Abstract
Aim:
We aimed to identify the percutaneous exposure incident (PEI) by private dentists in Mashhad, Iran.
Methods:
Subjects included 199 dentists enrolled in this study. A questionnaire consisting of 11 questions was sent to the dentists for data collection. Information was collected on knowledge about dangers of PEI, a history of needlestick or sharps injuries over the past 12 months, types of devices causing the needlestick or sharps injuries, HBV vaccination, knowledge about PEI protective and therapeutic protocol, and reporting PEI to the specialist. The first ten questions were corrected and each sheet received a score ranging from 0 to 10.
Result:
95 women (47.7%) and 104 men (52.3%) participated in this study aged between 27–72 years old. The findings showed that a total of 132 dentists (66.3%) had experiences with PEI. 45 (22.6%) of them had experiences with PEI in the past year. Files and needles were found to be the most frequent tools causing PEI, each with 29.7% of frequency. 16.6%, 8.6, 5.7, and 9.7% were obtained for dental burs, band, and surgical baled, respectively as other tools responsible for injuries. Results of the question about causes of needlestick injuries showed that personal carelessness is the most frequent reason (53.8%) followed by inappropriate disposal of the needles (7.6%).
Conclusion:
The personal carelessness and inappropriate disposal of needles were reported as the most common reasons for PEI injuries. It is suggested to educational programs for dentists should focus on preventing the PEI.
Keywords: Dental practices, needlestick injuries, sharps injuries
Introduction
Percutaneous exposure incident (PEI) is a term referring to cutaneous and mucosal exposure to the blood and serum by needlestick and other sharp tools. PEI can occur in dental healthcare workers.[1] Because of the presentation of blood and saliva, using sharp instruments such as needle and file, dental practice is a dangerous environment causing blood-borne infections.[2] PEI is one of the most risk factors in the transmission of the human immunodeficiency virus (HIV),[3] hepatitis B virus (HBV), and hepatitis C virus (HCV). It is noteworthy that, HCV causes hepatitis for which there is no vaccine. In 2002, the World Health Organization (WHO) reported that 39% of HCV, 37% of HBV, and 4.4% of HIV cases are caused by PEI. It can make a lot of direct and indirect costs; the mean cost for PEI related to the HIV-infected patients has been reported as 2456 dollars in the USA. The mean cost for PEI has also been reported as 272 euros and 237 dollars in other countries such as Sweden and Korea, respectively.[4,5,6]
Dentists and undergraduate dental students are among the riskiest groups for PEI, caused by the multiple sharp instruments like needles, burs, scalpels, scalers, surgical elevators, explorers, and orthodontic wires.[7] Needlestick is more common than others.[2] It seems that inadequate skill and training about PEI prevention is the reason explaining why dentists and undergraduate dental students are at greater risk.[8] Studies reported various statistics about dentists PEI worldwide as an example, in the United Kingdom about 50% of dentists reported PEI.[7] long work hours and sleep deprivation increase the risk of sharps injury. Most dentists and students do not report needlestick injuries.[5,9]
PEI treatment is expensive and time-consuming. In the present research paper, a study on PEI and its causes was conducted among the private dentists in Mashhad, Iran. The results of this study will lead to control and treatment of PEI.
Methods
Ethical approval was obtained from the Human Ethics Committee, Mashhad University of Medical Science. (ir.mums.dentistry.rec. 1397.083) Date: 26-11-2018.
A cross-sectional questionnaire type study was done. The study population selected by all private dental practitioners in Mashhad City who were listed in the Mashhad Dental Directory. A total of 900 dentists were listed in the Mashhad Directory out of which 199 dentists were selected by stratified cluster sampling.
A multiple-choice 11-question questionnaire including four A4 size-pages was sent to the dentists for data collection. Information on PEI including knowledge about dangers of PEI, ways of prevention and personal opinions about PEI, a history of needlestick or sharps injuries over the past 12 months, types of devices causing the needlestick or sharps injuries, HBV vaccination, knowledge about PEI protective and therapeutic protocol, and reporting PEI to the specialist.
Also, the records and personal information like age, gender, and a number of years working in dental practice were collected for each dentist. The first ten questions were corrected and each sheet received a score ranging from 0–10. The poor range is between 0 and 3 points, the average range is between 4 and 7, and scores between 8 and 10 mean an excellent range. Also, a question about the type of devices causing the PEI gathered a lot of information about the most harmful tools. Although this question did not get a score.
The statistical analysis was conducted using the SPSS software version 19 (V. 19, SPSS Inc., Chicago, IL). Mann-Whitney U and Chi-Square tests were used for data analysis. The P value of less than 0.05 was considered as statistically significant.
