Abstract
Dehydration due to diarrhea is one of the main causes of death worldwide, yet no clinical tools for accurately assessing and managing dehydration in patients with acute diarrhea have been created for low- and middle-income countries (LMICs). In 2012, Brown University’s Department of Emergency Medicine began partnering with the International Centre for Diarrhoeal Disease, Bangladesh in order to address some of these gaps. Out of this partnership, the DHAKA Score, a clinical diagnostic model for assessing dehydration in children under five years of age with acute diarrhea, was developed. Building upon the success of the DHAKA Study, researchers at both institutions have launched the NIRUDAK Study earlier this year to develop and validate similar age-specific clinical diagnostic models yet shifting the patient population to those over five. Improving diagnostic approaches and fluid management may reduce unnecessary utilization of already limited healthcare resources as well as the morbidity and mortality that occurs due to misdiagnosis.
Keywords: dehydration assessment, diarrhea management, mHealth, developing country or LMIC
BACKGROUND
Globally, diarrhea remains one of the most common and deadly acute conditions, second only to upper respiratory infections. According to the Global Burden of Disease Study in 2015, there were nearly 2.4 billion cases of acute diarrheal illness globally.1 However, there may, in fact, be many more cases as medical care is sought in fewer than 30–50% of cases in resource limited settings.2 While the typical course of diarrheal illness is self-limiting and benign, approximately 5% of cases in adults and older children (21.5 million diarrheal episodes annually) result in higher disease severity thus requiring advanced medical management.2 Despite recent strides in combating mortality, diarrheal disease is still the 5th leading cause of years of life lost globally, accounting for more than 1.3 million deaths annually, including 813,000 deaths in adults and children over five years of age.3
While a sizeable body of research on diarrheal illness in children under five years of age exists, less is understood about diarrheal illness in older children and adults. In comparison to the common viral causes of diarrheal illness in children less than five years of age, such as rotavirus and norovirus, bacterial causes predominate in older children, adolescents, adults, and the elderly globally.4 Worldwide, Vibrio cholerae O1/O139 and Enterotoxigenic Escherichia coli (ETEC) are the most common causes of acute diarrhea in hospitalized patients over five years of age, while Salmonella and Shigella species were the most common etiologies in outpatient settings.4 Evidence suggests that the elderly are especially at risk for higher diarrhea morbidity and mortality in both high-income countries as well as in low- and middle-income countries (LMIC). In the United States, 83% of all diarrheal deaths occur in patients over age 65.5,6 In Dhaka, Bangladesh, patients over 60 years of age with acute diarrheal illnesses are more likely to require hospital admission and have a more severe course of illness than younger patients.5,6 This difference in disease severity could be attributed to various reasons including age-related structural and functional gastrointestinal tract changes, underlying chronic illnesses, concomitant use of medications, impaired sense of thirst, poor baseline nutrition and hydration status or a more subtle clinical presentation of diarrheal illness.6
Based on their Integrated Management of Childhood Illness (IMCI) strategy, the World Health Organization (WHO) currently recommends assessing children under five years of age presenting with acute diarrhea for dehydration and classifying their level of dehydration severity into three categories: severe, some, or none based on the presence of four different clinical signs.7 For children with severe dehydration, immediate treatment with intravenous fluid is recommended, while those with some dehydration should receive oral rehydration solution (ORS). Those with no dehydration require only expectant management.7 The IMCI dehydration algorithm still remains the most common clinical tool for assessing dehydration status. However, several studies have found it to be a poor predictor of dehydration when compared to the gold standard of percentage weight change with rehydration.8–10
Several research institutions and organizations have attempted to develop better tools for assessing dehydration in children. The most commonly used diagnostic dehydration scales include the Clinical Dehydration Scale (CDS; created at the Hospital for Sick Children in Toronto) and the Gorelick Scale (developed at the Children’s Hospital of Philadelphia).8 While prior studies have found these tools to be relatively accurate for predicting dehydration in young children in high-income country settings, they have not been well validated in low- and middle-income countries nor have they been tested in older children or adults.8,11–15 the Gorelick scale, and the Clinical Dehydration Scale (CDS Misclassification of dehydration is a significant diagnostic problem as underestimation of a patient’s dehydration status could potentially result in further medical complications, such as acute renal failure or even death, while overestimation could result in increased risk of hospital-related adverse events, additional hospital expenses as well as increased burden on the patient’s family, especially in low- and middle-income countries.8,14,16
