Abstract
Objectives
This article aimed to assess associations of childhood socioeconomic conditions (CSC) with the risk of frailty in old age and whether adulthood socioeconomic conditions (ASC) influence this association.
Methods
Data from 21,185 individuals aged 50 years and older included in the longitudinal Survey of Health, Ageing, and Retirement in Europe were used. Frailty was operationalized as a sum of presenting weakness, shrinking, exhaustion, slowness, or low activity. Confounder-adjusted multilevel logistic regression models were used to analyze associations of CSC and ASC with frailty.
Results
While disadvantaged CSC was associated with higher odds of (pre-)frailty in women and men (odds ratio [OR] = 1.73, 95% confidence interval [CI] 1.34, 2.24; OR = 1.84, 95% CI 1.27, 2.66, respectively), this association was mediated by ASC. Personal factors and demographics, such as birth cohort, chronic conditions, and difficulties with activities of daily living, increased the odds of being (pre-)frail.
Discussion
Findings suggest that CSC are associated with frailty at old age. However, when taking into account ASC, this association no longer persists. The results show the importance of improving socioeconomic conditions over the whole life course in order to reduce health inequalities in old age.
Keywords: Health outcomes, Socioeconomic status, Successful aging
Frailty is a clinical syndrome used in geriatric medicine characterized by cumulative declines across multiple biological systems and, as a result, an increased vulnerability to stressors (Clegg, Young, Iliffe, Rikkert, & Rockwood, 2013). Frail people are at an increased risk of disability, falls, dementia, institutionalization, healthcare utilization, and death (Romero-Ortuno, 2013). Although there is an important heterogeneity in measures and definitions of frailty, one operationalization that has been validated, widely used, and accepted is the phenotype of frailty, previously described by Fried et al. (2001) (Etman, Burdorf, Van der Cammen, Mackenbach, & Van Lenthe, 2012; Romero-Ortuno, 2013; Santos-Eggimann, Cuenoud, Spagnoli, & Junod, 2009). It is defined as the presence of at least three of five specific attributes; shrinking, weakness, exhaustion, slowness, and low activity (Fried et al., 2001; Macklai, Spagnoli, Junod, & Santos-Eggimann, 2013). The presence of one or two of the attributes can be considered as pre-frailty, a precursor of frailty. As frailty is a dynamic process, transitions between the states take place and each of the states is predictive of outcomes such as hospitalization or worsening disability. Thus, it is important to take different states into consideration when studying frailty (Gill, Gahbauer, Allore, & Han, 2006).
Previous research has shown that the prevalence of frailty increases with each 5-year older age group: studies found prevalence rates of 17% among community-dwelling older adults aged 65 years and older and 25% to 40% among adults aged 80 years and over (Bandeen-Roche et al., 2015; Fried et al., 2001; Santos-Eggimann et al., 2009). Moreover, it was found that 52% of community-dwelling older adults over the age of 65 years were in a pre-frail state (Santos-Eggimann et al., 2009). Additionally, frailty was found to be more prevalent in women than in men, persons with lower education and lower income, poorer health, higher rates of comorbid chronic disease and disabilities, and in residents of nursing homes (Buckinx et al., 2015; Etman et al., 2012). With an aging population, the number of (pre-)frail people will increase rapidly, thus identifying people at risk and preventing the process of becoming frail is important.
Poor socioeconomic circumstances during childhood have already been shown to be associated with negative health outcomes during adulthood, such as higher risk of cardiovascular disease, lower quality of life, poorer physical capability, and higher mortality rates (Ben-Shlomo, 2013; Kuh, 2004; Wahrendorf & Blane, 2015). Multiple life course and life stage models exist in which childhood is regarded as the period in which people are most vulnerable to external influences (Blane, 2013; Bruer, 2001; Strachan, 2004; Stringhini et al., 2015). Childhood is thought to influence health in later life through different possible pathways including biological and developmental processes, cumulative (dis)advantage of structural stress exposure, and social mobility (Bruer, 2001; Dannefer, 2003; Luo & Waite, 2005).
Besides individual-level behaviors of children growing up in lower childhood socioeconomic circumstances, structural factors can also influence health and may have been prominent in the studied cohort during this period in Europe (Sharpe et al., 2018). For example, growing up in poor socioeconomic circumstances may also mean growing up in a lower-income neighborhood and home with poor environmental conditions, less access to quality education, quality health care and high-quality social networks, which in turn may impact health at older age (Doku, Acacio-Claro, Koivusilta, & Rimpela, 2018; Lazar & Davenport, 2018; Sharpe et al., 2018). Previous studies also suggest that socioeconomic factors contribute to differences in frailty and pre-frailty and that health inequalities as a result of education, occupational class, and wealth persist throughout old age (Santos-Eggimann et al., 2009; Stolz, Mayerl, Waxenegger, Rasky, & Freidl, 2017). Across birth cohorts, wealthier earlier birth cohorts show similar levels of frailty as recent cohorts, but the poorest cohort shows higher levels of frailty compared to earlier cohorts (Marshall, Nazroo, Tampubolon, & Vanhoutte, 2015). Additionally, recent studies found an increased risk in the worsening of frailty over time in lower educated persons aged 55 years and older compared to higher educated persons (Etman, Kamphuis, van der Cammen, Burdorf, & van Lenthe, 2015; Franse et al., 2017; Gill et al., 2006). This persisting inequality in old age can be partly explained by lifestyle and health, such as lower alcohol consumption, higher sedentariness, higher obesity, higher chronic disease rates, and being depressed (Cheval et al., 2018; Etman et al., 2015; Franse et al., 2017; Hoogendijk et al., 2014; Soler-Vila et al., 2016).
So far, available studies have mainly looked at the influence of socioeconomic factors in mid- and late adulthood. However, not many studies exist on the effect of socioeconomic conditions in the sensitive buildup stage in the life course (i.e., childhood) on frailty, using longitudinal data and a comprehensive operationalization of frailty (Strachan, 2004; Vineis, Kelly-Irving, Rappaport, & Stringhini, 2016). In addition, how childhood socioeconomic conditions (CSC) may influence the development of frailty along with the effects of aging and of life-course socioeconomic conditions is not well studied. Using longitudinal and multinational data enabled us to study whether (a) CSC are associated with levels of frailty in older adults as well as its rate of change and (b) whether this association is mediated by adulthood socioeconomic conditions (ASC). As a final, exploratory, aim, we examined this association while including other potentially related variables to frailty, such as chronic conditions and difficulties with activities of daily living (ADL).
