Abstract
Introduction:
Automated blood pressure (BP) monitor is widely used to assess the blood pressure (BP) of the study subjects in community-based researches. This study aims at the detection of hypertension by automated BP device and examines the concordance and validity between automated and mercury-free LED BP devices.
Materials and Methods:
This cross-sectional study was conducted in the tribal state of Jharkhand in India from January 2017 to June 2017. A total of 300 study participants aged more than 18 years were enrolled in this study. BP of the patients in the sitting position was measured three times each by automated device and mercury-free LED BP device. The different sets of readings were assessed by concordance correlation coefficient (CCC) and other validity measures.
Results:
The CCC for systolic and diastolic BP measured by automated and mercury-free LED BP is 0.88 and 0.85, respectively. The mean difference between systolic and diastolic BP by both the instruments is statistically insignificant (P > 0.05). The sensitivity, specificity, PPV, NPV, and accuracy of automated BP devices to predict hypertension is 96.61%, 92.21%, 75%, 99%, and 93%. The area under ROC for systolic and diastolic BP is 0.984 and 0.97, respectively with P values < 0.0001 in both the cases.
Conclusions:
This study concluded that the overall automated BP machine has fair degree of agreement (CCC) with a manual BP device. The validity of this monitor to screen hypertension may also be considered in field settings.
Keywords: Automated BP device, concordance correlation coefficient, kappa statistic, mercury-free LED BP instrument, validity
Background
The automated (electronic) blood pressure (BP) measurement devices are becoming more prevalent in healthcare settings. Although current guidelines for screening, diagnosis, and treatment of hypertension in clinical practice are still based on clinical trials and epidemiological evidence derived from readings taken with auscultatory devices (usually mercury BP devices),[1] it is widely established that the manual recordings of BP by auscultatory devices are more reliable and accurate in some patients than the automated devices. Despite this fact, the majority healthcare systems have adopted the use of automated devices for the routine recording of BP. The most notable one amongst many reasons for this is that in most of the settings, vital measurements are being recorded by least experienced staff, students, and healthcare assistants.[2,3,4] The correct estimation of BP is the cornerstone of assessing patient's cardiovascular and hemodynamic functioning and detecting hypertension which is one of the major contemporary public health problems. It also forms the key component in the identification of patient deterioration and important measures in physiological track and trigger systems used in adults and children.
The gold standard for measuring BP is through the arterial line but is majorly reserved for critically ill patients. Hence, for routine estimation of BP, noninvasive methods such as auscultation are used outside critical care settings. In regards to correct estimation of BP in noninvasive settings, mercury BP devices are considered as the gold standard for long and BP measurement of mercury instruments (in mmHg) is still considered for all practical purposes all over the world.[5] However, the fear of potential mercury toxicity along with the problems associated with the disposal of mercury, has led to a decrease in the use of mercury instruments worldwide. For the same reason, the European Union directed phasing out of mercury instruments recently.[6] Non-mercury BP devices like aneroid and more recently, digital ones have replaced the use of traditional mercury instruments in many settings. Instead of mercury BP devices, mercury-free LED BP device is available to avoid the precarious effect of mercury. An additional advantage of an aneroid instrument is the portability while that of digital instruments is the ease of use in view of the obvious fact that the latter obviates the need for auscultation skill of the examiner.[7,8,9,10]
In an assay validation or instrument validation process, the reproducibility of the measurement from trial to trial is of interest. Moreover, when a new assay or instrument is developed it is an interest to evaluate the new instrument that can reproduce the results based on the traditional gold standard assay.[11,12] In a comparison of two instruments, there are statistical methods to measure the degree of agreement between the two. Kappa statistic and weighted-Kappa statistic are appropriate methods to measure the amount of agreement for the nominal and ordinal levels of categorical data, respectively. Lin's introduced the concordance correlation coefficient (CCC) which measures the amount of agreement when the variable of interest is continuous.[13]
The CCC is an index that assesses the agreement between continuous measures made by different observers. At least four methods are used to estimate the CCC: two (Lin's method, variance components) which are defined on the basis that data were normally distributed, and the two others (U-statistics, GEE) which do not assume any particular distribution of the data.[9] The CCC measures the variation of their linear relationship from 45° lines through the origin. This coefficient not only measures how far each observation deviates from the line to fit into the data but also how far this line deviates from the 45° lines through the origin.[14] Nowadays, CCC is commonly used to assess the agreement between methods or raters measuring the response when data are measured on a continuous scale. The present study attempts to estimate the Lin's CCC of automated BP monitor as compared with mercury-free LED BP device and also to validate the accuracy of the automated BP monitor in diagnosing hypertension.
