning, consequent neural lesions and radiation exposure are typically related to the iliosacral screw technique. Accurate preoperative planning and the aid given by modern instrumentation to control positioning could reduce malpositioning rate, radiation exposure and surgical time.73,83,92,117,118
To improve fracture reduction, different solutions could be adopted: special positioning of the patient i.e. ‘hyperextended’ supine position in case of transverse fractures; manipulation techniques, especially useful in cases of sacral fractures associated with pelvic ring injuries, such as manipulating the iliac wings together with controlling rotations of the lower limbs when facing a type B pelvic injury; the use of specific aids such as transcondylar traction, indicated in case of impacted transverse fracture, Schanz pin, useful as a percutaneous aid to perform reduction manouvres and to mantain the obtained reduction until the definitive fixation, or frames such as the ‘Starr frame’, able to apply controlled forces to reduce the fracture on different planes simultaneously.75,119–121
Finally, minimally invasive lumbopelvic fixation has also recently been proposed, with promising results,60,76,122,123 thus, it could minimize the high rate of complications related to such an invasive technique.
In conclusion, sacral fractures represent unique injuries with a variety of fracture patterns. They can be associated with shock, intrapelvic solid organ injuries and neurological sequalae. Their treatment possesses many challenges and requires input from a multidisciplinary team for an optimum outcome.
Footnotes
ICMJE Conflict of interest statement: PVG reports a research grant to study the effect of platelet reach plasma (PRP) and mesenchymal stem cells (MSCs) on fracture healing of tibial fractures from Zimmer Biomet; consulting fees or honorariam from Depuy Synthes, Smith & Nephew and ZimmerBiomet. He is President of European Society of Tissue Regeneration in Orthopaedics and Traumatology (ESTROT), outside the submitted work.
The other authors declare no conflict of interest relevant to this work.
Funding statement
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
references
- 1. van Berkel D, Ong T, Drummond A, et al. ASSERT (Acute Sacral inSufficiEncy fractuRe augmenTation) randomised controlled, feasibility in older people trial: a study protocol. BMJ Open 2019;9:e032111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bydon M, De la, Garza-Ramos R, Macki M, Desai A, Gokaslan AK, Bydon A. Incidence of sacral fractures and in-hospital postoperative complications in the United States: an analysis of 2002–2011 data. Spine (Phila Pa 1976) 2014;39:E1103–E1109. [DOI] [PubMed] [Google Scholar]
- 3. Lyders EM, Whitlow CT, Baker MD, Morris PP. Imaging and treatment of sacral insufficiency fractures. AJNR Am J Neuroradiol 2010;31:201–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tamaki Y, Nagamachi A, Inoue K, et al. Incidence and clinical features of sacral insufficiency fracture in the emergency department. Am J Emerg Med 2017;35:1314–1316. [DOI] [PubMed] [Google Scholar]
- 5. Rommens PM, Arand C, Hofmann A, Wagner D. When and how to operate fragility fractures of the pelvis? Indian J Orthop 2019;53:128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bydon M, Fredrickson V, De la, Garza-Ramos R, et al. Sacral fractures. Neurosurg Focus 2014;37:E12. [DOI] [PubMed] [Google Scholar]
- 7. Beckmann NM, Chinapuvvula NR. Sacral fractures: classification and management. Emerg Radiol 2017;24:605–617. [DOI] [PubMed] [Google Scholar]
