Abstract
Context:
Identification and documentation of risk factors for non-communicable diseases (NCDs) among an 'invisible community' like the transgenders (TGs) will throw light on the prevailing health status of one of the most marginalized populations in India, thereby paving way for initiating measures that would cater to their healthcare needs.
Aims:
To estimate prevalence of risk factors for NCDs among TGs registered in a community-based organization in Puducherry.
Settings and Design:
A cross-sectional descriptive study among adult (≥18 years) TGs in a community-based organization in Puducherry.
Methods and Material:
Data on sociodemographic details, selected risk factors of NCDs—alcohol use, tobacco use, physical inactivity, obesity, unhealthy diet, hypertension, and self-reported diabetes mellitus (DM) were collected using a pre-tested structured questionnaire. Dependence levels on tobacco and/or alcohol were obtained using “Fagerstrom Addiction Scale” and “Alcohol Use Disorder Identification Test” scales, respectively.
Statistical Analysis Used:
Data were single entered using EpiData and analyzed using EpiData Analysis.
Results:
Of the 200 TGs included in the study, mean (SD) age was 30 (8.8) years. Around 47% belonged to upper-lower socioeconomic class. About 90% of the participants had unhealthy dietary practice, 84% were physically inactive, 41% had high waist hip ratio, 36% were obese, 16% had high blood pressure, and 8% had self-reported DM. Prevalence of tobacco use was 43.5% with high nicotine dependence noted in 29% (23/79) of smokeless tobacco users and 12% (2/17) of smokers. Alcohol use was reported among 64.5% of which one fifth had possible dependence.
Conclusion:
Prevalence of selected risk factors for NCDs was high among TGs when compared to general population in Puducherry, which warrants targeted health interventions and priority in policy planning.
Keywords: Transgenders, non communicable disease, risk factors, tobacco dependence, alcohol dependence
Introduction
Non-communicable diseases (NCDs) mainly comprise of cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes.[1] These four groups of diseases account for 71% of all deaths globally and 80% of all premature NCD deaths. They disproportionately affect masses in low and middle-income countries where more than three quarters of global NCD deaths occur (32 million).[2] In India, NCDs account for 63% of all deaths.[3]
According to World Health Organization (WHO) tobacco use, harmful use of alcohol, unhealthy diet, and physical inactivity are the major behavioral risk factors responsible for the same. The major metabolic risk factors for NCDs include obesity, raised blood pressure, and raised blood glucose.[1] There are studies assessing the risk factors for NCDs among the general population in India, but these risk factors are lesser explored among certain minority groups, transgenders (TGs) being one of them.
TG is an umbrella term referring to “people whose gender identity and expression does not conform to the norms and expectations traditionally associated with the sex assigned to them at birth.”[4] Studies show TGs are exposed to behavioral risk factors for NCDs like smoking, alcoholism[5,6] due to the stress that culminate from their daily battles with stigma, discrimination, and social exclusion.[7,8,9] WHO states that the challenges faced by the TG population are to be mitigated by addressing the social determinants of health[10] and improving the responsiveness of health systems.[8,11,12] Assessment of chronic disease morbidity in this group is essential for inclusion in the primary healthcare system. Hence the study was aimed to determine the risk factor levels for NCDs among this vulnerable section of the community.
Subjects and Methods
This cross-sectional descriptive study was conducted from August to September, 2016 among TGs (aged 18 years and above) registered with Sahodaran Community Oriented Health Development Society (SCOHD) in Puducherry, South India. SCOHD is a registered, government of Tamil Nadu and Puducherry recognized non-profit state level community-based organization (CBO) for people with different sexuality. It is a part of the Targeted Intervention project aided by State AIDS Control Society (SACS). Around 280 TGs are registered with the CBO.
Assuming at least 50% of TGs as having at least one behavioral risk factor for NCDs, with 8% absolute precision and alpha error of 5%, the sample size was calculated as 151 (using OpenEpi version 3.01). However, all the eligible TGs registered with the CBO were approached and data was collected from 200 subjects.
Participants were interviewed using a structured questionnaire. Sociodemographic details like occupation, education, family status were collected. Socioeconomic status was assessed using the Kuppuswamy socioeconomic scale 2015. Physical inactivity and diet were assessed based on the nature and duration of physical activity, the number of servings of fruits and vegetables consumed in a day, and on the indulgence in junk foods like salty and/or sugary food items and drinks, etc. Information on existing medical conditions like diabetes and hypertension among the participants were collected.