Results
About 199 dentists were enrolled in this study, including 95 women (47.7%) and 104 men (52.3%). Their mean age was equal to 40.9 ± 9.6 years old and ranged from 27 to 72 years old. Most of them were general dentists (87.4%) and the rest were specialists (12.6%). Work experience in private office ranged from 1 to 43 years and its means was equal to 11.3 years. All subjects had been vaccinated against hepatitis B. Our results showed that 132 dentists (66.3%) had PEI experiences in the past. It should be noted that some dentists report this incidence more than several times. Among them, 45 (22.6%) of dentists had PEI experience in the past year. Among those experiencing PEI, 99 (49.7%) dentists experienced PEI once, 24 (12.1%) of them experienced PEI twice, 8 (4%) of them experienced it three times, and one (0.5%) dentist experienced PEI four times. After correction of questionnaires, 114 (57.3%) dentists were found to get excellent, 81 (40.7%) of them got average and 4 (2.0%) of them got poor scores [Table 1].
Table 1.
Demographic and based Characteristics of 199 Dentists Survived
| Characteristics | Mean±SD or n (%) |
|---|---|
| Age (years) | 40.91±9.61 |
| Experience (years) | 11.37±7.92 |
| Gender | |
| Female | 95 (47.7) |
| Male | 104 (52.3) |
| Education | |
| General dentist | 174 (87.4) |
| Specialist dentist | 25 (12.6) |
| Scoring Criteria | |
| Poor | 4 (2) |
| Moderate | 81 (40.7) |
| Excellent | 114 (57.3) |
| PEI | |
| 0 | 67 (33.7) |
| 1 | 99 (49.7) |
| 2 | 24 (12.1) |
| 3 | 8 (4) |
| 4 | 1 (0.5) |
Files and needles are the most frequent tools causing PEI, each obtained a frequency of 29.7%, followed by dental burs, band, and surgical baled, respectively obtained a frequency of 16.6%,8.6, and 5.7%. Other injuries with 9.71% of frequency are scaler (4%), endodontic spreader (1.7%), elevators (1.7%), dental probe (1.7%), and arch bar (0.6%), respectively [Figure 1].
Figure 1.
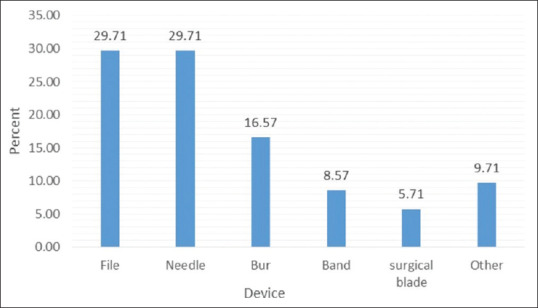
Percentage of various types of devices causing the experienced “sharps” injuries
Among those who experienced PEI, 40 dentists (30.3%) declared that they did report needlestick, and 74 (56.1%) of them declared that did have enough knowledge about protection protocol. Also, amongst the reasons of PEI, 10 cases (7.6%) reported that inappropriate disposal of needles is one of the PEI causes, 71 cases (53.8%) reported personal carelessness as a cause, and 51 cases (38.7%) did not remember the reasons [Table 2].
Table 2.
Characteristics related to Stick needled (n=132)
| n (%) | |
|---|---|
| Causes of PEI | |
| Poor disposal of needle | 10 (7.6) |
| Individual carelessness/accident | 71 (53.8) |
| Cannot remember | 51 (38.7) |
| Report to specialist | |
| Yes | 40 (30.3) |
| No | 92 (69.7) |
| Knowledge of Protocol | |
| Yes | 74 (56.1) |
| No | 58 (43.9) |
Nearly 93.5% of dentists declared that they recapped the syringe. The mean age of those reporting PEI to the specialist is lower than older ones. In other words, PEI reporting in younger dentists is much higher than older ones and this difference was significant (P < 0.001). Also, knowledge about the protocol is higher in young dentists than older dentists, but this difference was not significant. (P = 0.288). As the age increased, scores dropped. The difference between poor and excellent scores was found to be significant. (P = 0.022)
Discussion
Generally, dentistry is considered an occupation at high risk. The disease of patients with blood-borne infections remains mostly hidden due to the fear of patients to dental. For this reason, dentists are advised in most protocols to take all necessary steps to prevent transmission of blood-borne disease. Not reporting PEI can make numerous hazards for the medical system and increases the number of HIV, HBV, and HCV victims. Hepatitis B vaccination is suggested in most international PEI protocol.[10,11]
Various studies reported a wide range of PEI between 22–73%among healthcare workers.[7,9,11,12] It was found that about 23% of our subjects had a PEI experience during last year and about 67% of them reported PEI experience at all times. The result of our study was consistent with these studies.
Around 30.3% of those who had PEI experience during past years declared that they did report needlestick injuries, and 56.1% of dentists declared that, they did have enough knowledge about protection protocol. In our opinion, the lack of familiarity with the reporting systems and the needlestick therapies center are the main reasons causing PEI.