- 8. Schroeder GD, Kurd MF, Kepler CK, et al. The development of a universally accepted sacral fracture classification: a survey of AOSpine and AOTrauma members. Global Spine J 2016;6:686–694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sakaguchi M, Maebayashi T, Aizawa T, Ishibashi N. Risk factors for sacral insufficiency fractures in cervical cancer after whole pelvic radiation therapy. Anticancer Res 2019;39:361–367. [DOI] [PubMed] [Google Scholar]
- 10. Vajapey S, Matic G, Hartz C, Miller TL. Sacral stress fractures: a rare but curable cause of back pain in athletes. Sports Health 2019;11:446–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Beckmann N, Cai C. CT characteristics of traumatic sacral fractures in association with pelvic ring injuries: correlation using the Young-Burgess classification system. Emerg Radiol 2017;24:255–262. [DOI] [PubMed] [Google Scholar]
- 12. Park YS, Baek SW, Kim HS, Park KC. Management of sacral fractures associated with spinal or pelvic ring injury. J Trauma Acute Care Surg 2012;73:239–242. [DOI] [PubMed] [Google Scholar]
- 13. Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma 2018;32:S1–S170. [DOI] [PubMed] [Google Scholar]
- 14. Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma 1990;30:848–856. [PubMed] [Google Scholar]
- 15. Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury 2013;44:1733–1744. [DOI] [PubMed] [Google Scholar]
- 16. Katsuura Y, Lorenz E, Gardner W., II Anatomic parameters of the sacral lamina for osteosynthesis in transverse sacral fractures. Surg Radiol Anat 2018;40:521–528. [DOI] [PubMed] [Google Scholar]
- 17. Backer HC, Wu CH, Vosseller JT, et al. Spinopelvic dissociation in patients suffering injuries from airborne sports. Eur Spine J 2019. DOI: 10.1007/s00586-019-05983-6 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 18. Tian W, Chen WH, Jia J. Traumatic spino-pelvic dissociation with bilateral triangular fixation. Orthop Surg 2018;10:205–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lehmann W, Hoffmann M, Briem D, et al. Management of traumatic spinopelvic dissociations: review of the literature. Eur J Trauma Emerg Surg 2012;38:517–524. [DOI] [PubMed] [Google Scholar]
- 20. Nonne D, Capone A, Sanna F, et al. Suicidal jumper’s fracture – sacral fractures and spinopelvic instability: a case series. J Med Case Rep 2018;12:186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pulley BR, Cotman SB, Fowler TT. Surgical fixation of geriatric sacral U-type insufficiency fractures: a retrospective analysis. J Orthop Trauma 2018;32:617–622. [DOI] [PubMed] [Google Scholar]
- 22. Bakker G, Hattingen J, Stuetzer H, Isenberg J. Sacral insufficiency fractures: how to classify? J Korean Neurosurg Soc 2018;61:258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res 1988;227:67–81. [PubMed] [Google Scholar]
- 24. Wagner D, Kamer L, Sawaguchi T, Richards RG, Noser H, Rommens PM. Sacral bone mass distribution assessed by averaged three-dimensional CT models: implications for pathogenesis and treatment of fragility fractures of the sacrum. J Bone Joint Surg Am 2016;98:584–590. [DOI] [PubMed] [Google Scholar]
- 25. Ruatti S, Guillot S, Brun J, et al. Which pelvic ring fractures are potentially lethal? Injury 2015;46:1059–1063. [DOI] [PubMed] [Google Scholar]
- 26. Strange-Vognsen HH, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma 1991;5:200–203. [DOI] [PubMed] [Google Scholar]
- 27. Bishop JA, Dangelmajer S, Corcoran-Schwartz I, Gardner MJ, Routt MLC, Jr, Castillo TN. Bilateral sacral ala fractures are strongly associated with lumbopelvic instability. J Orthop Trauma 2017;31:636–639. [DOI] [PubMed] [Google Scholar]