Material and Methods
This cross-sectional study has been carried out at Rural Health Training Centre (RHTC), Ormanjhi, Ranchi from January 2017 to June 2017 which is in administrative control of preventive and social medicine (PSM) department of a teaching hospital of eastern India namely Rajendra Institute of Medical Sciences (RIMS), Ranchi. Based on the prevalence of hypertension in rural India to be 14%,[15] confidence interval (CI) 95%, power of the study to be 80%, and absolute error 4%, the sample size calculated came out to be 289. The sampling frame comprised individuals more than 18 years of age attending RHTC and were selected using a systematic random sampling method from the outpatient department (OPD). On selected days of OPD, the study was carried out on every fifth patient attending OPD who voluntarily agreed to participate in it and care was taken not more than 10 patients were recruited on a single day to maintain the quality of data collection. Thus, a total of 300 study subjects were enrolled and informed consent was taken for their participation after explaining the patient information sheet (PIS) in their local language.
The left-arm BP of the patients in the sitting position was measured by an automated device three times for at least every 5 min interval and readings were recorded by an observer (A) and again repeated assessment of the same patients was done by mercury-free LED BP device (manual BP device) by another observer (B) in the next room to avoid biases. As soon as the reading of one observer (A) had been completed, the study subjects were sent to the observer (B) in another adjacent room for BP measurement. Both observers were blinded to each other regarding the BP reading of the patients. Utmost care was taken in making the patients relaxed for at least 10 min before their BP measurement was done and the time was utilized in explaining the purpose of the study, taking their consent, and finally recruitment in the study. The instruments were calibrated on a daily basis before using it for data collection. This study was conducted on only those days of a week when both the observers A and B were present so that the interobserver variation may be avoided. Before the study both the observers were trained to follow the guidelines of measuring BP using different instruments.[16,17,18] The cutoff for categorizing a patient to be hypertensive is ≥140/90 mmHg as per the guidelines of the Joint National Commission (JNC) VII and VIII.[19]
All readings of both the devices were compiled in MS Excel 2007 and exported to NCSS 11 (@NCSS, LLC, USA) and SPSS version 20 (@IBM, USA) software for data analysis. Degree of agreement (Lin's CCC), Kappa statistic, validity measures, ROC curve of different sets of readings of two machines i.e. automated (@OMRON Model no. HEM 7200) and mercury-free LED BP device (@Diamond Model no: BPDG041) BP machine were assessed and compared. The study was approved by the Institutional Ethics Committee (IEC) of Rajendra Institute of Medical Sciences (RIMS), Ranchi (Jharkhand), India (Vide memo no. 112, Dated : 08/02/2017).
Results
A total of 300 patients were recruited for this study whose BP was assessed using both the BP measuring instruments. The mean age of the patients was 38.86 years with a standard deviation of 15.64 years. The proportion of males and females in the study subjects was 50.33% and 49.67%, respectively. The majority of the patients belonged to religion Hindu (82%), followed by Muslims (11%), and Christian (7%).
The mean and standard deviation (SD) BP with the automated device was 125.92 ± 23.47/74.45 ± 12.20 mmHg compared to 118.28 ± 22.90/72.62 ± 11.13 mmHg for the manual BP with CCC for systolic and diastolic BP is 0.88 and 0.85, respectively [Table 1]. According to the linear regression analysis of the measurements, the regression coefficient for systolic and diastolic measurements of both the instruments is more than 0.95 [Table 2, Figures 1 and 2]. The sensitivity, specificity, PPV, NPV, and accuracy of automated BP devices to predict hypertension is 96.61%, 92.21%, 75%, 99%, and 93%, respectively [Table 3]. The area under ROC for systolic and diastolic BP is 0.984 and 0.97, respectively with P values < 0.0001 in both the cases [Table 4, Figures 3 and 4].