Method
Study Design and Population
Data from individuals aged 50 years and over included in the longitudinal Survey of Health, Ageing, and Retirement in Europe (SHARE) were used. SHARE includes six waves of data that were collected every 2 years between 2004 and 2016 (Borsch-Supan et al., 2013). By means of standardized computer-assisted face-to-face interviews, information on aspects ranging from economic variables and demographics to health variables was collected (Alcer et al., 2005). Additionally, measurements of grip strength were performed for all participants. Retrospective life course data on CSC were only collected in Wave 3.
For the current analyses, we used all six currently available waves. SHARE participants were eligible for the analyses if they were aged between 50 and 95 years old, participated in the third wave, and had at least one complete measure of frailty in Waves 1, 2, 4, 5, and 6. Participants were drawn from 14 European countries based on probability samples adapted to each country (Klevmarken, 2005). SHARE was approved by the relevant research ethics committees in the participating countries and all participants provided written informed consent.
Frailty
The operationalization of frailty required adaptation of the SHARE data to the original attributes from the phenotype of frailty by Fried and colleagues (Fried et al., 2001). In order to construct the dependent variable with the provided information in SHARE, we adhered to Santos-Eggimann et al.’s (2009) proposition of the operationalization of frailty, which was measured similarly at each wave. This operationalization was constructed by selecting the most suitable metric and has been tested and validated in the SHARE population (Macklai et al., 2013; Romero-Ortuno, 2013). The shrinking attribute was operationalized using the question, “What has your appetite been like” and was fulfilled when participants reported the answer “diminution in desire for food” or, in the case of an unclear response to this question, the answer “less” to the follow-up item “So have you been eating more or less than usual?”. Weakness was derived from the grip strength measures, where the highest out of four consecutive dynamometer measures (two from each hand) was analyzed using cutoffs calculated for each wave separately, stratified by gender and body mass index quartiles as proposed by Fried et al. (Fried et al., 2001). The weakness criterion was fulfilled by the weakest 20% in each category. Exhaustion was operationalized by a positive answer to the question, “In the last month, have you had too little energy to do things you wanted to do?”. The slowness attribute was defined through mobility questions, as SHARE measured walking speed only for individuals aged 75 or older. According to Santos-Eggimann et al. (2009), previous analyses showed that low speed and positive answers to either of the following two items were strongly associated: “Because of a health problem, do you have any difficulty [expected to last three or more months] walking 100 meters” or “…climbing one flight of stairs without resting”. For the low activity attribute, the question “How often do you engage in activities that require a low or moderate level of energy such as gardening, cleaning the car, or going for a walk?” was considered. The criterion was fulfilled for individuals answering either “one to three times a month” or “hardly ever or never.”
Based on the operationalization of the five attributes, we created a score ranging from zero to five. Individuals with zero points were classified as non-frail, with one or two points as pre-frail, and with three or more points as frail (Fried et al., 2001). In the main analyses, frailty was dichotomized as either non-frail or (pre-)frail, in which those in pre-frail and frail states were combined.
CSC and ASC
CSC was computed according to Wahrendorf and Blane’s (2015) measure of childhood circumstances. This measure was constructed by combining four binary indicators of socioeconomic conditions at age 10; the occupational position of the main breadwinner, number of books at home, overcrowding, and housing quality. Previous studies showed that those four indicators are relevant when assessing the long-term effects of CSC on health (Chittleborough, Baum, Taylor, & Hiller, 2006; Dedman, Gunnell, Davey Smith, & Frankel, 2001; Evans, Kelley, Sikora, & Treiman, 2010; Marsh, 1999). This information was collected in the third wave of SHARE as part of the SHARELIFE module, which is a retrospective survey focused on people’s life histories (Schröder, 2011).
The occupational position of the main breadwinner was constructed by reclassifying the 10 main occupational groups of the International Standard Classification of Occupations (ISCO) according to their skill levels (Wahrendorf, Blane, Bartley, Dragano, & Siegrist, 2013). The first and second skill levels were categorized as “low” and the third and fourth skill levels were regrouped as “high” occupational position. A binary item was constructed using the number of books at home, with the category “0–10 books” being an indicator of social disadvantage (Evans et al., 2010). The measure of overcrowding was constructed using survey answers regarding the number of people living in the household and the number of rooms (excluding kitchen, bathrooms, and hallways). Having more than one person per room in the household was considered as overcrowding (Marsh, 1999). Finally, housing quality was assessed by the presence of the following items; fixed bath, cold running water supply, hot running water supply, indoor toilet, and central heating. Where none of these were present, the household was coded as disadvantaged (Dedman et al., 2001). A categorical variable for CSC ranging from zero (most advantaged) to four (most disadvantaged) was computed by combining the information of the four indicators.
The following variables were used as indicators of ASC; highest educational attainment (number of years), occupational class (high skill and low skill), and satisfaction with household income (from the question “Is household able to make ends meet?”, from one “with great difficulty” to four “easily”). Occupational class—high- or low-skilled—was based on the ISCO of the main job using the question “Which of the jobs you have told me about was the final job of your main career or occupation? By this we mean the last job in the career or the occupation that took up most of your working life, even though you might have had other jobs afterwards.” Participants who never performed paid work were classified as low skill.
Potential Confounders and Predictors
All analyses were adjusted for age and attrition (no dropout, dropped, deceased) and potential confounders, including birth cohort (no crisis or war period [i.e., born before 1914, between 1919 and 1928, or after 1945], first and second world war [i.e., born between 1914 and 1918 or between 1939 and 1945], and Great Depression [i.e., born between 1929 and 1938]), and growing up with biological parents (both parents, either mother or father, without parents). Final models (Model 3) were adjusted for other possible predictors of frailty; partnership status (living with partner: yes, no), cognitive functioning (delayed recall memory and verbal fluency), smoking (ever, not), number of chronic conditions (total number), difficulties with ADL (score range zero to five), and difficulties with instrumental activities of daily living (IADL, score range 0 to 5). For the number of chronic conditions, a score was computed based on the following conditions: stroke, heart attack, hypertension, diabetes, cancer, Parkinson’s disease, and asthma. ADL was based on bathing, dressing, eating, getting in and out of bed, and walking across a room. IADL was based on using the telephone, managing money, managing medications, shopping for groceries, and preparing meals.