Current tobacco and alcohol users were defined as having consumed tobacco or alcohol within past 1 month. Possible nicotine dependence among current users was assessed using the pre-tested and validated Fagerstrom Addiction Scale for Smokers and the Modified Fagerstrom Questionnaire for Smokeless Tobacco Users. AUDIT scale (Alcohol Use Identification Test) was used to assess the dependence level for alcohol among current users.
Details of hormonal treatment, illicit drug use (self-reported), and HIV status (self-reported) were also collected. Physical parameters like height, weight, waist, and hip circumferences were measured following standard STEPS guidelines.[13] Body mass index (BMI) was calculated based on the weight and height of the subject. Waist circumference and hip circumference of each participant were measured using a stretch-resistant tape and waist hip ratio (WHR) was obtained.[14] Blood pressure was measured using electronic sphygmomanometer (Omron HEM 7130) in right upper limb in sitting posture with arm at the level of heart. Two readings at least 10 min apart were taken and an average of both served as the final reading. The questionnaire after translating to the local language (Tamil) was translated back into English to ensure its reliability and validity. A pilot test was conducted before initiation of the study, to look for the feasibility of administration of questionnaire.
This study was approved by the Institute Ethics committee and permission was obtained from the organization. Daily visits were made to the CBO for data collection for a period of 2 months and members who could not be contacted at the organization were contacted in the community. Eligible subjects were included in the study after obtaining written informed consent. Maintenance of privacy and confidentiality was ensured.
Data were single entered using EpiData and analyzed using EpiData Analysis. Continuous variables like age, BMI, WHR, blood pressure were expressed using mean (SD). Categorical variables were expressed in proportions.
Results
A total of 200 TGs in the age group of 18 years and above were included in the study with a response rate of 100%. Out of the 200 participants, majority were male to female (MTF) TGs (only two were female to male TGs). Sociodemographic characteristics are detailed in Table 1. About 42% of participants were in the age group of 25–34 years. Around 33.5% received college education and one-third was educated up to higher secondary. Over 46.5% of participants belong to the upper-lower class of socioeconomic status. More than half (57.5%) of them were not living with their biological families.
Table 1.
Sociodemographic characteristics of transgenders (aged >=18) belonging to a community based organization in Puducherry (n=200)
| Characteristics | Frequency (n) | Percentage (%) | |
|---|---|---|---|
| Age | 18-24 years | 61 | 30.5 |
| 25-34 years | 84 | 42 | |
| >=35 years | 55 | 27.5 | |
| Educational Status | Illiterate | 13 | 6.5 |
| Up to 8th grade | 55 | 27.5 | |
| 9th-12th grade | 65 | 32.5 | |
| Any college education | 67 | 33.5 | |
| Occupation Categories | Unemployed | 11 | 5.5 |
| Begging | 71 | 35.5 | |
| Sex work | 16 | 8 | |
| Both begging & sex work | 29 | 14.5 | |
| Salaried | 40 | 20 | |
| Other jobs | 33 | 16.5 | |
| Socio-economic status* | Upper middle | 31 | 15.5 |
| Lower middle | 72 | 36 | |
| Upper lower | 93 | 46.5 | |
| Lower | 4 | 2 | |
* Modified Kuppuswamy scale 2015
Majority (90.5%) consumed less than five servings of fruits and vegetables in a day and 74% consumed junk food. About 84% of the study population were found to be physically inactive [Table 2]. Table 3 shows the prevalence of metabolic risk factors. About 8% reported to be diabetic; 34.5% were unaware of their blood sugar status. Less than 10% (6.5%) of the population had self-reported hypertension. Around 16% were hypertensive on recording. Mean (SD) systolic blood pressure in the population was around 123.8 (17.3) mmHg and mean (SD) diastolic blood pressure was 75.6 (11.5) mmHg. Prevalence of obesity according to BMI in this study group was 34.5%, while 16% were overweight. The mean (SD) waist circumference was 83.5 (12.4). Abdominal obesity was seen in 35% of the TGs. WHR was above the cutoff (0.9) in 41% of the study participants. Around 15% of the participants reported current hormone pill use, 2.5% reported being HIV positive, and only 1% reported illicit drug use.