Table 1.
Comparison of systolic and diastolic blood pressure measurements by two instruments
| Method | Mean | SD | Min | Max | R Squared | Correlation | CV | CCC | 95% CI | |
|---|---|---|---|---|---|---|---|---|---|---|
| Systolic blood pressure | Automated blood pressure monitor | 125.9 | 23.47 | 86 | 214 | |||||
| Mercury-free LED BP device | 118.3 | 22.9 | 77 | 189 | 0.88 | 0.94 | 0.07 | 0.89 | (0.86-0.91) | |
| Diastolic blood pressure | Automated blood pressure monitor | 74.45 | 12.2 | 48 | 117 | |||||
| Mercury-free LED BP device | 72.62 | 11.13 | 51 | 111 | 0.75 | 0.87 | 0.08 | 0.85 | (0.82-0.88) |
Table 2.
Regression Coefficient-systolic and diastolic blood pressure
| Parameter | Systolic BP | Diastolic BP | ||
|---|---|---|---|---|
| Intercept B (0) |
Slope B (1) |
Intercept B (0) |
Slope B (1) |
|
| Regression Coefficients | 12.31 | 0.96 | 5.40 | 0.95 |
| Lower 95% C.L. | 7.39 | 0.92 | 0.83 | 0.89 |
| Upper 95% C.L. | 17.23 | 1.0 | 9.97 | 1.01 |
| Standard Error | 2.50 | 0.02 | 2.32 | 0.03 |
| T | 4.92 | 46.26 | 2.32 | 30.06 |
| Probability level (t-test) | 0.00 | 0.00 | 0.02 | 0.00 |
Figure 1.
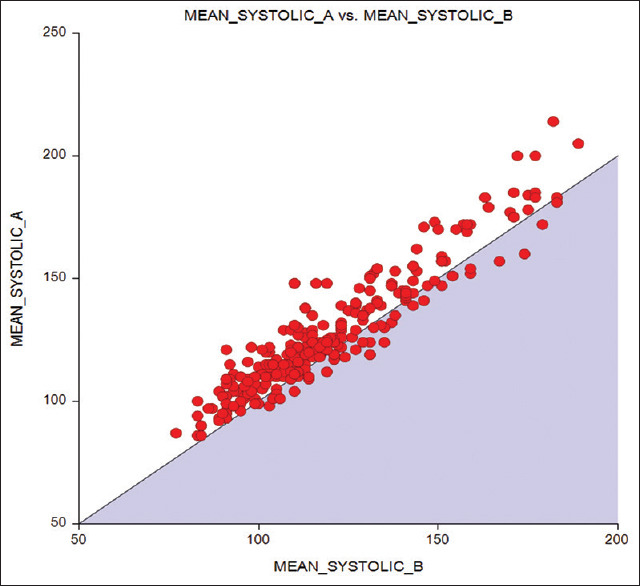
Linear regression curve of systolic blood pressure
Figure 2.
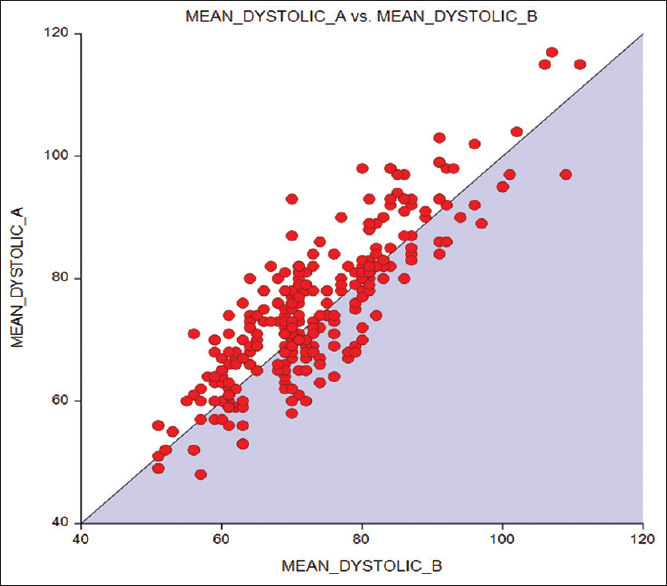
Linear regression analysis of diastolic blood pressure
Table 3.