Statistical Analyses
To describe the associations of CSC with frailty, logistic mixed-effects models were estimated. These models have been developed to take the nested structure of the data into account (e.g., multiple observations within a single participant), thereby providing accurate parameter estimates with acceptable Type 1 error rates (Boisgontier & Cheval, 2016). Additionally, using this modeling approach, we did not have to exclude participants that had missing observations in certain waves, as they do not require an equal number of observations from all participants (see Supplementary Figure 1 for a flow chart for more information on participants’ selection criteria). We also checked if missing observations were country-specific, which was not the case. Models’ Bayesian Information Criterion (BIC), as well as likelihood ratio tests, revealed that the best random structure was random intercepts for participants and random linear slopes of age. Random slopes estimate the linear growth trajectory of the individual participant. In order to see the estimates per country, countries were included as fixed effect (Supplementary Tables 3–6).
Analyses were stratified by gender based on expected differences between men and women in the prevalence of frailty (Buckinx et al., 2015). All analyses were adjusted for age, country, and living with biological parents during childhood. All models were additionally adjusted for birth cohort, as people from earlier cohorts were more likely to come from more disadvantaged socioeconomic conditions. Age was centered at 73 years, which was the sample’s midpoint, and then divided by ten so the coefficients yield the effect of the overall frailty evolution over a 10-year interval. Age squared was included to account for possible accelerated changes in frailty over aging. Interaction terms between CSC and age were included to test whether CSC moderated the effects of aging on (pre-)frailty. A significant interaction means that the rate of change in frailty differs across CSC. As potential mediators, we ran a second model that included indicators of ASC. A third model additionally included health- and lifestyle variables.
Four sensitivity analyses were performed; two analyses with frailty as a dichotomous outcome comparing (a) non-frail to pre-frail individuals, and (b) non-frail and pre-frail versus frail individuals (to check for the associations in different frailty states, as the number of participants who were frail within each CSC were low), one where participants older than 90 were excluded (as descriptive statistics showed that observations in this age category within each CSC were very low, which may lead to problems with estimation), and one where clinically depressed participants were excluded (as the definition of frailty overlaps to some extent with depression, particularly exhaustion and low activity). Additionally, we ran ordinal multilevel regression models, where frailty was divided into three categories; frail, pre-frail, and non-frail. Statistical analyses were performed using the R language and the lme4 and lmerTest packages (Bates, Mächler, Bolker, & Walker, 2015; Kuznetsova, 2016; R Core Team, 2017).
Results
Participant Characteristics
Participant characteristics are reported in Table 1. The final sample consisted of 21,185 people (55% female) (see Supplementary Figure 1 for a flow chart). Mean age was 63.4 years (9.5 SD) for women and 63.4 (9.0) for men. A CSC gradient was observed in women and men: the percentage of (pre-)frail people increased from most advantaged to most disadvantaged CSC (Supplementary Tables 1 and 2). Participants had on average 3 complete (information on all attributes was available) measures of frailty over the five waves and the number of participants with only one measurement wave was 13%.
Table 1.
Participant Characteristics
| Women | Men | |
|---|---|---|
| n (%) | n (%) | |
| Non-frail | 5,168 (45%) | 5,289 (55%) |
| Pre-frail | 5,169 (45%) | 3,723 (39%) |
| Frail | 1,267 (11%) | 569 (6%) |
| Age, years (SD) | 63.4 (9.5) | 63.4 (9.0) |
| Birth cohort | ||
| No war, no economic crisis | 5,996 (52%) | 4,680 (49%) |
| War | 2,886 (25%) | 2,461 (26%) |
| Economic crisis | 2,722 (23%) | 2,440 (25%) |
| Living with biological parents | ||
| Both parents | 10,459 (90%) | 8,681 (91%) |
| One biological parent | 902 (8%) | 729 (8%) |
| Without biological parent | 243 (2%) | 171 (2%) |
| Attrition | ||
| No drop out | 8,402 (72%) | 6,609 (69%) |
| Drop out | 2,299 (20%) | 1,926 (20%) |
| Death | 903 (9%) | 1,046 (11%) |
| Level of education, in years (SD) | 10.3 (4.1) | 11.2 (4.4) |
| Main occupation low skill (vs high) | 9,681 (83%) | 6,566 (69%) |
| Satisfaction with income (SD) | 2.8 (0.9) | 2.9 (0.9) |
| Delayed recall memory (SD) | 0.4 (1.8) | 0.4 (1.9) |
| Verbal fluency (SD) | 2.1 (6.6) | 2.1 (6.8) |
| Ever smoked (SD) | 0.3 (0.5) | 0.6 (0.5) |
| Number chronic conditions (SD) | 1.7 (1.3) | 1.5 (1.2) |
| Partnership status, living with partner (vs without) | 7,760 (67%) | 8,001 (84%) |
| Difficulties ADL (SD) | −0.0 (0.6) | −0.0 (0.5) |
| Difficulties IADL (SD) | −0.0 (0.8) | −0.1 (0.7) |
Note. ADL = activities of daily living; IADL = instrumental activities of daily living; SD = standard deviation. N women = 11,604, N men = 9,581. Satisfaction with income ranges between 1 (great difficulty) and 4 (easily).
Effects of CSC on Risk of Frailty Over Aging
The results of the confounder-adjusted logistic mixed-effects models for the association of CSC with the odds of being (pre-)frail are shown in models 1 in Table 2 (women) and Table 3 (men). Women who grew up in disadvantaged and most disadvantaged CSC had higher odds of being (pre-)frail compared to those in the most advantaged CSC. This result was similar among men, where additionally a higher odds was found among those from middle CSC. Among women and men, a positive age indicated that as people age, the odds of being (pre-)frail increased. The significant quadratic effect of age coefficient indicated that there was an accelerated change of frailty over aging. Interactions of CSC with age and age squared showed no significant effects, indicating that CSC did not moderate the level nor the rate of change in (pre-)frailty over aging (Supplementary Tables 3 and 4).
Table 2.