Table 2.
Behavioural risk factors for non-communicable diseases among the study participants (n=200)
| Behavioural Risk | Factors | Frequency (n) n=200 | Percentage (%) |
|---|---|---|---|
| Physical inactivity* | Present | 168 | 84 |
| Absent | 32 | 16 | |
| Intake of Fruits & vegetables | >=5 servings of fruits& vegetables a day | 19 | 9.5 |
| <5 servings of fruits & vegetables a day | 181 | 90.5 | |
| Consumption of junk food | Daily | 68 | 34 |
| Once or more in a week | 70 | 35 | |
| Occasionally or rarely | 10 | 5 | |
| Do not consume | 52 | 26 | |
| Tobacco use | Current users | 87 | 43.5 |
| Past users | 19 | 9.5 | |
| Never users | 94 | 47 | |
| Alcohol use | Current users | 129 | 64.5 |
| Past users | 14 | 7 | |
| Never users | 57 | 28.5 |
*Less than 150 minutes of moderate physical activity
Table 3.
Select metabolic and physiological risk factor profile for non-communicable diseases among the study participants (n=200)
| Metabolic & Physiological | Risk Factors | Frequency (n) n=200 | Percentage (%) |
|---|---|---|---|
| Diabetes (Self-reported) | Yes | 16 | 8 |
| No | 115 | 57.5 | |
| Don’t know | 69 | 34.5 | |
| Hypertension (Self-reported) | Yes | 13 | 6.5 |
| No | 125 | 62.5 | |
| Don’t know | 62 | 31 | |
| Hypertension (Recorded during data collection) | Yes | 32 | 16 |
| No | 168 | 84 | |
| Body mass index | Underweight (<18.5 kg/m2) | 33 | 16.5 |
| Normal (18.5-24.99 kg/m2) | 66 | 33 | |
| Overweight (25-30 kg/m2) | 32 | 16 | |
| Obese (>30 kg/m2) | 69 | 34.5 | |
| Waist circumference | <=90 cm | 130 | 65 |
| >90 cm | 70 | 35 | |
| Waist-Hip ratio | <=0.9 | 118 | 59 |
| >0.9 | 82 | 41 |
About 43.5% of the participants were currently using tobacco out of which 80.5% were exclusive smokeless tobacco users, 9.1% exclusive smokers, and 10.3% used both forms. Among 17 participants who were current smokers, the mean (SD) age of initiation of smoking was 23 (5.6) years and 11.7% showed high dependence on nicotine. Among the 79 current users of smokeless tobacco, mean (SD) age of initiation of smokeless tobacco was 22.8 (7.8) years and 29.1% had high dependence on nicotine [Table 4]. Current users of alcohol were 64.5% (n = 129) and the mean (SD) age of initiation of alcohol was 22.2 (6.3) years. About 45% had hazardous use, 21% showed harmful use, and 19.3% had possible dependence as per the AUDIT scale [Figure 1].
Table 4.
Nicotine dependence among current tobacco users in the study
| Nicotine dependence among smokers † (n=17) | Frequency (n) | Percentage (%) |
|---|---|---|
| Low Dependence (0-2) | 11 | 64.7 |
| Medium Dependence (3-5) | 4 | 23.5 |
| High Dependence (>=6) | 2 | 11.7 |
| Nicotine dependence among smokeless tobacco users‡ (n=79) | ||
| Low Dependence (0-4) | 20 | 25.3 |
| Medium Dependence (5-8) | 36 | 45.5 |
| High Dependence (>=9) | 23 | 29.1 |
†Fagerstrom Addiction Scale for Smokers. ‡Modified Fagerstrom Questionnaire for smokeless tobacco users
Figure 1.