Comparison of patients based on the BP categorization by two different instruments
| Automated BP device | Mercury-free LED BP Device | Validity measures | |||
|---|---|---|---|---|---|
| Hypertensive | Non Hypertensive | Total | |||
| Hypertensive | 57 | 19 | 76 | Sensitivity=96.61%. Specificity=92.21%, PPV=75%, NPV=99%, Accuracy=93%, Kappa statistics=0.80 |
|
| Nonhypertensive | 2 | 222 | 224 | ||
| Total | 59 | 241 | 300 | ||
Table 4.
Characteristics of the ROC curve
| Systolic blood pressure | Sensitivity (%) | Specificity (%) | ROC characteristics |
|---|---|---|---|
| JNC VII (≥140 mmHg) | 98.1 | 92 | Area under ROC=0.984 |
| ROC curve cut of value at 139 mmHg | 100 | 91 | SE=0.005 |
| P<0.0001 | |||
| 95% CI = (0.973, 0.994) | |||
| Diastolic blood pressure | |||
| JNC VII (≥90 mmHg) | 82.6 | 93 | Area under ROC=0.97 |
| ROC curve cut of value at 86 mmHg | 95.7 | 90 | SE=0.01 |
| P=<0.0001 | |||
| 95% CI = (0.950, 0.989) | |||
Figure 3.
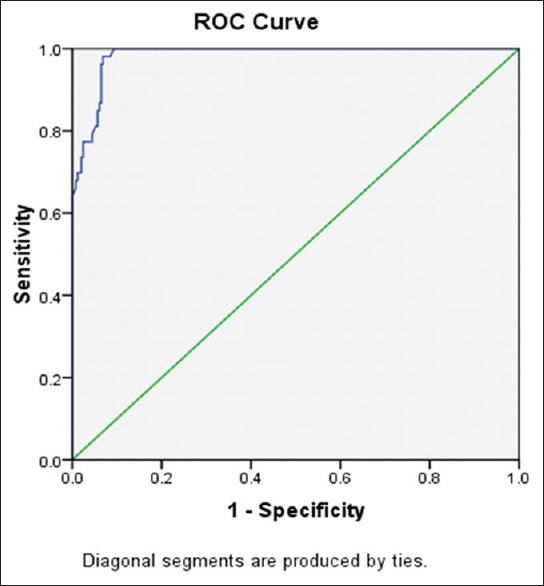
ROC curve of systolic blood pressure
Figure 4.
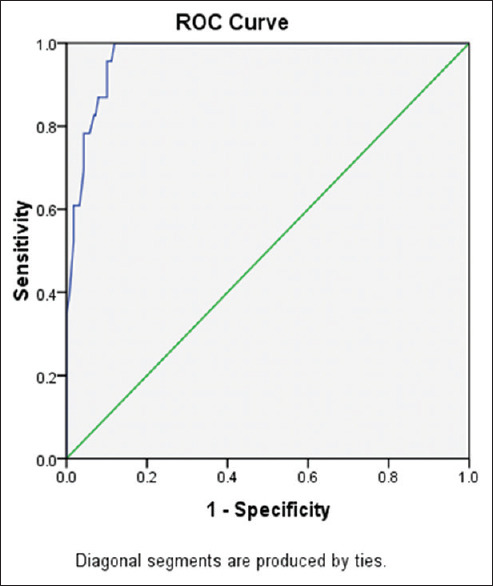
ROC curve of diastolic blood pressure
Discussion
BP devices are important entities in clinical and nursing practice in the management of hypertension. Several types of BP devices are available in the market depending on the need of the users. To minimize the observer bias and influence of observer-subject interaction on the measurement of BP in clinical settings, the automated BP devices were designed and were made available.[9] The role of the observer in recording the BP is made minimal and substituted with a clinically endorsed, handy, digital instrument thus eliminating inaccuracy due to factors such as digit preference, too quick deflation of the cuff, or misreading up or down to influence the patient's BP status. The benefits of taking readings using an automated device are generally applicable to population surveys.