Associations Between Childhood Socioeconomic Conditions and (Pre-)Frailtya at Older Age, Women
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 3.52 (2.72, 4.55)*** | 3.49 (2.35, 5.19)*** | 3.69 (2.07, 6.60)*** |
| Age squared | 1.45 (1.25, 1.68)*** | 1.34 (1.05, 1.69)* | 1.57 (1.10, 2.23)* |
| Birth cohort, warb | 0.97 (0.87, 1.08) | 0.95 (0.85, 1.05) | 0.99 (0.87, 1.10) |
| Birth cohort, economic crisisb | 1.02 (0.91, 1.17) | 0.99 (0.87, 1.11) | 0.93 (0.79, 1.10) |
| Living with one parentc | 1.09 (0.87, 1.08) | 1.01 (0.88, 1.18) | 1.02 (0.85, 1.23) |
| Living without parentsc | 1.23 (0.94, 1.63) | 1.18 (0.90, 1.56) | 1.17 (0.84, 1.63) |
| CSC advantagedd | 1.04 (0.81, 1.34) | 0.92 (0.74, 1.18) | 0.98 (0.72, 1.34) |
| CSC middled | 1.17 (0.93, 1.63) | 0.94 (0.74, 1.20) | 1.09 (0.80, 1.48) |
| CSC disadvantagedd | 1.33 (1.04, 1.70)* | 0.96 (0.74, 1.23) | 0.92 (0.67, 1.26) |
| CSC most disadvantagedd | 1.73 (1.34, 2.24)*** | 1.12 (0.85, 1.47) | 1.06 (0.75, 1.50) |
| Age × CSC advantagedd | 0.90 (0.67, 1.21) | 0.91 (0.68, 1.22) | 1.02 (0.66, 1.58) |
| Age × CSC middled | 1.04 (0.78, 1.38) | 1.08 (0.81, 1.44) | 1.05 (0.68, 1.60) |
| Age × CSC disadvantagedd | 1.02 (0.77, 1.35) | 1.02 (0.76, 1.38) | 0.98 (0.63, 1.51) |
| Age × CSC most disadvantagedd | 0.87 (0.65, 1.16) | 0.89 (0.65, 1.21) | 1.01 (0.64, 1.60) |
| Level of education in years | 0.96 (0.95, 0.98)*** | 0.97 (0.95, 0.99)* | |
| Age × education | 1.00 (0.98, 1.02) | 1.00 (0.97, 1.03) | |
| Main occupation, lowe | 1.20 (1.02, 1.40)* | 1.13 (0.92, 1.39) | |
| Age × low occupatione | 0.98 (0.81, 1.18) | 0.75 (0.56, 1.00) | |
| Satisfaction with income | 1.37 (1.30, 1.44)*** | 1.30 (1.22, 1.39)*** | |
| Age × satisfaction with income | 1.05 (0.99, 1.12) | 1.01 (0.92, 1.10) | |
| Partnership, without partnerf | 1.12 (1.00, 1.25)* | ||
| Delayed recall | 0.99 (0.96, 1.02) | ||
| Fluency | 1.00 (0.99, 1.01) | ||
| Ever smokedg | 1.14 (1.03, 1.26)* | ||
| Number of chronic conditions | 1.01 (0.98, 1.05) | ||
| Difficulties ADL | 0.90 (0.82, 1.00) | ||
| Difficulties IADL | 1.09 (1.01, 1.18)* |
Note. ADL = activities of daily living; CI = confidence interval; CSC = childhood socioeconomic conditions; IADL = instrumental activities of daily living; OR = odds ratio; Ref = reference category. Models are adjusted for attrition, country, aged squared × education, age squared × occupation, age squared × satisfaction with income. N = 11,604. Satisfaction with income ranges between 1 (great difficulty) and 4 (easily).
aFrailty, reference category non-frail.
bBirth cohort, reference category no war and no economic crisis.
cLiving with biological parents, reference category both parents.
dCSC, reference category most advantaged.
eMain occupation, reference category high occupation.
fPartnership status, reference category with partner.
gSmoking, reference category never.
*p < .05, **p < .01, ***p < .001.
Table 3.
Associations Between Childhood Socioeconomic Conditions and (Pre-)Frailtya at Older Age, Men
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age | 3.44 (2.36, 5.00)*** | 2.75 (1.56, 4.84)*** | 2.70 (1.53, 4.75)** |
| Age squared | 1.41 (1.10, 1.81)** | 1.18 (0.81, 1.72) | 1.16 (0.80, 1.70) |
| Birth cohort, warb | 0.95 (0.81, 1.11) | 0.94 (0.80, 1.10) | 0.95 (0.81, 1.11) |
| Birth cohort, economic crisisb | 0.90 (0.75, 1.08) | 0.87 (0.73, 1.05) | 0.88 (0.74, 1.06) |
| Living with one parentc | 0.88 (0.71, 1.10) | 0.90 (0.72, 1.12) | 0.89 (0.71, 1.11) |
| Living without parentsc | 1.25 (0.81, 1.94) | 1.25 (0.81, 1.93) | 1.21 (0.78, 1.87) |
| CSC advantagedd | 1.27 (0.88, 1.84) | 1.10 (0.76, 1.60) | 1.09 (0.75, 1.57) |
| CSC middled | 1.44 (1.02, 2.04)* | 1.11 (0.78, 1.59) | 1.12 (0.78, 1.59) |
| CSC disadvantagedd | 1.61 (1.13, 2.31)** | 1.11 (0.76, 1.61) | 1.11 (0.77, 1.62) |
| CSC most disadvantagedd | 1.84 (1.27, 2.66)** | 1.16 (0.78, 1.71) | 1.18 (0.80, 1.75) |
| Age × CSC advantagedd | 0.85 (0.55, 1.32) | 0.82 (0.52, 1.28) | 0.83 (0.53, 1.29) |
| Age × CSC middled | 0.95 (0.63, 1.44) | 0.93 (0.61, 1.43) | 0.95 (0.63, 1.45) |
| Age × CSC disadvantagedd | 0.90 (0.60, 1.37) | 0.87 (0.56, 1.35) | 0.88 (0.57, 1.38) |
| Age × CSC most disadvantagedd | 0.97 (0.64, 1.48) | 0.93 (0.58, 1.49) | 0.94 (0.59, 1.50) |
| Level of education in years | 0.98 (0.96, 1.00)* | 0.98 (0.96, 1.00)* | |
| Age × education | 1.02 (0.99, 1.04) | 1.02 (0.99, 1.04) | |
| Main occupation, lowe | 1.32 (1.10, 1.59)** | 1.29 (1.07, 1.55)** | |
| Age × low occupatione | 1.17 (0.93, 1.48) | 1.17 (0.93, 1.48) | |
| Satisfaction with income | 1.37 (1.27, 1.48)*** | 1.36 (1.26, 1.47)*** | |
| Age × satisfaction with income | 1.02 (0.93, 1.12) | 1.02 (0.93, 1.13) | |
| Partnership, without partnerf | 1.36 (1.19, 1.63)*** | ||
| Delayed recall | 0.99 (0.96, 1.03) | ||
| Fluency | 1.00 (0.99, 1.01) | ||
| Ever smokedg | 1.12 (1.00, 1.27) | ||
| Number of chronic conditions | 0.98 (0.94, 1.02) | ||
| Difficulties ADL | 1.04 (0.92, 1.17) | ||
| Difficulties IADL | 1.02 (0.93, 1.12) |
Note. ADL = activities of daily living; CI = confidence interval; CSC; childhood socioeconomic conditions; IADL = instrumental activities of daily living; OR = odds ratio; Ref = reference category. Models are adjusted for attrition, country, aged squared × education, age squared × occupation, age squared × satisfaction with income. N = 9,581. Satisfaction with income ranges between 1 (great difficulty) and 4 (easily).