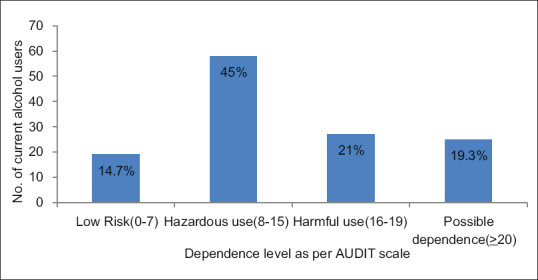
Dependence among the current alcohol users in study participants as per AUDIT Scale (n = 129)
Discussion
Few studies have been conducted in the past, to assess the risk factors for NCDs among TGs in India. Physical inactivity levels of the TG participants in this study are alarmingly higher (84%) in comparison to studies conducted on general adult population by Rajalakshmi M et al. in Tamil Nadu[15] and Chauhan RC et al. in Puducherry[16] (50.75% and 51.5%, respectively). This is also greater when compared to 66% in the general population in Tamil Nadu as per the NCD risk factor survey done under Integrated Disease Surveillance Project (IDSP).[17] But this is similar to that found in a TG study in Coimbatore (83%).[18] This could be because of lack of awareness and/or unavailability of safe space for doing physical activity without inhibition. The present study found 90.5% of the study participants had less than five servings of fruits and vegetables per day which is almost similar to general adult population (99%)[17] and slightly higher than the study conducted by Chauhan RC et al. (86.5%).[16]
The prevalence of self-reported diabetes (8%) is greater when compared to the study conducted among TGs (3%) by Sivakami et al. in Coimbatore[18] and by Vaithyanathan et al. among general population in Puducherry (5.7%).[19] This is similar though, in comparison to the general population in India (7.7%).[20] But 34.5% of the TGs have not been screened for diabetes, and their blood sugar levels are unknown which is disconcerting. The high prevalence of raised blood pressure observed in this study is almost similar to that observed by Sivakami et al. (15%).[18] However, only 6.5% of the TGs in this study self-reported to be hypertensive, which indicates an urgent need for awareness regarding blood pressure screening among them.
The proportions of overweight and obese participants in this study are higher in comparison to the transgender participants of the same study (20% and 12%, respectively).[18] Literature shows much lower obesity among general population (19.2%) when compared to the TGs in this study, but it also shows slightly higher overweight prevalence.[16] This study reveals high prevalence of abdominal obesity among the TGs in comparison to the general population in Tamil Nadu (25%).[17] A study conducted among fishermen in a selected district of Tamil Nadu indicates lower prevalence of abdominal obesity (13.3%) in comparison to the participants of this study.[21] The proportion of WHR above cutoff is higher in the present study when compared to the Sivakami et al. study (10%).[18]
Our study findings are on par with the prevalence of tobacco usage among TGs in Coimbatore (50%).[18] But it is higher when compared with males from the general population in Puducherry (13.4% and 14.4%).[16,22]
High-nicotine dependence (11.7%) was found among TG smokers in this study, which is greater than the proportion of high dependence smokers among industrial workers in Mangalore (9.7%).[23] Medium dependence for nicotine was also higher among TG smokers in comparison to the same study (2.23%). The current TG study shows a bigger prevalence of exclusive smokeless tobacco use; and high-dependence on smokeless tobacco (29.1%) exceeds that seen among smokers. This is also greater in comparison to the high-dependence levels observed in other studies done on general population (17% and 20%).[24,25] This could be because of lack of taxation on smokeless forms and easier availability at much lower costs.
Prevalence of alcohol usage in this study was higher than that observed in the Coimbatore TG study (25%)[18] but similar to that found by Shunmugam et al. on TGs in Maharashtra and Tamil Nadu (70%).[26] However, in comparison to the alcohol consumption among general male, and all adult population in Puducherry (27.5% and 9.3% respectively),[16,27] this study exposes alarming prevalence. This study discovered greater (45%) hazardous risk of alcohol dependence. A study conducted by Vaithyanathan et al., among general population of Puducherry displays lower proportion of possible dependence (13.1%),[28] than that found in our study (19.3%). Ramanan et al. found high-risk for dependence (29.3%) among drinkers, which corresponds to harmful and possible dependence in our study (40.3%).[29] This is also disturbingly higher among the transgender population.
The prevalence of NCD risk factors among TGs in this study are high and the pattern of risk factors are found to be higher among them than that in the general population. Certain risk factors like physical inactivity, abdominal obesity, tobacco–alcohol usage, and dependence on them are higher. This emphasizes the necessity of awareness programmes covering these aspects, which could be done on specified days like diabetes day, hypertension day, world-no-tobacco day, etc. Sensitizing PHCs (Primary Health Centres) for regular surveys like testing blood pressure, blood sugar etc. On HIV testing days would enable early detection of lurking risk factors for NCDs at the primary healthcare level itself.
