Abstract
This cohort study reports a decade of increases and decreases in insulin prices and cost burden for insured patients with diabetes.
In the United States, increasing insulin out-of-pocket costs1 have been a concern, and the potential for rationing2 has prompted states to consider capping these costs.3
Patients with a high-deductible health plan with a health savings account (HDHP-HSA) have high medication costs because these plans require payment of the full reimbursement price until the annual deductible is reached. In contrast, patients with a health reimbursement arrangement (HRA) or a no-account plan (without an HSA) typically have tiered drug copayments. Plan members with an HRA can use their reimbursement account to pay for medical expenses. In this cohort study, we examined insulin out-of-pocket costs and reimbursement price from 2006 to 2017 among patients with commercial health insurance.
Methods
We used Optum’s deidentified Clinformatics Data Mart Database4 to obtain medical and pharmacy claims data for privately insured members from all 50 states. We applied the HEDIS (Healthcare Effectiveness Data and Information Set) claims-based definition for diabetes5 and identified patients with diabetes who had insulin fills. The Harvard Pilgrim Health Care Institutional Review Board approved this study. Informed consent was waived by this institutional review board because the study used deidentified data.
We classified health insurance benefit types as HDHP-HSA, HRA, or no account. We imputed insulin reimbursement price per calendar year by calculating the median non-$0 deductible payment per 30-day equivalent fill of insulin prescriptions among members with an HDHP-HSA. These members pay the reimbursement price negotiated by the pharmacy benefit manager or insurer until they reach their deductible amount; this value approximates the reimbursement price while minimizing outlier price effects.
In addition, we calculated insulin out-of-pocket costs per 30-day fill and per member per month to characterize the actual monthly patient costs. Using an annual time-series design, we estimated the 2006 to 2017 inflation-adjusted (2017 US dollars) median reimbursement prices and mean out-of-pocket costs. We stratified out-of-pocket cost per member per month trends by health insurance benefit type. Because we had only 6 months of 2017 data, we imputed full-year measures on the basis of summarized January-to-June costs to summarized January-to-December costs from 2006 to 2016. The eMethods in the Supplement provides more detail.
All statistical analyses were performed with SAS, version 7.1 (SAS Institute Inc). Data were analyzed from January 1, 2006, to June 30, 2017.
Results
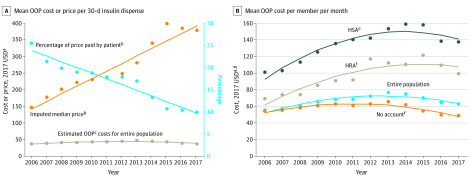
Data from 612 071 unique patients with diabetes and 10 954 436 insulin claims were analyzed. Of these claims, 8 800 930 (80%) originated from members with a no-account plan, 442 662 (4%) from those with an HRA plan, and 774 903 (7%) from those with an HDHP-HSA. In addition, 935 941 (9%) lacked insurance benefit design data and were excluded from the stratified analysis (eFigure in the Supplement). The median insulin 30-day fill reimbursement price increased from $143 (95% CI, $119-$167) in 2006 to $394 (95% CI, $370-$418) in 2017 ($23/y increase; 95% CI, $19-$27). The mean out-of-pocket cost per 30-day insulin fill was $36 (95% CI, $33-$39) in 2006, $45 (95% CI, $43-$46) in 2012, and $38 (95% CI, $36-$41) in 2017. Patients’ share of insulin reimbursement price decreased from 24% (95% CI, 22%-26%) in 2006 to 10% (95% CI, 8.0%-11%) in 2017 (Figure, A and Table).
Figure. Estimated and Observed Annual Out-of-Pocket (OOP) Costs and Price for Insulin Supply .
2017 values were imputed by (1) estimating the ratio of January-to-June values to January-to-December values in 2017 (per outcome) based on the 2006 to 2016 trend in this ratio and (2) multiplying the January-to-June costs from 2017 by the estimated 2017 ratio. Estimates were derived from an autoregressive model with intercept, trend, and change in trend2 terms, adjusting SEs for autocorrelation and removing nonsignificant terms. The eMethods section in the Supplement provides more details.
aCosts and prices were inflation-adjusted to 2017 US dollars according to the Consumer Price Index for US medical care.
bInsulin prices were imputed by calculating the median non-$0 OOP payment toward the annual deductible per 30-day equivalent insulin fill among members with a high-deductible health plan with a health savings account (HDHP-HSA). The percentage paid was the mean annual insulin OOP cost divided by the imputed price of insulin per given year. The eMethods section in the Supplement provides more details.
cOOP costs were derived by using 30-day equivalent insulin fills.
dOOP costs were calculated at the per member per month level.
eHDHP-HSA plans have federally regulated deductible minimums (≥$1050 to $13 100 over this period) and allow tax-exempt HSA contributions, but most services (including medications) are subject to a deductible.
fNo account and health reimbursement arrangement (HRA) are plans with any deductible amount but without any type of HSA.