- 28. Isler B. Lumbosacral lesions associated with pelvic ring injuries. J Orthop Trauma 1990;4:1–6. [DOI] [PubMed] [Google Scholar]
- 29. Guerado E, Cervan AM, Cano JR, Giannoudis PV. Spinopelvic injuries: facts and controversies. Injury 2018;49:449–456. [DOI] [PubMed] [Google Scholar]
- 30. Hanna TN, Sadiq M, Ditkofsky N, et al. Sacrum and coccyx radiographs have limited clinical impact in the emergency department. AJR Am J Roentgenol 2016;206:681–686. [DOI] [PubMed] [Google Scholar]
- 31. Rodrigues-Pinto R, Kurd MF, Schroeder GD, et al. Sacral fractures and associated injuries. Global Spine J 2017;7:609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kao FC, Hsu YC, Liu PH, Yeh LR, Wang JT, Tu YK. Osteoporotic sacral insufficiency fracture: an easily neglected disease in elderly patients. Medicine (Baltimore) 2017;96:e9100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sudhir G, K L K, Acharya S, Chahal R. Sacral insufficiency fractures mimicking lumbar spine pathology. Asian Spine J 2016;10:558–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wagner D, Ossendorf C, Gruszka D, Hofmann A, Rommens PM. Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg 2015;41:349–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pascarella R, Del Torto M, Politano R, Commessatti M, Fantasia R, Maresca A. Critical review of pelvic fractures associated with external iliac artery lesion: a series of six cases. Injury 2014;45:374–378. [DOI] [PubMed] [Google Scholar]
- 36. Halawi MJ. Pelvic ring injuries: surgical management and long-term outcomes. J Clin Orthop Trauma 2016;7:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hatgis J, Granville M, Jacobson RE, Berti A. Sacral insufficiency fractures: recognition and treatment in patients with concurrent lumbar vertebral compression fractures. Cureus 2017;9:e1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nork SE, Jones CB, Harding SP, Mirza SK, Routt ML., Jr. Percutaneous stabilization of U-shaped sacral fractures using iliosacral screws: technique and early results. J Orthop Trauma 2001;15:238–246. [DOI] [PubMed] [Google Scholar]
- 39. Mandell JC, Weaver MJ, Khurana B. Computed tomography for occult fractures of the proximal femur, pelvis, and sacrum in clinical practice: single institution, dual-site experience. Emerg Radiol 2018;25:265–273. [DOI] [PubMed] [Google Scholar]
- 40. Schicho A, Schmidt SA, Seeber K, Olivier A, Richter PH, Gebhard F. Pelvic X-ray misses out on detecting sacral fractures in the elderly: importance of CT imaging in blunt pelvic trauma. Injury 2016;47:707–710. [DOI] [PubMed] [Google Scholar]
- 41. Henes FO, Nüchtern JV, Groth M, et al. Comparison of diagnostic accuracy of magnetic resonance imaging and multidetector computed tomography in the detection of pelvic fractures. Eur J Radiol 2012;81:2337–2342. [DOI] [PubMed] [Google Scholar]
- 42. Na WC, Lee SH, Jung S, Jang HW, Jo S. Pelvic insufficiency fracture in severe osteoporosis patient. Hip Pelvis 2017;29:120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Baldwin MJ, Tucker LJ. Sacral insufficiency fractures: a case of mistaken identity. Int Med Case Rep J 2014;7:93–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kinoshita H, Miyakoshi N, Kobayashi T, Abe T, Kikuchi K, Shimada Y. Comparison of patients with diagnosed and suspected sacral insufficiency fractures. J Orthop Sci 2019;24:702–707. [DOI] [PubMed] [Google Scholar]
- 45. Yoder K, Bartsokas J, Averell K, McBride E, Long C, Cook C. Risk factors associated with sacral stress fractures: a systematic review. J Man Manip Ther 2015;23:84–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wang B, Fintelmann FJ, Kamath RS, Kattapuram SV, Rosenthal DI. Limited magnetic resonance imaging of the lumbar spine has high sensitivity for detection of acute fractures, infection, and malignancy. Skeletal Radiol 2016;45:1687–1693. [DOI] [PubMed] [Google Scholar]