Additional measures in terms of planning health services, outreach activities, referral and counselling need to be targeted in this group. Dependence on tobacco and alcohol can be managed by holding brief counselling sessions with simple advice, and by warranting further diagnostic evaluation and appropriate treatment for dependence. Around 15% of the participants reported current hormone pill use, 2.5% reported being HIV positive, and 1% reported illicit drug use in this study. These factors could be potential risk factors for NCDs, the association of which needs to be systematically studied.
There were several strengths and limitations in this study. Sample size could be covered with full response rate because of the cooperation from the participants at the CBO, as they were interested in knowing the risk profile for NCDs in their community. Also many of the members of the CBO could be contacted and interviewed from their residences. There could be possible social desirability bias regarding reporting of behavioral risk factors. Only self- reported diabetes was recorded and fasting blood sugar levels were not checked among the study participants.
Conclusion
The perspectives and needs of TG people should be routinely considered in public health efforts to eliminate health inequalities. Another key issue is access to health services for vulnerable genders. The fear of stigma inhibits them from utilizing even basic healthcare needs, and therefore a more receptive attitude from the entire healthcare system is quintessential for improving the health status of this community. The spirit of inclusivity as promulgated through Universal Health Coverage will help ameliorate the health status of each such individual.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to extend their warm gratitude to Dr. Sheethal K Nayak, President cum Project director of SCOHD (Sahodaran Community Oriented Health Development Society), Puducherry, for her total support and participation in this study.
References
- 1.WHO |Non-communicable diseases country profiles 2018 [Internet] WHO; [cited 2019 Nov 13]. Available from: http://www.who.int/nmh/publications/ncd-profiles-2018/en/ [Google Scholar]
- 2.WHO |Non-communicable diseases [Internet] [cited 2019 Nov 13]. Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases .
- 3.WHO |Noncommunicable diseases country profiles 2018 [Internet] WHO; [cited 2019 Nov 13]. Available from: http://www.who.int/nmh/countries/en/ [Google Scholar]
- 4.WHO_HIV_2015.17_eng.pdf [Internet] [cited 2019 Nov 13]. Available from: https://apps.who.int/iris/bitstream/handle/10665/179517/WHO_HIV_2015.17_eng.pdf .
- 5.Virupaksha HG, Muralidhar D. Resilience among transgender persons:Indian perspective. Indian J Soc Psychiatry. 2018;34:111–5. [Google Scholar]
- 6.Watson RJ, Veale JF, Gordon AR, Clark BA, Saewyc EM. Risk and protective factors for transgender youths'substance use. Prev Med Rep. 2019;15:100905. doi: 10.1016/j.pmedr.2019.100905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chattu VK, Laplume MO, Kumary S. Time for the two-spirits:Shaping the inclusive policy environment for hispanics and transgenders through global health diplomacy. J Fam Med Prim Care. 2017;6:716–20. doi: 10.4103/jfmpc.jfmpc_74_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reisner SL, Poteat T, Keatley J, Cabral M, Mothopeng T, Dunham E, et al. Global health burden and needs of transgender populations:A review. Lancet. 2016;388:412–36. doi: 10.1016/S0140-6736(16)00684-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Namer Y, Razum O. Subgroup-specific services or universal health coverage in LGBTQ+health care. Lancet Public Health. 2019;4:e278. doi: 10.1016/S2468-2667(19)30080-5. [DOI] [PubMed] [Google Scholar]
- 10.Martinez-Velez JJ, Melin K, Rodriguez-Diaz CE. A preliminary assessment of selected social determinants of health in a sample of transgender and gender nonconforming individuals in Puerto Rico. Transgender Health. 2019;4:9–17. doi: 10.1089/trgh.2018.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organisation. Primary Health Care on the Road to Universal Health Coverage. [cited 2019 Dec 20]. uhc_report_2019.pdf [Internet] Available from: https://www.who.int/healthinfo/universal_health_coverage/report/uhc_report_2019.pdf .
- 12.World Health Organisation. Executive board provisional agenda B133_1_annotated-en.pdf [Internet] [cited 2019 Nov 13]. Available from: http://apps.who.int/gb/ebwha/pdf_files/EB133/B133_1_annotated-en.pdf .
- 13.World Health Organisation.steps_framework_dec03.pdf [Internet] [cited 2019 Nov 18]. Available from: https://www.who.int/ncd_surveillance/en/steps_framework_dec03.pdf .