aFrailty, reference category non-frail.
bBirth cohort, reference category no war and no economic crisis.
cLiving with biological parents, reference category both parents.
dCSC, reference category most advantaged.
eMain occupation, reference category high occupation.
fPartnership status, reference category with partner.
gSmoking, reference category never.
*p < .05, **p < .01, ***p < .001.
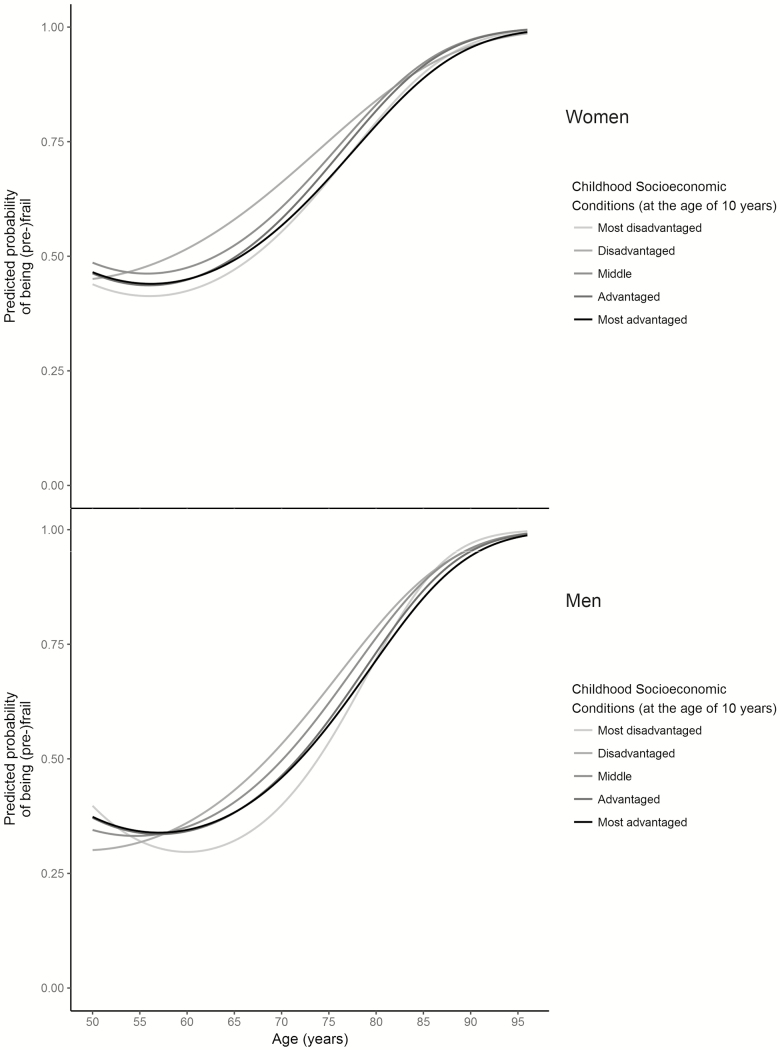
Figure 1 shows the predicted probability of being (pre-)frail in women and men for each CSC (Model 1). The figure suggests a difference between the CSC that is relatively stable, but diminishes from age 85 onwards.
Figure 1.
Predicted probability of being (pre-)frail for each childhood socioeconomic condition, adjusteda. aAdjusted for age, age squared, attrition, birth cohort, living with biological parents, age*CSC, age squared*CSC (see Tables 2 and 3, Model 1).
Effects of ASC on Risk of Frailty Over Aging
When educational attainment, main occupational class, and satisfaction with household income were added as potential mediators in the model including CSC, results indicated that these indicators of ASC mediate the association of CSC with odds of being (pre-)frail in both women and men (see Model 2 in Tables 2 and 3).
In both women and men, lower education, having a low-skilled job, and higher satisfaction with income were associated with higher odds of (pre-)frailty. Regarding the health- and lifestyle variables, living without a partner increased the odds of being (pre-)frail in both women and men. Having smoked and more difficulties with IADL were associated with higher odds of being (pre-)frail in women (see Model 3 in Tables 2 and 3).
The results of the sensitivity analyses for frailty as dichotomous outcome comparing non-frail to pre-frail can be found in the Supplementary Tables 5 and 6. For the other sensitivity analyses as well as results from ordinal multilevel regression models, tables are not shown. Overall, the results of the sensitivity analyses were consistent with these findings in the main analyses.
Discussion
In this study, the association of CSC, ASC, and other life course factors with (pre-)frailty at older age was analyzed using large scale, multinational, longitudinal data. With respect to our first research question, results showed a relation between CSC and the odds of being (pre-)frail in both women and men: the more disadvantaged the CSC, the higher the odds of being (pre-)frail. However, these results no longer hold when looking at our second research question, the effects of ASC (i.e., level of education, main occupation class, and level of household income) on the relation between CSC and frailty, as findings showed that ASC mediated the effect of CSC on the odds of being (pre-)frail in both women and men.