This study was conducted to validate the accuracy of non-mercury digital or automated instruments and their ability to correctly diagnose hypertension. A digital instrument was selected for the purpose and was judged with respect to a properly calibrated non-mercury BP device. The mean BP with the automated device was 125.92 ± 23.47/74.45 ± 12.20 mmHg compared to 118.28 ± 22.90/72.62 ± 11.13 mmHg for the manual BP and the mean difference is statistically insignificant with P values for systolic and diastolic BP is 0.36 and 0.056, respectively. The CCC for systolic is 0.89 (95% CI 0.86–0.91) which near to moderate concordance and for diastolic, it is 0.85 (95% CI 0.82–0.88) which is not a fair concordance. CCC provides a range in defining agreement and different researchers have interpreted it differently. Altman interpreted like other correlation coefficients like Pearson's with < 0.20 as poor and >0.80 as excellent and McBride suggested >0.90 as good concordances.[20,21] Every statistician does agree that ±1 is perfect concordance or discordance and 0 is no correlation and with everything in between should be interpreted with caution. This further suggested that there is a question over the overall accuracy of digital instruments in measuring diastolic BP (CCC-0.85, not fair concordance according to Mc Bride) in primary care setting which is in concordance with the study done in West Bengal where aneroid BP device has better sensitivity and specificity in compared to digital device.[10] A study was done by Nelson also demonstrated that there is inaccuracy in the use of automated BP monitors and traditional aneroid manometers in comparison to the gold standard mercury column manometer.[22] However, Cohen's kappa statistic for diagnosing hypertension of digital devices as compared to the mercury-free LED BP device was found to be 0.80 which is a fair degree of agreement according to the JNC VII and VIII criteria.
The implementation of digital devices has decreased the end-digit and threshold biases in the clinical setting which cannot be ruled out even in this study where the manual BP machine user tends to report the BP with the preference of the zero end digit as found in other studies.[23,24] End digit bias is universally found in settings where manual BP machine is used which may result in faulty BP measurements leading to either depriving hypertensive patients of the benefits of treatment or exposing normotensive patients to unnecessary side-effects of antihypertensive medications.[24,25,26]
The quality and accuracy of automated office BP in relation to the awake ambulatory BP have been found out to be significantly better compared to manual office BP.[27] There are studies that also say that white coat hypertension may be eliminated with the automated office BP readings.[11,28] Although in our study the mean BP is more with the automated BP device compared to manual BP machine, this may be explained considering the fact that the initial readings were taken with the automated device by an observer and then the mercury-free LED BP device was used to take the readings in the study. The time elapsed during the initial readings may have reduced the anxiety and BP lowered during the recording by the manual device. Moreover, the observer with the manual machine was a community physician and people were acquainted with him which may have eliminated the effect of the white coat. This also highlights the fact that the white coat response may be lowered when a known clinician records the BP. Studies on white coat hypertension reported about 25% of the hypertensive population had a clinically increase in BP when readings were taken in the treatment setting, especially by clinicians. Even the automated devices provoke a similar response and readings are similar to manual office BP when a clinician observes the readings.[29,30,31] Studies have clearly shown that the increase in BP associated with conventional manual office measurement can be eliminated if the three basic tenets of automated office BP are followed; the patient rests alone in a quiet room and multiple readings are taken with a fully automated device and no observer in the room.[22,28] In the present study, after multiple readings, BP seems to lower a bit after the initial readings by the first observer which supports the fact that multiple readings may lessen the effect of white coat effect. The improved accuracy is probably achieved by having the patient resting alone and by the use of an automated, validated device to take multiple, standardized readings and with no observer or acquainted observer with whom the patient is comfortable. The study holds paramount importance in the contemporary world as increased BP is one of the leading causes of morbidity and mortality all over the world including India and measuring BP is a routine activity in all clinical settings. Screening and diagnosis of hypertension is a major component of primary care and family physicians are contributing to it vehemently. Their efforts must not go in vain due to simple confusion in the selection and usage of different sphygmomanometers available at present. Through this study, measurement of BP will have more grounds of evidence and open new avenues of research for the future.