- 14.World Health Organization. Waist Circumference and Waist-Hip Ratio:Report of a WHO Expert Consultation, Geneva, 8-11 December 2008. Geneva: World Health Organization; 2011. [Google Scholar]
- 15.Rajalakshmi M, Dongre AR. Risk factors for non-communicable diseases in villages of Tamil Nadu-A survey. Int J Med Sci Public Health. 2019;8:312–8. [Google Scholar]
- 16.Chauhan RC, Purty AJ, Natesan M, Velavan A, Singh Z. Risk factors profile for noncommunicable diseases among adult urban population of puducherry in India. J Obes Metab Res. 2014;1:201–8. [Google Scholar]
- 17.IDSP Non-communicable disease risk factor survey.Tamil_Nadu.pdf [Internet] [cited 2019 Nov 13]. Available from: https://www.icmr.nic.in/sites/default/files/reports/Tamil_Nadu.pdf .
- 18.Sridevi Sivakami PL, Veena KV. Social exclusion have a negative impact on the health of the Transgender. Indian Streams Res J. 2011;1:1–4. [Google Scholar]
- 19.Purushothaman V, Thekkur P, Boovaragasamy C, Suguna A, Anbazhagan S, Seetharaman N. Concomitant behavioral risk factors of non-communicable diseases and its associated factors among adults in the selected rural areas of Puducherry, South India:A community based cross-sectional study. Natl J Res Community Med. 2017;6:149–54. [Google Scholar]
- 20.Tandon N, Anjana RM, Mohan V, Kaur T, Afshin A, Ong K, et al. The increasing burden of diabetes and variations among the states of India:The global burden of disease study 1990-2016. Lancet Glob Health. 2018;6:e1352–62. doi: 10.1016/S2214-109X(18)30387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Annadurai K, Balan N, Ranaganathan K. Non-communicable disease risk factor profile among Fishermen community of Kancheepuram district, Tamil Nadu:A cross sectional study. Int J Community Med Public Health. 2018;5:708–13. [Google Scholar]
- 22.National Family Health Survey-4_State FactSheet Puducherry.pdf [Internet] [cited 2019 Nov 16]. Available from: http://rchiips.org/nfhs/pdf/NFHS4/PY_FactSheet.pdf .
- 23.Akram S, Gururaj NA, Nirgude AS, Shetty S. A study on tobacco use and nicotine dependence among plywood industry workers in Mangalore City. J Evol Med Dent Sci. 2015;4:5729–35. [Google Scholar]
- 24.Divinakumar KJ, Patra P, Prakash J, Daniel A. Prevalence and patterns of tobacco use and nicotine dependence among males industrial workers. Ind Psychiatry J. 2017;26:19–23. doi: 10.4103/ipj.ipj_14_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patel PM, Rupani MP, Gajera AN. Dependence on smokeless tobacco and willingness to quit among patients of a tertiary care hospital of Bhavnagar, Western India. Indian J Psychiatry. 2019;61:472–8. doi: 10.4103/psychiatry.IndianJPsychiatry_87_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shunmugam M, Sivasubramanian M, Roy Karmakar S, Samuel M, Chakrapani V. International AIDS Conference. Washington DC, USA: 2012. Extent of alcohol use and its association with inconsistent condom use among hijras/ transgender (male-to-female) people in India: Survey findings from urban and rural sites in Maharashtra and Tamil Nadu. [Google Scholar]
- 27.Vaithyanathan P, Thekkur P, Boovaragasamy C, Suguna A, Surekha A, Seetharaman N. Concomitant behavioral risk factors of non-communicable diseases and its associated factors among adults in the selected rural areas of Puducherry, South India:A community based cross-sectional study. Natl J Res Community Med. 2017;6:149–54. [Google Scholar]
- 28.Vaithiyanathan P, Thekkur P, Kamashvell C, Datta SS. Alcohol use, harmful use of alcohol and probable dependence among residents of a selected fishermen community in South India:A community based cross-sectional analytical study. Int J Community Med Public Health. 2018;5:520–5. [Google Scholar]
- 29.Ramanan VV, Singh SK. A study on alcohol use and its related health and social problems in rural Puducherry, India. J Fam Med Prim Care. 2016;5:804–8. doi: 10.4103/2249-4863.201175. [DOI] [PMC free article] [PubMed] [Google Scholar]