Incidence reports lead to post-exposure prophylaxis, timely diagnosis of antibody levels and patients' anxiety reduction. In contrast to the younger ones, the rate of nonreported needlestick injuries caused by a lack of knowledge of the treatment protocol increased with age among subjects.
In our study, unlike the general view, it was found that young dentists received higher scores than the experienced dentists. Young dentists had a higher range of PEI reporting and a better understanding of the precaution and treatment protocol. New education seems to have improved the situation among young dentists in the fields of precaution and treatment of PEI.
Information and education do not seem to be sufficient for the experienced dentists and just 74 dentists (56.1%) declared that they did have enough knowledge about protection protocol. For this reason, we held various workshops with the co-operation of Iran Medical Council and Mashhad University of Medical Sciences. We also produced and distributed 20-page pamphlet about precaution and treatment ways of PEI among the dentists.
Shiao et al. stated a lack of experience in using a sharp instrument and lack of familiarity with the reporting system among nursing students as the reasons for not reporting PEI.[13] Burke and Madan reported time-consuming reporting processes as the most commonly reported reason among the physicians.[14]
Salzer et al. found that embarrassment, fear of future job problems, lack of time, and astigmatism are the causes of PEI.[15] In our study, personal carelessness was found as the most frequent cause of PEI. In our opinions, fatigue due to the high load of the dental practice, inexperience about PEI, and insufficient education are the reasons for PEI.
Pervaiz et al. in a systemic review found that the prevalence of PEI among dental healthcare workers in Pakistan ranged from 30 to 73%. The PEI reporting rate was between 15 and 76%, and the lack of awareness of the reporting system was reported as the most common reason.[9] In addition, Shaghaghian et al., in a cross-sectional study conducted among 140 dentists in Shiraz, Iran, found that there is a strong relationship between the level of education and attention to infection control. Moreover, Malik et al. found that 74% of subjects knew the universal guidelines.[4]
Hepatitis B is the world's tenth leading cause of death. On average, 3% of people in Iran carry the virus. The dentists are four times more at risk of hepatitis B than ordinary people. In recent years, vaccination coverage has not been completed in other countries.[8] Fortunately, our study found that all subjects were covered by the vaccination against hepatitis B, showing that the dentists ' knowledge in this field is sufficient.
In 2019, Çiçek-Şentürk et al. using a 9-year data of PEI collected from hospital infection control committees, found that appropriate intervention against an increase in the rate of PEI is effective. They concluded that Infection control committees in hospitals play an important role in raising awareness.[16] Qazi et al. suggested referral to the infection control department to improve awareness and ensure safe practices at the time of employment.[17] In Mashhad city, there are different clinics of infection control committees serving the patients suffering from blood-borne diseases. Based on the low reporting rate of PEI among dentists (about 30%), it is suggested to design some plans for introducing the injured to the infection control centers to record the incident and receive appropriate treatment.
In the current study, subjects declared that files and needles are the most common tools causing PEI. In a study by Siew et al., burs and syringe needle have been found as the more frequent ones.[18] Leggat et al. manifested that, injuries caused by needle and scaler are widespread in Australia.[7] Matsumoto et al. reported that needle, scaler, and ultrasonic-related tools are the most common tools causing injuries among healthcare workers.[1]
Dentists have more risk of needlestick than nonsurgical physicians. Wide gauge (internal lumen) of the needles used for intramuscular or intravenous injections compared with the needles used for intraoral local anesthesia delivery, makes needlestick more dangerous in medical staff. However, the oral cavity is filled with saliva that is the other source of contamination in dentistry. Primary care physicians that work in the wards that face blood and other contaminated body fluid have increased occupational risk.
Conclusion
While PEI remains a health problem among dentists in Mashhad, Iran, we hope that the statistics will mitigate this problem using the training programs. The personal carelessness and inappropriate disposal of needles are the most common reasons for PEI injuries. Moreover, files and needles are the most deleterious tools. 57.3% of subjects got excellent scores. However, 69.7% of dentists did not report their PEI and 43.9% of them were not aware of the protocol. Thus, education does not seem to be enough in this field.