The major limitation of the study was that it was conducted within the OPD settings, which itself carried the chances of bias as studying individuals were only from OPD patients who sought health services only. Moreover, we used a single instrument of each type and therefore it is impossible to comment on all types of digital instruments and generalize the findings when there are multiple brands of these instruments available in the market. In this study, only two instruments were compared but studies may be contemplated with different instruments for more evidence in the future. The novelty of this research is that CCC has been used to measure agreement between two continuous variables for a long time but this has never been used to compare the BP in Indian settings using different BP measuring instruments.
Conclusion
This study concluded that the overall automated BP machine has a fair degree of agreement with a mercury-free LED BP device. The statistical tests also proved its validity to diagnose hypertension may also be considerable. The automated BP machine with little training may be used in the field as well as clinical set up by paramedical staff for checking and monitoring BP but with caution. It may be recommended that the digital instruments which need not much technical expertise in measuring BP may be made available at strategic locations for its usage as per the need. But it should be kept in mind that this instrument must be calibrated at regular intervals to avoid any error or biases by observing all the precautions.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
My sincere gratitude to the research participants for their co-operation in the study.
References
- 1.Pavlik VN, Hyman DJ, Toronjo C. Comparison of automated and mercury column blood pressure measurements in health care settings. J Clin Hypertens (Greenwich) 2000;2:81–6. [PubMed] [Google Scholar]
- 2.van Popele NM, Bos WJ, de Beer NA, vanDer Kuip DA, Hofman A, Grobbee DE, et al. Arterial stiffness as underlying mechanism of disagreement between an oscillometric BP monitor and a blood pressure device. Hypertension. 2000;36:484–8. doi: 10.1161/01.hyp.36.4.484. [DOI] [PubMed] [Google Scholar]
- 3.Smith S. An audit of nursing observations on ward patients. Nurs Times. 2008;104:28–9. [Google Scholar]
- 4.Watson D. The impact of accurate patient assessment on quality of care. Nurs Times. 2006;102:32–7. [PubMed] [Google Scholar]
- 5.Ogedegbe G, Pickering T. Principles and techniques of blood pressure measurement. Cardiol Clin. 2010;28:571–86. doi: 10.1016/j.ccl.2010.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carrasco JL, Jover L, King TS, Chinchilli VM. Comparison of concordance correlation coefficient estimating approaches with skewed data. J Biopharm Stat. 2007;17:673–84. doi: 10.1080/10543400701329463. [DOI] [PubMed] [Google Scholar]
- 7.European Union. Directive 2007/51/EC of the European Parliament and of the Council of 25 September 2007 amending Council Directive 76/769/EEC relating to restrictions on the marketing of certain measuring devices containing mercury Strasbourg. 2007. [Last accessed on 2019 Sep 12]. Available from: http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX:32007L0051 .
- 8.Shahbabu B, Dasgupta A, Sarkar K, Sahoo SK. Which is more accurate in measuring the blood pressure?A digital or an aneroid blood pressure device. J Clin Diagn Res. 2016;10:LC11–4. doi: 10.7860/JCDR/2016/14351.7458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.King TS, Chinchilli VM, Carrasco JL. A repeated measures concordance correlation coefficient. Stat Med. 2007;26:3095–113. doi: 10.1002/sim.2778. [DOI] [PubMed] [Google Scholar]
- 10.Fagard RH, Van Den Broeke C, De Cort P. Prognostic significance of blood pressure measured in the office, at home and during ambulatory monitoring in older patients in general practice. J Hum Hypertens. 2005;19:801–7. doi: 10.1038/sj.jhh.1001903. [DOI] [PubMed] [Google Scholar]
- 11.Myers MG, Godwin M. Automated measurement of blood pressure in routine clinical practice. J Clin Hypertens. 2007;9:267–70. doi: 10.1111/j.1524-6175.2007.06512.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ma Y, Temprosa M, Fowler S, Prineas RJ, Montez MG, Friday JB, et al. Evaluating the accuracy of an aneroid sphygmomanometer in a clinical trial setting. Am J Hypertens. 2009;22:263–6. doi: 10.1038/ajh.2008.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–68. [PubMed] [Google Scholar]