- 47. Lapina O, Tiškevičius S. Sacral insufficiency fracture after pelvic radiotherapy: a diagnostic challenge for a radiologist. Medicina (Kaunas) 2014;50:249–254. [DOI] [PubMed] [Google Scholar]
- 48. Scheyerer MJ, Hüllner M, Pietsch C, Werner CM, Veit-Haibach P. Evaluation of pelvic ring injuries using SPECT/CT. Skeletal Radiol 2015;44:217–222. [DOI] [PubMed] [Google Scholar]
- 49. Zhang L, He Q, Jiang M, Zhang B, Zhong X, Zhang R. Diagnosis of insufficiency fracture after radiotherapy in patients with cervical cancer: contribution of technetium tc 99m-labeled methylene diphosphonate single-photon emission computed tomography/computed tomography. Int J Gynecol Cancer 2018;28:1369–1376. [DOI] [PubMed] [Google Scholar]
- 50. Hak DJ, Baran S, Stahel P. Sacral fractures: current strategies in diagnosis and management. Orthopedics 2009;32:orthosupersite.com/view.asp?rID=44034. [DOI] [PubMed] [Google Scholar]
- 51. Gray R, Molnar R, Suthersan M. A minimally invasive surgical technique for the management of U-shape sacral fractures. Spinal Cord Ser Cases 2017;3:17045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hagen J, Castillo R, Dubina A, Gaski G, Manson TT, O’Toole RV. Does surgical stabilization of lateral compression-type pelvic ring fractures decrease patients’ pain, reduce narcotic use, and improve mobilization? Clin Orthop Relat Res 2016;474:1422–1429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Höch A, Schneider I, Todd J, Josten C, Böhme J. Lateral compression type B 2-1 pelvic ring fractures in young patients do not require surgery. Eur J Trauma Emerg Surg 2018;44:171–177. [DOI] [PubMed] [Google Scholar]
- 54. Mahajan R, Tandon V, Das K, Nanda A, Venkatesh R, Chhabra HS. Management of neglected sacral fracture with cauda equina syndrome: report of two cases with review of literature. Spinal Cord Ser Cases 2015;1:15020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lehman RA, Jr, Kang DG, Bellabarba C. A new classification for complex lumbosacral injuries. Spine J 2012;12:612–628. [DOI] [PubMed] [Google Scholar]
- 56. Sommer C. Fixation of transverse fractures of the sternum and sacrum with the locking compression plate system: two case reports. J Orthop Trauma 2005;19:487–490. [DOI] [PubMed] [Google Scholar]
- 57. Kasukawa Y, Miyakoshi N, Ebina T, et al. Enhanced bone healing and decreased pain in sacral insufficiency fractures after teriparatide treatment: retrospective clinical-based observational study. Clin Cases Miner Bone Metab 2017;14:140–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Baillieul S, Guinot M, Dubois C, Prunier A, Mahler F, Gaudin P. Set the pace of bone healing: treatment of a bilateral sacral stress fracture using teriparatide in a long-distance runner. Joint Bone Spine 2017;84:499–500. [DOI] [PubMed] [Google Scholar]
- 59. Bederman SS, Hassan JM, Shah KN, Kiester PD, Bhatia NN, Zamorano DP. Fixation techniques for complex traumatic transverse sacral fractures: a systematic review. Spine (Phila Pa 1976) 2013;38:E1028–E1040. [DOI] [PubMed] [Google Scholar]
- 60. Kanezaki S, Miyazaki M, Notani N, et al. Minimally invasive triangular osteosynthesis for highly unstable sacral fractures: technical notes and preliminary clinical outcomes. Medicine (Baltimore) 2019;98:e16004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Vigdorchik JM, Jin X, Sethi A, et al. A biomechanical study of standard posterior pelvic ring fixation versus a posterior pedicle screw construct. Injury 2015;46:1491–1496. [DOI] [PubMed] [Google Scholar]