In terms of the factors studied, young dentists also had better performance. Therefore, the authors suggested to check PEI reporting forms and follow them up with high accuracy, and also educational programs for dentists should focus on preventing PEI to control the prevalence of PEI. Also, holding different plans for introducing infection control clinics to the dentists seems to be helpful. Further studies are needed to investigate the effect of a dentist's education and to compare their results to our study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Matsumoto H, Sunakawa M, Suda H, Izumi Y. Analysis of factors related to needle-stick and sharps injuries at a dental specialty university hospital and possible prevention methods. J Oral Sci. 2019;61:164–70. doi: 10.2334/josnusd.18-0127. [DOI] [PubMed] [Google Scholar]
- 2.Siddiqi A, Niazi MIK, De Silva H, Firth N, Konthasingha P, Zafar S. Percutaneous exposure incidents:A review of practice and awareness of current protocols at a dental faculty. Oral Surg. 2017;10:e80–7. [Google Scholar]
- 3.Black Thomas LM. Underreporting of bloodborne pathogen exposures in nursing students. Nurse Educ. 2019 doi: 10.1097/NNE.0000000000000696. doi:10.1097/NNE.0000000000000696. [DOI] [PubMed] [Google Scholar]
- 4.Malik A, Shaukat MS, Qureshi A. Needle-stick injury:A rising bio-hazard. J Ayub Med College Abbottabad. 2012;24:144–6. [PubMed] [Google Scholar]
- 5.Pereira MC, Mello FW, Ribeiro DM, Porporatti AL, da Costa S, Junior, Flores-Mir C, et al. Prevalence of reported percutaneous injuries on dentists:A meta-analysis. J Dent. 2018;76:9–18. doi: 10.1016/j.jdent.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 6.Mahboobi N, Mahboobi N, Oliaei P, Alavian SM. Hepatitis C virus;Its implication for endodontists. Iran Endod J. 2014;9:169–73. [PMC free article] [PubMed] [Google Scholar]
- 7.Leggat PA, Smith DR. Prevalence of percutaneous exposure incidents amongst dentists in Queensland. Aust Dent J. 2006;51:158–61. doi: 10.1111/j.1834-7819.2006.tb00420.x. [DOI] [PubMed] [Google Scholar]
- 8.Salehi AS, Garner P. Occupational injury history and universal precautions awareness:A survey in Kabul hospital staff. BMC Infect Dis. 2010;10:19. doi: 10.1186/1471-2334-10-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pervaiz M, Gilbert R, Ali N. The prevalence and underreporting of needlestick injuries among dental healthcare workers in Pakistan:A systematic review. Int J Dent. 2018;2018:9609038. doi: 10.1155/2018/9609038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaghaghian S, Pardis S, Mansoori Z. Knowledge, attitude and practice of dentists towards prophylaxis after exposure to blood and body fluids. Int J Occup Environ Med. 2014;5:146–54. [PMC free article] [PubMed] [Google Scholar]
- 11.Askarian M, Malekmakan L. The prevalence of needle stick injuries in medical, dental, nursing and midwifery students at the university teaching hospitals of Shiraz, Iran. Indian J Med Sci. 2006;60:227–32. [PubMed] [Google Scholar]
- 12.Bhardwaj A, Sivapathasundaram N, Yusof M, Minghat A, Swe K, Sinha N. The prevalence of accidental needle stick injury and their reporting among healthcare workers in orthopaedic wards in General Hospital Melaka, Malaysia. Malays Orthop J. 2014;8:6–13. doi: 10.5704/MOJ.1407.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shiao JS, McLaws ML, Huang KY, Guo YL. Student nurses in Taiwan at high risk for needlestick injuries. Ann Epidemiol. 2002;12:197–201. doi: 10.1016/s1047-2797(01)00303-9. [DOI] [PubMed] [Google Scholar]
- 14.Burke S, Madan I. Contamination incidents among doctors and midwives:Reasons for non-reporting and knowledge of risks. Occup Med (Lond) 1997;47:357–60. doi: 10.1093/occmed/47.6.357. [DOI] [PubMed] [Google Scholar]
- 15.Salzer HJ, Hoenigl M, Kessler HH, Stigler FL, Raggam RB, Rippel KE, et al. Lack of risk-awareness and reporting behavior towards HIV infection through needlestick injury among European medical students. Int J Hygiene Environ Health. 2011;214:407–10. doi: 10.1016/j.ijheh.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 16.Cicek-Senturk G, Tekin A, Gurbuz Y, Tütüncü EE, Sevinç G, Kuzi S, et al. Retrospective investigation of 9 years of data on needlestick and sharps injuries:Effect of a hospital infection control committee. Am J Infect Control. 2019;47:186–90. doi: 10.1016/j.ajic.2018.07.015. [DOI] [PubMed] [Google Scholar]
- 17.Qazi AR, Siddiqui FA, Faridi S, Nadeem U, Umer NI, Mohsini ZS, et al. Comparison of awareness about precautions for needle stick injuries:A survey among health care workers at a tertiary care center in Pakistan. Patient Saf Surg. 2016;10:19. doi: 10.1186/s13037-016-0108-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Siew C, Gruninger SE, Miaw CL, Neidle EA. Percutaneous injuries in practicing dentists. A prospective study using a 20-day diary. J Am Dent Assoc. 1995;126:1227–34. doi: 10.14219/jada.archive.1995.0357. [DOI] [PubMed] [Google Scholar]