RESEARCH SETTING AND PARTNERSHIP
Initially founded in the early 1960s under the South-East Asia Treaty Organization, Cholera Research Laboratory (now known as the International Centre for Diarrhoeal Disease Research, Bangladesh or more simply icddr,b since 1978) has developed an international reputation as a preeminent research/treatment center for developing and testing interventions specifically designed to the meet the needs of Bangladesh and other LMICs.17 Such areas of research include malnutrition, respiratory disease, vaccine testing, maternal and child health and health systems. Research conducted at icddr,b has produced innovative solutions to some of the most prominent global health concerns and generated evidence that has influenced health policy globally. A few of the its most notable achievements include the development of the ORS, providing key evidence underpinning the WHO’s decision to recommend zinc as a way to shorten the duration and prevent future cases of diarrhea, providing data that illustrated maternal immunization with tetanus toxoid before pregnancy protects mothers from neonatal tetanus, and detailing treatment guidelines for severe malnutrition that are now standardized protocol endorsed by the WHO.17
Icddr,b’s commitment to developing high-quality research studies has led to its robust network of scientific collaborators and implementing partners worldwide. In 2012, Brown University’s Department of Emergency Medicine began partnering with icddr,b in order to address some of the above-mentioned gaps in diagnostic tools to assist clinicians in assessing and managing dehydration in patients with acute diarrhea in LMICs. Through a five-year research grant from the United States National Institutes of Health (NIH) Fogarty International Center (PI Levine, K01TW009208), researchers at Brown University and icddr,b collaborated on the DHAKA Study together to develop and test new clinical prediction models, ultrasound-based tools and mobile health tools for assessing dehydration in young children under five in Bangladesh.
DEHYDRATION ASSESSMENT IN YOUNG CHILDREN
As part of this research, the DHAKA (Dehydration: Assessing Kids Accurately) Score, the first clinical diagnostic model for assessing dehydration in children under five years of age with acute diarrhea in LMIC settings, was developed.16 The DHAKA Score was empirically derived and externally validated in a low-income country, to avoid the limitations of the other models, like CDS.12,13 Using the gold standard of percent weight change with rehydration, the DHAKA Score categorized patients as severe dehydration (>9% weight change), some dehydration (3–9% weight change) or no dehydration (<3% weight change).18 Of children enrolled in the study, 49% had no dehydration, 37% had some dehydration and 14% had severe dehydration.16 Each 1-point increase in the DHAKA Score was found to predict an increase of 0.6% in percent dehydration and increase the odds of dehydration by 1.4.16 When compared to the IMCI algorithm, both the accuracy and reliability of the DHAKA score were superior.16
The use of mHealth tools can also facilitate the evaluation of dehydration in patients with diarrhea, with a study showing greater reliability when an mHealth-supported WHO algorithm was used rather than the standard WHO algorithm printed on a laminated card.19 In conjunction with clinical predictor tools, point-of-care ultrasound can be a useful adjuvant in predicting dehydration in children with diarrhea. By measuring aorta-to-IVC ratio, point-of-care ultrasound has been shown to be a significant predictor of the percent dehydration, with each 1-point increase predicting a 1.1% increase in the percent dehydration.20 However, the sensitivity and specificity were not sufficiently robust for it to be used as an independent screening tool.
DEHYDRATION ASSESSMENT IN OLDER CHILDREN AND ADULTS
Despite the progress in evaluating and developing a clinical diagnostic scale, the patient population for such diagnostic tools has predominantly been children under five years of age. This leaves out a significant portion of patients who are also affected by diarrheal illnesses – those over five. As such, researchers at Brown University and icddr,b have continued their partnership and launched the NIRUDAK Study earlier this year at icddrb,b’s Dhaka Hospital (Figure 1) to address the above-mentioned limitations. NIRUDAK, which means “dehydrated” in Bangla, stands for Novel Innovative Research for Understanding Dehydration in Adults and Kids. The overall objective of this prospective study is to develop and validate new age-specific clinical diagnostic models to assess dehydration, thereby building upon the success of the DHAKA Study.16,18,19 However, the focus of the study will be in patients over five years of age presenting with acute diarrhea. Once these age-specific models are developed, they will be incorporated into a mobile health application so that clinicians will not only be able to more accurately diagnose dehydration severity but will also better determine the optimal management strategy for patients with acute diarrhea.