- 62. Takao M, Hamada H, Sakai T, Sugano N. Factors influencing the accuracy of iliosacral screw insertion using 3D fluoroscopic navigation. Arch Orthop Trauma Surg 2019;139:189–195. [DOI] [PubMed] [Google Scholar]
- 63. El Dafrawy MH Strike SA Osgood GM. Use of the S3 corridor for iliosacral fixation in a dysmorphic sacrum: a case report. JBJS Case Connect 2017;7:e62. [DOI] [PubMed] [Google Scholar]
- 64. Höch A, Pieroh P, Henkelmann R, Josten C, Böhme J. In-screw polymethylmethacrylate-augmented sacroiliac screw for the treatment of fragility fractures of the pelvis: a prospective, observational study with 1-year follow-up. BMC Surg 2017;17:132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. König MA, Hediger S, Schmitt JW, Jentzsch T, Sprengel K, Werner CML. In-screw cement augmentation for iliosacral screw fixation in posterior ring pathologies with insufficient bone stock. Eur J Trauma Emerg Surg 2018;44:203–210. [DOI] [PubMed] [Google Scholar]
- 66. Kortman K, Ortiz O, Miller T, et al. Multicenter study to assess the efficacy and safety of sacroplasty in patients with osteoporotic sacral insufficiency fractures or pathologic sacral lesions. J Neurointerv Surg 2013;5:461–466. [DOI] [PubMed] [Google Scholar]
- 67. Lucas JF, Routt ML, Jr, Eastman JG. A useful preoperative planning technique for transiliac-transsacral screws. J Orthop Trauma 2017;31:e25–e31. [DOI] [PubMed] [Google Scholar]
- 68. Kobbe P, Hockertz I, Sellei RM, Reilmann H, Hockertz T. Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. Int Orthop 2012;36:159–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Liuzza F, Silluzio N, Florio M, et al. Comparison between posterior sacral plate stabilization versus minimally invasive transiliac-transsacral lag-screw fixation in fractures of sacrum: a single-centre experience. Int Orthop 2019;43:177–185. [DOI] [PubMed] [Google Scholar]
- 70. Dienstknecht T, Berner A, Lenich A, Nerlich M, Fuechtmeier B. A minimally invasive stabilizing system for dorsal pelvic ring injuries. Clin Orthop Relat Res 2011;469:3209–3217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Salášek M, Jansová M, Křen J, Pavelka T, Weisová D. Biomechanical comparison of a transiliac internal fixator and two iliosacral screws in transforaminal sacral fractures: a finite element analysis. Acta Bioeng Biomech 2015;17:39–49. [PubMed] [Google Scholar]
- 72. Futamura K, Baba T, Mogami A, et al. ‘Within ring’-based sacroiliac rod fixation may overcome the weakness of spinopelvic fixation for unstable pelvic ring injuries: technical notes and clinical outcomes. Int Orthop 2018;42:1405–1411. [DOI] [PubMed] [Google Scholar]
- 73. Zhang R, Yin Y, Li S, Guo J, Hou Z, Zhang Y. Sacroiliac screw versus a minimally invasive adjustable plate for Zone II sacral fractures: a retrospective study. Injury 2019;50:690–696. [DOI] [PubMed] [Google Scholar]
- 74. Acklin YP, Marco G, Sommer C. Double locking plate fixation of sacral fractures in unstable pelvic ring C-type injuries. Oper Orthop Traumatol 2015;27:74–79. [DOI] [PubMed] [Google Scholar]
- 75. Pascal-Moussellard H, Hirsch C, Bonaccorsi R. Osteosynthesis in sacral fracture and lumbosacral dislocation. Orthop Traumatol Surg Res 2016;102:S45–S57. [DOI] [PubMed] [Google Scholar]
- 76. Williams SK, Quinnan SM. Percutaneous lumbopelvic fixation for reduction and stabilization of sacral fractures with spinopelvic dissociation patterns. J Orthop Trauma 2016;30:e318–e324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Bourghli A, Boissiere L, Obeid I. Dual iliac screws in spinopelvic fixation: a systematic review. Eur Spine J 2019;28:2053–2059. [DOI] [PubMed] [Google Scholar]