Our findings corroborate cross-sectional studies showing a relationship between disadvantaged socioeconomic conditions over the life course, measured by, amongst others, education, standard of living, and household income, and a higher risk of frailty in old age in France, Italy, and Latin America (Alvarado, Zunzunegui, Beland, & Bamvita, 2008; Herr, Robine, Aegerter, Arvieu, & Ankri, 2015; Poli et al., 2017). Our study went further by showing that socioeconomic differences persisted over age, and even increased among women. Two studies from Latin America and the United Kingdom support our findings of a relationship between poor CSC and higher odds of frailty in both men and women (Alvarado et al., 2008; Gale, Booth, Starr, & Deary, 2016). Our study added to these findings by using a more comprehensive indicator of CSC. Other research supports the idea that not only CSC, but also socioeconomic circumstances across the life course are determinants of frailty in later life. Alvarado and colleagues found that adulthood and current social conditions, measured as low education, non-white collar occupation, and insufficient income, were cross-sectionally associated with higher odds of frailty in both men and women (Alvarado et al., 2008). Gardiner and colleagues studied frailty trajectories in older women and found that late-life socioeconomic status has a strong impact on frailty, but did not look at the effects of CSC (Gardiner, Mishra, & Dobson, 2016). Similar to the findings in the present study, they found that women who had difficulties in managing their income were more likely to be frail. Dury and colleagues also found that older people who had a lower household income were more at risk for frailty (Dury et al., 2017). Similarly, Herr and colleagues found that the most important risk factor of frailty was a poor level of financial security in old age (Herr et al., 2015). These findings all support the idea that socioeconomic circumstances across the life course are strong determinants of frailty in older age.
Importantly, the present study is the first longitudinal and cross-national European study to reveal that pathways to (pre-)frailty already start in childhood and are associated with CSC. However, what this study adds to the existing knowledge is that these findings on the association with CSC no longer qualify when taking a life-course perspective: taking ASC (i.e., education, occupation, and income) into account mediates the association.
Apart from the findings on socioeconomic conditions, in several exploratory analyses, we also revealed that key demographic variables, such as age and individual differences in life history, such as not having a partner, may be associated with frailty. These results corroborate previous cross-sectional reports on increasing age being associated with increasing prevalence of frailty, or multi-morbidity (Woo, Zheng, Leung, & Chan, 2015). Increased age was also found to be a risk factor for frailty by Dury and colleagues (Dury et al., 2017). Further, they found that having no partner was a risk characteristic, which was also a finding in this study, but only in men. More in-depth research in the findings regarding demographics and personal factors over the life course may help in explaining its pathways with frailty.
Strengths and Limitations
A major strength of this study is the use of a multinational and longitudinal database with a large sample size with a potential observation period of 10 years. Additionally, pre-defined and previously used methods for defining and analyzing socioeconomic conditions and frailty were used, thereby limiting chances of misclassification bias. Also, using the same methods of operationalizing frailty as other SHARE studies makes it easy to compare the results of this study with other SHARE studies. We minimized the health selection bias by including respondents participating in only one wave.
The present study has some limitations. First, information on CSC and ASC was measured retrospectively and was self-reported. The data may, therefore, be subject to recall bias. However, previous research found evidence for the accuracy of recall of simple measures of socioeconomic conditions in a survey of older adults (Lacey, Belcher, & Croft, 2012). Second, as we used longitudinal data, we had participants who dropped out or died during follow-up. However, to deal with this, we adjusted for attrition in the analyses, which is a statistical adjustment for mediator-outcome confounding, although this does not solve the issue of missing data due to attrition. Third, different definitions and methods of operationalizing frailty exist which may lead to different estimates of frailty, depending on the definition used and the population being studied. Even though several SHARE studies used the same operationalization, it may be more difficult to compare to studies using a different operationalization. Yet, this strategy seems most optimal to allow better comparison with other studies using SHARE data. Additionally, in our analyses we combined the pre-frail and frail groups, whereas some other studies only look at frailty (three or more attributes) or a sum score. Even though this may make direct comparison more difficult, in our sensitivity analyses we did not find changes to the main analyses and are thus confident about the associations we found.
Conclusion
The present study is the first longitudinal cross-national European study to analyze the associations of CSC with frailty and explore the role of ASC as mediators in this association. In conclusion, our findings suggest that pathways to (pre-)frailty start in early life. Importantly, they also demonstrate that these effects are mediated by socioeconomic factors later in life. These findings give clear evidence of the long-term impact of socioeconomic conditions over the life course on frailty at older age. This may help in developing public health policies improving frailty trajectories by targeting individuals at risk of becoming frail. Early interventions for (pre-)frail individuals are expected to improve their quality of life and reduce costs of care (Buckinx et al., 2015). Policies aiming to improve socioeconomic conditions in adulthood, can have beneficial effects across the life course and may help in reducing the impact of unfavorable early-life conditions on health inequalities.
Funding
This work was supported by the European Union’s Horizon 2020 research and innovation program under the Marie Sklodowska-Curie Grant (agreement number 676060 [LONGPOP] to B. W. A. van der Linden); and the Swiss National Centre of Competence in Research “LIVES – Overcoming vulnerability: Life course perspectives”, which is financed by the Swiss National Science Foundation (grant number: 51NF40-160590). This article uses data from SHARE Waves 1, 2, 3 (SHARELIFE), 4, 5 and 6 (DOIs: 10.6103/SHARE.w1.600, 10.6103/SHARE.w2.600, 10.6103/SHARE.w3.600, 10.6103/SHARE.w4.600, 10.6103/SHARE.w5.600, 10.6103/SHARE.w6.600). The SHARE data collection was primarily funded by the European Commission through FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812) and FP7 (SHARE-PREP: N°211909, SHARE-LEAP: N°227822, SHARE M4: N°261982). The authors gratefully acknowledge additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C) and various national funding sources (see www.share-project.org).
Author Contributions
B. W. A. van der Linden, B. Cheval, and S. Cullati designed the analyses. B. Cheval and S. Sieber were involved in analyzing the data. B. W. A. van der Linden drafted the manuscript and all authors helped to write and revise the manuscript.
Conflict of Interest
None reported.