Figure 1.

Emergency ward at icddr,b’s Dhaka Hospital. [PHOTO : DR. SABIHA NA SRIN]
The aim of the NIRUDAK Study is threefold:
To derive and internally validate three age-specific clinical diagnostic models for the assessment of dehydration severity in older children/adolescents, adults and the elderly.
To incorporate these models into a mobile health tool to be used by clinicians.
To validate this mobile health tool in a new population of patients.
NIRUDAK Study’s research aims will be accomplished through two large, prospective observational studies, which will occur in three phases over the next five years. The first phase will focus on achieving Aim 1. During this derivation phase, data on clinical signs and symptoms shown to correlate with dehydration severity will be collected from patients presenting to the rehydration unit of icddr,b. Using advanced machine learning techniques, the best clinical predictors for each individual age group will be selected against the gold standard of percent weight change with rehydration to develop diagnostic models. The second phase, or formative phase, will use the models from the derivation phase to develop an innovative new mobile health tool to guide clinicians in the management of dehydration. Formative focus groups and in-depth interviews will also be conducted to further improve its usability. Finally, in the validation phase the application’s accuracy and reliability will be validated in a new population of patients presenting with acute diarrhea at icddr,b.
Since early June 2019, 503 patients have been enrolled in the first phase of the NIRUDAK study with 53% of them being males and 47% females. So far, 97% of patients enrolled in the study have sufficient follow-up information to calculate their percent weight change with rehydration, our gold standard measure for dehydration. Among those enrolled in the study, 83.1% were characterized as being severely dehydrated by triage nurses and received IV fluid, while the rest were characterized as having some dehydration and given ORS. However, according to the study’s gold standard of percent weight change, only 11.1% were severely dehydrated and should have received IV fluids while 60.7% had some dehydration and 28.2% of patients had no significant dehydration. (Figures 2,3)