- 78. Mohd Asihin MA, Bajuri MY, Ahmad AR, Ganaisan PK, Fazir M, Salim AA. Spinopelvic fixation supplemented with gullwing plate for multiplanar sacral fracture with spinopelvic dissociation: a case series with short term follow up. Front Surg 2019;6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Sagi HC, Militano U, Caron T, Lindvall E. A comprehensive analysis with minimum 1-year follow-up of vertically unstable transforaminal sacral fractures treated with triangular osteosynthesis. J Orthop Trauma 2009;23:313–319. [DOI] [PubMed] [Google Scholar]
- 80. Song W, Zhou D, He Y. The biomechanical advantages of bilateral lumbo-iliac fixation in unilateral comminuted sacral fractures without sacroiliac screw safe channel: a finite element analysis. Medicine (Baltimore) 2016;95:e5026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Acklin YP, Zderic I, Richards RG, Schmitz P, Gueorguiev B, Grechenig S. Biomechanical investigation of four different fixation techniques in sacrum Denis type II fracture with low bone mineral density. J Orthop Res 2018;36:1624–1629. [DOI] [PubMed] [Google Scholar]
- 82. Mitchell PM, Corrigan CM, Patel NA, et al. 13-year experience in external fixation of the pelvis: complications, reduction and removal. Eur J Trauma Emerg Surg 2016;42:91–96. [DOI] [PubMed] [Google Scholar]
- 83. Krappinger D, Lindtner RA, Benedikt S. Preoperative planning and safe intraoperative placement of iliosacral screws under fluoroscopic control. Oper Orthop Traumatol 2019;31:465–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Wang H, Fu YH, Ke C, et al. Minimally invasive stabilisation of posterior pelvic ring instabilities with pedicle screws connected to a transverse rod. Int Orthop 2018;42:681–686. [DOI] [PubMed] [Google Scholar]
- 85. Kim JW, Oh CW, Oh JK, et al. The incidence of and factors affecting iliosacral screw loosening in pelvic ring injury. Arch Orthop Trauma Surg 2016;136:921–927. [DOI] [PubMed] [Google Scholar]
- 86. Koshimune K, Ito Y, Sugimoto Y, et al. Minimally invasive spinopelvic fixation for unstable bilateral sacral fractures. Clin Spine Surg 2016;29:124–127. [DOI] [PubMed] [Google Scholar]
- 87. El Dafrawy MH, Kebaish KM. Percutaneous S2 alar iliac fixation for pelvic insufficiency fracture. Orthopedics 2014;37:e1033–e1035. [DOI] [PubMed] [Google Scholar]
- 88. Hopf JC, Krieglstein CF, Müller LP, Koslowsky TC. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury 2015;46:1631–1636. [DOI] [PubMed] [Google Scholar]
- 89. Maki S, Nakamura K, Yamauchi T, et al. Lumbopelvic fixation for sacral insufficiency fracture presenting with sphincter dysfunction. Case Rep Orthop 2019;2019:9097876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Konig MA, Jehan S, Boszczyk AA, Boszczyk BM. Surgical management of U-shaped sacral fractures: a systematic review of current treatment strategies. Eur Spine J 2012;5:829–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Strobl FF, Haeussler SM, Paprottka PM, et al. Technical and clinical outcome of percutaneous CT fluoroscopy-guided screw placement in unstable injuries of the posterior pelvic ring. Skeletal Radiol 2014;43:1093–1100. [DOI] [PubMed] [Google Scholar]