Supplementary Material
References
- Alcer K., Benson G., Blom A. G., Börsch-Supan A., Brugiavini A., Christelis D.,…Weerman B (2005). The Survey of Health, Aging, and Retirement in Europe - Methodology. Mannheim, Germany: Mannheim Research Institute for the Economic of Aging. [Google Scholar]
- Alvarado B. E., Zunzunegui M. V., Béland F., & Bamvita J. M (2008). Life course social and health conditions linked to frailty in Latin American older men and women. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 63, 1399–1406. doi:10.1093/gerona/63.12.1399 [DOI] [PubMed] [Google Scholar]
- Bandeen-Roche K., Seplaki C. L., Huang J., Buta B., Kalyani R. R., Varadhan R.,…Kasper J. D (2015). Frailty in older adults: a nationally representative profile in the United States. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 70, 1427–1434. doi:10.1093/gerona/glv133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D., Mächler M., Bolker B., & Walker S (2015). Fitting Linear Mixed-Effects Models Using lme4. Journal of Statistical Software, 67, 48. doi:10.18637/jss.v067.i01 [Google Scholar]
- Blane D., Kelly-Irving M., d’Errico A., Bartley M., & Montgomery S (2013). Social-biological transitions: how does the social become biological? Longitudinal Life Course Studies, 4, 136–146. doi:10.14301/llcs.v4i2.236 [Google Scholar]
- Boisgontier M. P., & Cheval B (2016). The ANOVA to mixed model transition. Neuroscience and Biobehavioral Reviews, 68, 1004–1005. doi:10.1016/j.neubiorev.2016.05.034 [DOI] [PubMed] [Google Scholar]
- Börsch-Supan A., Brandt M., Hunkler C., Kneip T., Korbmacher J., Malter F.,…Zuber S.; SHARE Central Coordination Team (2013). Data Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). International Journal of Epidemiology, 42, 992–1001. doi:10.1093/ije/dyt088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruer J. T. (2001). A critical and sensitive period primer. In Bailey J. D. B., Bruer J. T., & Symons F. J. (Eds.), Critical thinking about critical periods, pp. 3–26. Baltimore, MD: Paul H. Brookes. [Google Scholar]
- Buckinx F., Rolland Y., Reginster J. Y., Ricour C., Petermans J., & Bruyère O (2015). Burden of frailty in the elderly population: perspectives for a public health challenge. Archives of Public Health, 73, 19. doi:10.1186/s13690-015-0068-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheval B., Boisgontier M. P., Orsholits D., Sieber S., Guessous I., Gabriel R.,…Cullati S (2018). Association of early- and adult-life socioeconomic circumstances with muscle strength in older age. Age and Ageing, 47, 398–407. doi:10.1093/ageing/afy003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chittleborough C. R., Baum F. E., Taylor A. W., & Hiller J. E (2006). A life-course approach to measuring socioeconomic position in population health surveillance systems. Journal of Epidemiology and Community Health, 60, 981–992. doi:10.1136/jech.2006.048694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg A., Young J., Iliffe S., Rikkert M. O., & Rockwood K (2013). Frailty in elderly people. Lancet (London, England), 381, 752–762. doi:10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannefer D. (2003). Cumulative advantage/disadvantage and the life course: cross-fertilizing age and social science theory. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 58, S327–S337. doi:10.1093/geronb/58.6.S327 [DOI] [PubMed] [Google Scholar]
- Dedman D. J., Gunnell D., Davey Smith G., & Frankel S (2001). Childhood housing conditions and later mortality in the Boyd Orr cohort. Journal of Epidemiology and Community Health, 55, 10–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doku D. T., Acacio-Claro P. J., Koivusilta L., & Rimpela A (2018). Health and socioeconomic circumstances over three generations as predictors of youth unemployment trajectories. European Journal of Public Health. Ahead of print 2018 Nov 22. doi:10.1093/eurpub/cky242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dury S., De Roeck E., Duppen D., Fret B., Hoeyberghs L., Lambotte D.,…Dierckx E (2017). Identifying frailty risk profiles of home-dwelling older people: focus on sociodemographic and socioeconomic characteristics. Aging & mental health, 21, 1031–1039. doi:10.1080/13607863.2016.1193120 [DOI] [PubMed] [Google Scholar]
- Etman A., Burdorf A., Van der Cammen T. J., Mackenbach J. P., & Van Lenthe F. J (2012). Socio-demographic determinants of worsening in frailty among community-dwelling older people in 11 European countries. Journal of Epidemiology and Community Health, 66, 1116–1121. doi:10.1136/jech-2011-200027 [DOI] [PubMed] [Google Scholar]
- Etman A., Kamphuis C. B., van der Cammen T. J., Burdorf A., & van Lenthe F. J (2015). Do lifestyle, health and social participation mediate educational inequalities in frailty worsening? European Journal of Public Health, 25, 345–350. doi:10.1093/eurpub/cku093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans M. D., Kelley J., Sikora J., & Treiman D. J (2010). Family scholarly culture and educational success: Books and schooling in 27 nations. Research in Social Stratification and Mobility, 28, 171–197. doi:10.1016/j.rssm.2010.01.002 [Google Scholar]
- Franse C. B., van Grieken A., Qin L., Melis R. J. F., Rietjens J. A. C., & Raat H (2017). Socioeconomic inequalities in frailty and frailty components among community-dwelling older citizens. PLoS One, 12, e0187946. doi:10.1371/journal.pone.0187946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Tangen C. M., Walston J., Newman A. B., Hirsch C., Gottdiener J.,…McBurnie M. A.; Cardiovascular Health Study Collaborative Research Group (2001). Frailty in older adults: evidence for a phenotype. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 56, M146–M156. doi:10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- Gale C. R., Booth T., Starr J. M., & Deary I. J (2016). Intelligence and socioeconomic position in childhood in relation to frailty and cumulative allostatic load in later life: the Lothian Birth Cohort 1936. Journal of Epidemiology and Community Health, 70, 576–582. doi:10.1136/jech-2015-205789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gardiner P. A., Mishra G. D., & Dobson A. J (2016). The effect of socioeconomic status across adulthood on trajectories of frailty in older women. Journal of the American Medical Directors Association, 17, 372.e1–372.e3. doi:10.1016/j.jamda.2015.12.090 [DOI] [PubMed] [Google Scholar]
- Gill T. M., Gahbauer E. A., Allore H. G., & Han L (2006). Transitions between frailty states among community-living older persons. Archives of Internal Medicine, 166, 418–423. doi:10.1001/archinte.166.4.418 [DOI] [PubMed] [Google Scholar]
- Herr M., Robine J. M., Aegerter P., Arvieu J. J., & Ankri J (2015). Contribution of socioeconomic position over life to frailty differences in old age: comparison of life-course models in a French sample of 2350 old people. Annals of Epidemiology, 25, 674–680.e1. doi:10.1016/j.annepidem.2015.05.006 [DOI] [PubMed] [Google Scholar]