Figure 2.
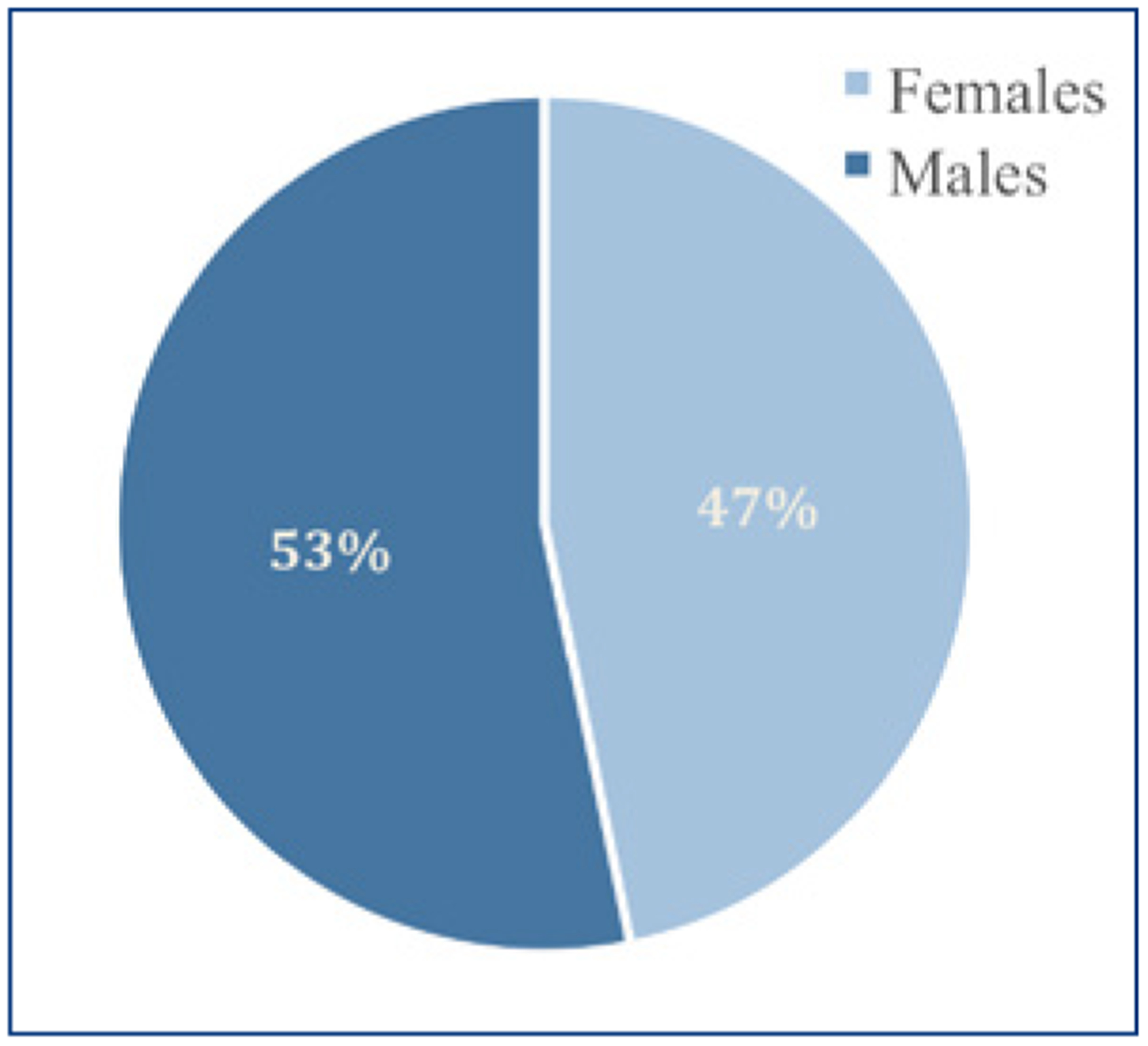
Sex Distribution of Patients Enrolled in NIRUDAK Study as of June 2019
Figure 3.
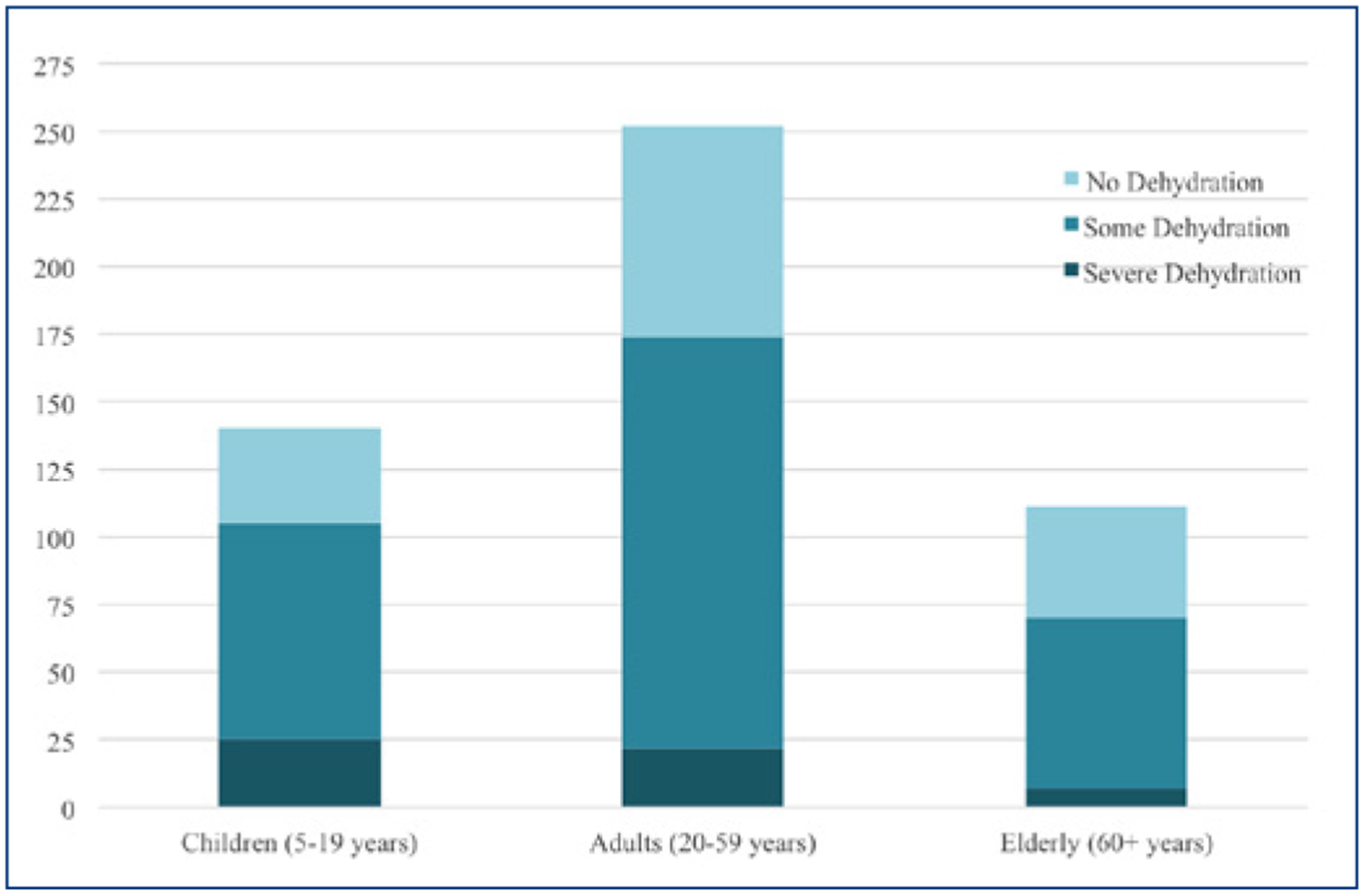
Dehydration Status Distribution within Each Age Group of Patients Enrolled in the NIRUDAK Study
CONCLUSION
Developing such models, like the DHAKA Score and the upcoming NIRUDAK Score, and incorporating them into mobile health applications has the potential to help clinicians rapidly and accurately not only determine the severity of dehydration in patients with acute diarrhea but also choose the optimal rehydration strategy. Those 28.2% of enrolled patients who were admitted with no significant dehydration would have most likely received expectant management at home rather than IV fluids and/or ORS with the help of such diagnostic tools. While the intended use of this tool will be in hospitals or clinics by hospital staff, one of the major uses will be during epidemics of cholera in humanitarian settings, where the numbers of patients can overwhelm available resources. Additionally, this tool can be incorporated into international/local guidelines for dehydration management. Making such distinctions in characterizing dehydration could reduce unnecessary utilization of already limited healthcare resources. More importantly, improved diagnostic approaches and fluid management may in turn be shown to reduce both the morbidity and mortality that occurs as a result of misdiagnosis.
Acknowledgment
We would like to thank the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) for their support and the National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases for providing funding for the NIRUDAK Study (PI Levine, 1R01DK116163-01A1).