- 92. Yang F, Yao S, Chen KF, et al. A novel patient-specific three-dimensional-printed external template to guide iliosacral screw insertion: a retrospective study. BMC Musculoskelet Disord 2018;19:397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Zhang R, Yin Y, Li S, Li A, Hou Z, Zhang Y. Lumbopelvic fixation versus novel adjustable plate for sacral fractures: a retrospective comparative study. J Invest Surg 2019. DOI: 10.1080/08941939.2019.1569737 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 94. Kang S, Chung PH, Kim JP, Kim YS, Lee HM, Eum GS. Superior gluteal artery injury during percutaneous iliosacral screw fixation: a case report. Hip Pelvis 2015;27:57–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Yu YH, Lu ML, Tseng IC, et al. Effect of the subcutaneous route for iliac screw insertion in lumbopelvic fixation for vertical unstable sacral fractures on the infection rate: a retrospective case series. Injury 2016;47:2212–2217. [DOI] [PubMed] [Google Scholar]
- 96. Xie YL, Cai L, Ping AS, Lei J, Deng ZM, Hu C, Zhu XB. Lumbopelvic fixation and sacral decompression for u-shaped sacral fractures: surgical management and early outcome. Curr Med Sci 2018;38:684–690. [DOI] [PubMed] [Google Scholar]
- 97. Raza H, Bowe A, Davarinos N, Leonard M. Bowel preparation prior to percutaneous ilio-sacral screw insertion: is it necessary? Eur J Trauma Emerg Surg 2018;44:211–214. [DOI] [PubMed] [Google Scholar]
- 98. Osterhoff G, Noser J, Sprengel K, Simmen HP, Werner CML. Rate of intraoperative problems during sacroiliac screw removal: expect the unexpected. BMC Surg 2019;19:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Chen W, Hou Z, Su Y, Smith WR, Liporace FA, Zhang Y. Treatment of posterior pelvic ring disruptions using a minimally invasive adjustable plate. Injury 2013;44:975–980. [DOI] [PubMed] [Google Scholar]
- 100. Andresen R, Radmer S, Andresen JR, Schober HC. Comparison of the 18-month outcome after the treatment of osteoporotic insufficiency fractures by means of balloon sacroplasty (BSP) and radiofrequency sacroplasty (RFS) in comparison: a prospective randomised study. Eur Spine J 2017;26:3235–3240. [DOI] [PubMed] [Google Scholar]
- 101. Yang SC, Tsai TT, Chen HS, Fang CJ, Kao YH, Tu YK. Comparison of sacroplasty with or without balloon assistance for the treatment of sacral insufficiency fractures. J Orthop Surg (Hong Kong) 2018;26:2309499018782575. [DOI] [PubMed] [Google Scholar]
- 102. Adelved A, Tötterman A, Glott T, Hellund JC, Madsen JE, Røise O. Long-term functional outcome after traumatic lumbosacral dissociation: a retrospective case series of 13 patients. Injury 2016;47:1562–1568. [DOI] [PubMed] [Google Scholar]
- 103. Adelved A, Tötterman A, Glott T, Søberg HL, Madsen JE, Røise O. Patient-reported health minimum 8 years after operatively treated displaced sacral fractures: a prospective cohort study. J Orthop Trauma 2014;28:686–693. [DOI] [PubMed] [Google Scholar]
- 104. Lindahl J, Mäkinen TJ, Koskinen SK, Söderlund T. Factors associated with outcome of spinopelvic dissociation treated with lumbopelvic fixation. Injury 2014;45:1914–1920. [DOI] [PubMed] [Google Scholar]
- 105. Khaled SA, Soliman O, Wahed MA. Functional outcome of unstable pelvic ring injuries after iliosacral screw fixation: single versus two screw fixation. Eur J Trauma Emerg Surg 2015;41:387–392. [DOI] [PubMed] [Google Scholar]
- 106. Noser J, Dietrich M, Tiziani S, Werner CML, Pape HC, Osterhoff G. Mid-term follow-up after surgical treatment of fragility fractures of the pelvis. Injury 2018;49:2032–2035. [DOI] [PubMed] [Google Scholar]
- 107. Loggers SAI, Joosse P, Jan Ponsen K. Outcome of pubic rami fractures with or without concomitant involvement of the posterior ring in elderly patients. Eur J Trauma Emerg Surg. 2019;45:1021-1029. [DOI] [PubMed] [Google Scholar]
- 108. Eckardt H, Egger A, Hasler RM, et al. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: assessment of complications and factors influencing failure. Injury 2017;48:2717–2723. [DOI] [PubMed] [Google Scholar]