- Hoogendijk E. O., van Hout H. P., Heymans M. W., van der Horst H. E., Frijters D. H., Broese van Groenou M. I.,…Huisman M (2014). Explaining the association between educational level and frailty in older adults: results from a 13-year longitudinal study in the Netherlands. Annals of Epidemiology, 24, 538–44.e2. doi:10.1016/j.annepidem.2014.05.002 [DOI] [PubMed] [Google Scholar]
- Klevmarken A., Swensson B., Hesselius P (2005). The SHARE sampling prodecures and calibrated design weights. In Börsch-Supan A., & Jürges H. (Eds.), The Survey of Health, Aging and Retirement in Europe: Methodology (pp. 28–69). Mannheim, Germany: Mannheim Research Institute for the Economics of Aging. [Google Scholar]
- Kuh D., & Ben-Shlomo Y (2004). A life course approach to chronic disease epidemiology. Oxford, UK: Oxford University Press. [PubMed] [Google Scholar]
- Kuh, D., Cooper, R., Hardy R., Richards, M., & Ben-Shlomo, Y. (Eds.). (2013). A life course approach to healthy ageing. New York, United States of America: Oxford University Press. [Google Scholar]
- Kuznetsova A., Brockhoff P. B., Christensen R. H. B (2016). ImerTest: Tests in Linear Mixed Effects Models. R package version 2.0–33 Retrieved from https://CRAN.R-project.org/package=lmerTest
- Lacey R. J., Belcher J., & Croft P. R (2012). Validity of two simple measures for estimating life-course socio-economic position in cross-sectional postal survey data in an older population: results from the North Staffordshire Osteoarthritis Project (NorStOP). BMC Medical Research Methodology, 12, 88. doi:10.1186/1471-2288-12-88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazar M., & Davenport L (2018). Barriers to health care access for low income families: a review of literature. Journal of Community Health Nursing, 35, 28–37. doi:10.1080/07370016.2018.1404832 [DOI] [PubMed] [Google Scholar]
- Luo Y., & Waite L. J (2005). The impact of childhood and adult SES on physical, mental, and cognitive well-being in later life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 60, S93–S101. doi:10.1093/geronb/60.2.S93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macklai N. S., Spagnoli J., Junod J., & Santos-Eggimann B (2013). Prospective association of the SHARE-operationalized frailty phenotype with adverse health outcomes: evidence from 60+ community-dwelling Europeans living in 11 countries. BMC Geriatrics, 13, 3. doi:10.1186/1471-2318-13-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsh A., Gordon D., Pantazis C., & Heslop P (1999). Home sweet home? The impact of poor housing on health. Bristol, UK: The Policy Press, University of Bristol. [Google Scholar]
- Marshall A., Nazroo J., Tampubolon G., & Vanhoutte B (2015). Cohort differences in the levels and trajectories of frailty among older people in England. Journal of Epidemiology and Community Health, 69, 316–321. doi:10.1136/jech-2014-204655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poli S., Cella A., Puntoni M., Musacchio C., Pomata M., Torriglia D.,…Pilotto A (2017). Frailty is associated with socioeconomic and lifestyle factors in community-dwelling older subjects. Aging Clinical and Experimental Research, 29, 721–728. doi:10.1007/s40520-016-0623-5 [DOI] [PubMed] [Google Scholar]
- R Core Team (2017). R: A language and environment for statistical computing. Retrieved from https://www.R-project.org/ [Google Scholar]
- Romero-Ortuno R. (2013). The SHARE operationalized frailty phenotype: a comparison of two approaches. Eur Geriatr Med, 4, 255–259. doi:10.1016/j.eurger.2013.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos-Eggimann B., Cuénoud P., Spagnoli J., & Junod J (2009). Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 64, 675–681. doi:10.1093/gerona/glp012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schröder M. (2011). Retrospective Data Collection in the Survey of Health, Ageing and Retirement in Europe. SHARELIFE Methodology. Mannheim, Germany: Mannheim Research Institute for the Economics of Ageing. [Google Scholar]
- Sharpe R. A., Taylor T., Fleming L. E., Morrissey K., Morris G., & Wigglesworth R (2018). Making the case for “Whole System” Approaches: integrating public health and housing. International Journal of Environmental Research and Public Health, 15, 2345. doi:10.3390/ijerph15112345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soler-Vila H., García-Esquinas E., León-Muñoz L. M., López-García E., Banegas J. R., & Rodríguez-Artalejo F (2016). Contribution of health behaviours and clinical factors to socioeconomic differences in frailty among older adults. Journal of Epidemiology and Community Health, 70, 354–360. doi:10.1136/jech-2015-206406 [DOI] [PubMed] [Google Scholar]
- Stolz E., Mayerl H., Waxenegger A., Rásky É., & Freidl W (2017). Impact of socioeconomic position on frailty trajectories in 10 European countries: evidence from the Survey of Health, Ageing and Retirement in Europe (2004-2013). Journal of Epidemiology and Community Health, 71, 73–80. doi:10.1136/jech-2016-207712 [DOI] [PubMed] [Google Scholar]
- Strachan D. P., & Sheikh A (2004). A life course approach to respiratory and allergic diseases. In Kuh D. & Ben Shlomo Y. (Eds.), A life course approach to chronic disease epidemiology (pp. 240–259). Oxford, UK: Oxford University Press. [Google Scholar]
- Stringhini S., Polidoro S., Sacerdote C., Kelly R. S., van Veldhoven K., Agnoli C.,…Vineis P (2015). Life-course socioeconomic status and DNA methylation of genes regulating inflammation. International Journal of Epidemiology, 44, 1320–1330. doi:10.1093/ije/dyv060 [DOI] [PubMed] [Google Scholar]
- Vineis P., Kelly-Irving M., Rappaport S., & Stringhini S (2016). The biological embedding of social differences in ageing trajectories. Journal of Epidemiology and Community Health, 70, 111–113. doi:10.1136/jech-2015-206089 [DOI] [PubMed] [Google Scholar]
- Wahrendorf M., & Blane D (2015). Does labour market disadvantage help to explain why childhood circumstances are related to quality of life at older ages? Results from SHARE. Aging & Mental Health, 19, 584–594. doi:10.1080/13607863.2014.938604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wahrendorf M., Blane D., Bartley M., Dragano N., & Siegrist J (2013). Working conditions in mid-life and mental health in older ages. Advances in Life Course Research, 18, 16–25. doi:10.1016/j.alcr.2012.10.004 [DOI] [PubMed] [Google Scholar]
- Woo J., Zheng Z., Leung J., & Chan P (2015). Prevalence of frailty and contributory factors in three Chinese populations with different socioeconomic and healthcare characteristics. BMC Geriatrics, 15, 163. doi:10.1186/s12877-015-0160-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.