Footnotes
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The views expressed within this article are those of the authors and do not necessarily represent the views of icddr,b nor the National Institutes of Health.
Contributor Information
MONIQUE GAINEY, Clinical Research Program Coordinator, Rhode Island Hospital..
MEAGAN BARRY, Department of Emergency Medicine, Warren Alpert Medical School of Brown University..
ADAM C. LEVINE, Associate Professor of Emergency Medicine; Director, Division of Global Emergency Medicine, Warren Alpert Medical School of Brown University..
SABIHA NASRIN, Medical Officer, International Centre for Diarrheal Disease, Bangladesh icddr,b..
References
- 1.GBD 2015 Disease and Injury and Prevalence Collaborators. Global, regional and national incidence, prevalence and years lived with disability for 310 diseases and injuries, 1990 – 2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lamberti L, Fischer Walker C, Sack D, Black R. Systematic review of diarrhea duration and severity in children and adults in low- and middle-income countries. BMC Public Health. 2012;12(276). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mortality GBD C of DC. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(1459):544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fischer Walker CL, Sack D, Black RE. Etiology of diarrhea in older children, adolescents and adults: a systematic review. PLos Negl Trop Dis. 2010;4(768). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hall A, Curns A, McDonald L, Parashar U, Lopman B. The roles of Clostridium difficile and norovirus among gastroenteritis-associated deaths in the United States, 1999 – 2007. Clin Infect Dis. 2012;55(216):23. [DOI] [PubMed] [Google Scholar]
- 6.Faruque ASG, Malek MA, Khan A, Huq S, Salam M, Sack D. Diarrhoea in elderly people: aetiology, and clinical characteristics. Scand J Infect Dis. 2004;36(204):8. [DOI] [PubMed] [Google Scholar]
- 7.WHO. IMCI: Integrated Management of Childhood Illness; 2005.