- 109. Walker JB, Mitchell SM, Karr SD, Lowe JA, Jones CB. Percutaneous transiliac-transsacral screw fixation of sacral fragility fractures improves pain, ambulation, and rate of disposition to home. J Orthop Trauma 2018;32:452–456. [DOI] [PubMed] [Google Scholar]
- 110. Boyoud-Garnier L, Boudissa M, Ruatti S, Kerschbaumer G, Grobost P, Tonetti J. Chronic low back pain after lumbosacral fracture due to sagittal and frontal vertebral imbalance. Orthop Traumatol Surg Res 2017;103:523–526. [DOI] [PubMed] [Google Scholar]
- 111. Lee HD, Jeon CH, Won SH, Chung NS. Global sagittal imbalance due to change in pelvic incidence after traumatic spinopelvic dissociation. J Orthop Trauma 2017;31:e195–e199. [DOI] [PubMed] [Google Scholar]
- 112. Lee JS, Kim YH. Factors associated with gait outcomes in patients with traumatic lumbosacral plexus injuries. Eur J Trauma Emerg Surg. 2019. doi: 10.1007/s00068-019-01137-x [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 113. Adelved A, Tötterman A, Hellund JC, Glott T, Madsen JE, Røise O. Radiological findings correlate with neurological deficits but not with pain after operatively treated sacral fractures. Acta Orthop 2014;85:408–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Bekmez S, Demirkıran G, Caglar O, Akel I, Acaroğlu E. Transverse sacral fractures and concomitant late-diagnosed cauda equina syndrome. Ulus Travma Acil Cerrahi Derg 2014;20:71–74. [DOI] [PubMed] [Google Scholar]
- 115. Kepler CK, Schroeder GD, Hollern DA, et al. Do formal laminectomy and timing of decompression for patients with sacral fracture and neurologic deficit affect outcome? J Orthop Trauma 2017;31:S75–S80. [DOI] [PubMed] [Google Scholar]
- 116. Bai Z, Gao S, Liu J, Liang A, Yu W. Anatomical evidence for the anterior plate fixation of sacroiliac joint. J Orthop Sci 2018;23:132–136. [DOI] [PubMed] [Google Scholar]
- 117. Theologis AA, Burch S, Pekmezci M. Placement of iliosacral screws using 3D image-guided (O-Arm) technology and stealth navigation: comparison with traditional fluoroscopy. Bone Joint J Br 2016;98-B:696–702. [DOI] [PubMed] [Google Scholar]
- 118. Wang JQ, Wang Y, Feng Y, et al. Percutaneous sacroiliac screw placement: a prospective randomized comparison of robot-assisted navigation procedures with a conventional technique. Chin Med J (Engl) 2017;130:2527–2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Irifune H, Hirayama S, Takahashi N, Chiba M, Yamashita T. Closed reduction in a ‘hyperextended supine position’ with percutaneous transsacral-transiliac and iliosacral screw fixation for Denis zone III sacral fractures. Adv Orthop 2018;2018:6098510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Ruatti S, Kerschbaumer G, Gay E, Milaire M, Merloz P, Tonetti J. Technique for reduction and percutaneous fixation of U- and H-shaped sacral fractures. Orthop Traumatol Surg Res 2013;99:625–629. [DOI] [PubMed] [Google Scholar]
- 121. Peng Y, Zhang W, Zhang G, et al. Using the Starr Frame and Da Vinci surgery system for pelvic fracture and sacral nerve injury. J Orthop Surg Res 2019;14:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Fujino S, Miyagi M, Tajima S, et al. Surgical treatment for suicidal jumper’s fracture (unstable sacral fracture) with thoracolumbar burst fracture: a report of three cases. Spine Surg Relat Res 2017;1:100–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Okuda A, Maegawa N, Matsumori H, et al. Minimally invasive spinopelvic ‘crab-shaped fixation’ for unstable pelvic ring fractures: technical note and 16 case series. J Orthop Surg Res 2019;14:51. [DOI] [PMC free article] [PubMed] [Google Scholar]