- 14.Westgard JO, Hunt MR. The American Association of Clinical Chemists, Inc; 1973. Use and Interpretation of Common Statistical Tests in Method-Comparison Studies. [PubMed] [Google Scholar]
- 15.Agrawal VK, Bhalwar R, Basannar DR. Prevalence and determinants of hypertension in a rural community. Med J Armed Forces India. 2008;64:21–5. doi: 10.1016/S0377-1237(08)80139-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Community prevention and control of cardiovascular diseases. WHO Tech Rep Ser. 1986;732:1–62. [PubMed] [Google Scholar]
- 17.Muntner P, Shimbo D, Carey RM, Charleston JB, Gaillard T, Misra S, et al. on behalf of the American Heart Association Council on Hypertension;Council on Cardiovascular Disease in the Young;Council on Cardiovascular and Stroke Nursing;Council on Cardiovascular Radiology and Intervention;Council on Clinical Cardiology;and Council on Quality of Care and Outcomes Research. Measurement of blood pressure in humans:A scientific statement from the American Heart Association. Hypertension. 2019;73:e35–66. doi: 10.1161/HYP.0000000000000087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Whelton PK, Carey RM, Aronow WS, Casey DE, Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults:A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Hypertension. 2018;:e140-4] Hypertension. 2018;71:e13–115. [Google Scholar]
- 19.Hernandez-Vila E. A review of the JNC 8 Blood Pressure Guideline. Tex Heart Inst J. 2015;42:226–8. doi: 10.14503/THIJ-15-5067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Altman DG. Practical Statistics for Medical Research. London: Chapman and Hall; 1991. [Google Scholar]
- 21.McBride GB. Using Statistical Methods for Water Quality Management:Issues, Problems and Solutions. New York: Wiley; 2005. [Google Scholar]
- 22.Nelson D, Kennedy B, Regnerus C, Schweinle A. Accuracy of automated blood pressure monitors. J Dent Hyg. 2008;82:35. [PubMed] [Google Scholar]
- 23.Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients'resting blood pressure in clinical settings:A systematic review. J Hypertens. 2017;35:421–41. doi: 10.1097/HJH.0000000000001197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thavarajah S, White WB, Mansoor GA. Terminal digit bias in a specialty hypertension faculty practice. J Hum Hypertens. 2003;17:819–22. doi: 10.1038/sj.jhh.1001625. [DOI] [PubMed] [Google Scholar]
- 25.Graves JW, Bailey KR, Grossardt BR, Gullerud RE, Meverden RA, Grill DE, et al. The impact of observer and patient factors on the occurrence of digit preference for zero in blood pressure measurement in a hypertension specialty clinic:Evidence for the need of continued observation. Am J Hypertens. 2006;19:567–72. doi: 10.1016/j.amjhyper.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 26.Nargesi AA, Ghazizadeh Z, Larry M, Morteza A, Heidari F, Asgarani F, et al. Manual or automated blood pressure device?A historical cohort to quantify measurement bias in blood pressure recording. J Clin Hypertens (Greenwich) 2014;16:716–21. doi: 10.1111/jch.12400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, Grant FC, et al. Conventional versus automated measurement of blood pressure in primary care patients with systolic hypertension:Randomized parallel design controlled trial. BMJ. 2011;342:d286. doi: 10.1136/bmj.d286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nelson M. Automated blood pressure readings in primary care demonstrate better correlation to the gold standard of ambulatory monitoring than manual assessment. Evid Based Med. 2011;16:172–3. doi: 10.1136/ebm1414. [DOI] [PubMed] [Google Scholar]
- 29.Myers MG. Automated blood pressure measurement in routine clinical practice. Blood Press Monit. 2006;11:59–62. doi: 10.1097/01.mbp.0000200481.64787.c0. [DOI] [PubMed] [Google Scholar]
- 30.Myers MG, Godwin M, Dawes M, Kiss A, Tobe S, Kaczorowski J. Measurement of blood pressure in the office—recognizing the problem and proposing the solution. Hypertension. 2010;55:195–200. doi: 10.1161/HYPERTENSIONAHA.109.141879. [DOI] [PubMed] [Google Scholar]
- 31.Pickering TG, James GD, Boddie C, Harshfield GA, Blank S, Laragh JH. How common is white coat hypertension? JAMA. 1988;259:225–8. [PubMed] [Google Scholar]