- 8.Pringle K, Shah SP, Umulisa I, et al. Comparing the accuracy of the three popular clinical dehydration scales in children with diarrhea. Int J Emerg Med. 2011;4(1):58. doi: 10.1186/1865-1380-4-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Levine AC, Munyaneza RM, Glavis-Bloom J, et al. Prediction of Severe Disease in Children with Diarrhea in a Resource-Limited Setting. Carlo WA, ed. PLoS One. 2013;8(12):e82386. doi: 10.1371/journal.pone.0082386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jauregui J, Nelson D, Choo E, et al. External Validation and Comparison of Three Pediatric Clinical Dehydration Scales. Carlo WA, ed. PLoS One. 2014;9(5):e95739. doi: 10.1371/journal.pone.0095739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kinlin LM, Freedman SB. Evaluation of a Clinical Dehydration Scale in Children Requiring Intravenous Rehydration. Pediatrics. 2012;129(5):e1211–e1219. doi: 10.1542/peds.2011-2985 [DOI] [PubMed] [Google Scholar]
- 12.Falszewska A, Szajewska H, Dziechciarz P. Diagnostic accuracy of three clinical dehydration scales: a systematic review. Arch Dis Child. 2018;103(4):383–388. doi: 10.1136/archdis-child-2017-313762 [DOI] [PubMed] [Google Scholar]
- 13.Falszewska A, Dziechciarz P, Szajewska H. The diagnostic accuracy of Clinical Dehydration Scale in identifying dehydration in children with acute gastroenteritis: a systematic review. Clin Pediatr. 2014;53(1181):8. [DOI] [PubMed] [Google Scholar]
- 14.Pomorska D, Dziechciarz P, Mduma E, Gidion J, Falszewska A, Szajewska H. Comparison of three dehydration scales showed that they were of limited or no value for assessing small children with acute diarrhoea. Acta Paediatr. 2018;107(7):1283–1287. doi: 10.1111/apa.14284 [DOI] [PubMed] [Google Scholar]
- 15.Falszewska A, Dziechciarz P, Szajewska H. Diagnostic accuracy of clinical dehydration scales in children. Eur J Pediatr. 2017;176(8):1021–1026. doi: 10.1007/s00431-017-2942-8 [DOI] [PubMed] [Google Scholar]
- 16.Levine A, Glavis-Bloom J, Modi P, Al E. External validation of the DHAKA score and comparison with the current IMCI algorithm for the assessment of dehydration in children with diarrhoea: a prospective cohort study. Lancet Glob Heal. 2016;4(744):51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.icddr,b - About us. https://www.icddrb.org/about-us. Accessed June 12, 2019.
- 18.Levine A, Glavis-Bloom J, Modi P, Al E. Empirically Derived Dehydration Scoring and Decision Tree Models for Children With Diarrhea: Assessment and Internal Validation in a Prospective Cohort Study in Dhaka, Bangladesh. Glob Heal Sci Pr. 2015;3(405):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meisner L, Bilal S, Nelson E, et al. Evaluation of standard and mobile health (mHealth)-supported clinical diagnostic tools for assessing dehydration in patients with diarrhea in rural Bangladesh. In: ASTMH 66th Annual Meeting; 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Modi P, Glavis-Bloom J, Nasrin S, et al. Accuracy of Inferior Vena Cava Ultrasound for Predicting Dehydration in Children with Acute Diarrhea in Resource-Limited Settings. Simeoni U, ed. PLoS One. 2016;11(1):e0146859. doi: 10.1371/journal.pone.0146859 [DOI] [PMC free article] [PubMed] [Google Scholar]