Table. Estimated Reimbursement Prices of and Out-of-Pocket (OOP) Costs for 30-Day Insulin Dispenses, 2006, 2012, and 2017a.
| Parameter | Estimated value (95% CI) | ||
|---|---|---|---|
| 2006 | 2012 | 2017 | |
| Estimates per 30-d dispense among all insulin users | |||
| Insulin, US$ | |||
| Price | 143 (119-167) | 280 (268-291) | 394 (370-418) |
| OOP costs per 30-d dispense | 36 (33-39) | 45 (43-46) | 38 (36-41) |
| Share of price paid by patient, % | 24 (22-26) | 16 (15-17) | 10 (8-11) |
| OOP estimates per member per mo, US$b | |||
| All insulin users | 52 (48-57) | 72 (70-75) | 64 (60-68) |
| HSA | 93 (82-104) | 146 (140-153) | 141 (130-152) |
| HRA | 62 (48-75) | 105 (98-113) | 108 (94-121) |
| No account | 52 (49-56) | 63 (61-65) | 48 (44-51) |
Abbreviation: HDHP, high-deductible health plan; HRA, health reimbursement arrangement; HSA, health savings account.
All US dollar amounts were adjusted for inflation and standardized to 2017 dollars using the medical expense Consumer Price Index data from 2006 to 2017. Members with a HDHP-HSA must pay the full costs of medications, including insulin, until they reach their deductible. Those with HRA and no-account plans pay for medications according to a copayment schedule. The percentage refers to the amount members paid for insulin divided by the imputed median price of insulin for a given year. Estimates were derived from an autoregressive model with intercept, trend, and change in trend2 terms, adjusting SEs for autocorrelation and removing nonsignificant terms. The 95% CIs were derived from the estimates from the time-series model by substituting parameters for specific points in time (ie, 2006, 2012, and 2017). The eMethods section in the Supplement provides more details.
Insulin OOP costs were calculated at the per member per month level to account for multiple insulin prescription fills in a given month.
Among all insulin users, insulin out-of-pocket costs per member per month increased from $52 (95% CI, $48-$57) in 2006 to a peak of $72 (95% CI, $70-$75) in 2013, and then decreased to $64 (95% CI, $60-$68) in 2017. The out-of-pocket costs per member per month for those with an HDHP-HSA increased from $93 (95% CI, $82-$104) in 2006 to a peak of $150 (95% CI, $144-$155) in 2014, and then decreased to $141 (95% CI, $130-$152) in 2017 (Figure, B and Table).
Discussion
Despite the increasing insulin prices paid by insurers, insulin out-of-pocket costs remained relatively flat from 2006 to 2017 among privately insured patients and began to decrease in 2013. Members with an HDHP-HSA paid substantially higher out-of-pocket amounts per month, which began decreasing in 2014.
This study has some limitations. First, we did not study uninsured or publicly insured patients or those with other private insurance but whose data were not in the Optum database. Second, the imputed insulin price did not account for manufacturer rebates. Third, the claims data used may have had inaccuracies.
Although the findings in this study contradict the view that insulin cost-sharing is excessive for many privately insured patients,2 monthly out-of-pocket payments may be burdensome for low-income individuals. Nevertheless, the data suggest that privately insured patients have been relatively shielded from insulin price increases and that commercial health insurers have accommodated higher insulin prices by increasing premiums or deductibles for all members.6
eMethods.
eFigure. CONSORT Diagram
eReferences
References
- 1.Lipska KJ, Ross JS, Van Houten HK, Beran D, Yudkin JS, Shah ND. Use and out-of-pocket costs of insulin for type 2 diabetes mellitus from 2000 through 2010. JAMA. 2014;311(22):2331-2333. doi: 10.1001/jama.2014.6316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sable-Smith B. Weekend Edition Saturday. Insulin’s high cost leads to lethal rationing. September 1, 2018. Accessed January 23, 2019. https://www.npr.org/sections/health-shots/2018/09/01/641615877/insulins-high-cost-leads-to-lethal-rationing
- 3.Lannan K. Massachusetts Senate unanimously approves bill targeting high drug prices. November 15, 2019. Accessed December 3, 2019. https://www.masslive.com/news/2019/11/massachusetts-senate-unanimously-approves-bill-targeting-high-drug-prices.html
- 4.Optum. De-identified Clinformatics Data Mart Database. Accessed August 1, 2019. https://www.optum.com/solutions/life-sciences.htm
- 5.Ross-Degnan D, Wallace J, Zhang F, Soumerai SB, Garabedian L, Wharam JF. Reduced cost-sharing for preventive drugs preferentially benefits low-income patients with diabetes in high deductible health plans with health savings accounts: a Natural Experiment for Translation in Diabetes (NEXT-D2) study. Published online May 2020. Medical Care. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sherman M, Curfman GD, Parent J, Wagner AK Prescription medications account for one in four dollars spent by a commercial health plan. Health Affairs blog. August 24, 2018. Accessed August 4, 2019. https://www.healthaffairs.org/do/10.1377/hblog20180821.820628/full/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods.
eFigure. CONSORT Diagram
eReferences