Background.
Patients who travel long distances to undergo liver transplantation have limited opportunities to develop confidence in their new healthcare providers and experience fewer support visits from family and friends at the transplant site. The objectives of this study were to document the psychological and financial impact of having to travel long distances for liver transplantation in adult liver disease patients.
Methods.
This was a single-center, prospective study that used a 7-question survey, including Likert scales, patient recall, and administrative databases.
Results.
Ninety-six adult outpatient liver transplant recipients (59% males; mean age, 43.1 ± 2.1 y) participated in the survey. Approximately 70% (more so among males and higher educated patients) felt that they had sufficient time to develop confidence in their new healthcare providers and 87% felt that confidence in their local healthcare providers had not been diminished by undergoing the procedure elsewhere. Forty-four percent of patients felt that their overall liver transplant experience had been compromised by more limited opportunities for support visits, a perception that was twice as common in females. Median out-of-pocket expenses were under $5000, and inflation corrected costs to third-party payers have been stable for the past 20 y.
Conclusions.
The principal psychological impact of travelling long distances for liver transplantation relates to the consequences of fewer support visits. Confidence in the new and local healthcare teams is not compromised by such travel in most patients. Out-of-pocket expenses are under $5000, and transplant costs to third-party payers have remained stable over the past 20 y.
Since the early 1980s, orthotopic liver transplantation has been considered a nonresearch procedure for the treatment of adult patients with advanced liver disease.1 Over the subsequent 4 decades, approximately 150 transplant centers have been established in North America. Although these centers are well suited for servicing the needs of the local population and those residing in close proximity to the transplant site, they present some unique psychological and financial challenges to patients having to travel long distances to undergo the procedure.2–8 Some of these challenges include more limited opportunities to establish confidence in their new healthcare team; the potential for diminished confidence in their local healthcare providers; the perception that more remote patients may not receive as high a priority for the procedure and/or as high-quality perioperative care as local patients; and relatively limited opportunities for family, friends, and spiritual support visits.
Numerous previous studies/reports have documented the costs of developing and maintaining a liver transplant program, but to date, none have described out-of-pocket costs incurred by the patient/family members and costs to third-party payers in nontransplant jurisdictions within the context of socialized healthcare.9 Moreover, changes to these costs over time have also not been previously described. Such information is essential for social media–driven campaigns such as GoFundMe to raise support for transplant candidates and/or their families and to inform cost projections for centers considering developing transplant programs at their site.
MATERIALS AND METHODS
Adult patients attending a post-liver transplant outpatient clinic at the Health Sciences Center in Winnipeg, Manitoba, Canada, during the periods between May and August 2018 and 2019 were invited to participate in the study. Liver transplantations had been performed in 5 sites that ranged in distance from 1303 to 2270 km from Winnipeg. Acute illness and the presence of hepatic encephalopathy served as exclusion criteria. After obtaining informed verbal consent, a survey was administered in person–person interviews by the same study investigator (M.G.V.I.). The survey (Table 1) was created by a professional psychologist (M.B.) and largely consisted of a 5-point Likert psychometric or rating scale with number 1 representing the most positive and 5 the most negative option.
TABLE 1.
Study survey and (response options)
In addition to survey responses, the following information was collected and with the exception of the number of visitors and out-of-pocket expenses, verified by the transplant team:
Patient’s age, sex, and highest level of education.
Underlying liver disease, date of transplant, site of transplant, and length of stay at the transplant site.
Number of visits to the transplant site before transplantation, number of visiting family members (in addition to the single, provincially covered, support person), friends, or clergy.
An estimate of the out-of-pocket expenses to the patient and visiting family/friends.
Out-of-pocket expenses were based on patient recall and estimates, whereas third-party payer costs of liver transplantation performed outside the province from 1996/1997 to 2016/2017 were obtained from a Manitoba Health administrative database. The data included inpatient, outpatient, drug, and transportation expenses. Medical services and transportation costs for consultations and presurgery assessments were included in the expenses. Financial data were corrected for inflation by employing yearly inflation rates published by Statistics Canada.
Statistics
Data collected from the patient survey were analyzed by descriptive statistics. Chi-square tests were used to determine if responses were disproportionately common in groups of a certain age, sex, education level, underlying liver disease, or transplant site. Missing responses were excluded from the data analyses. Modeling was performed to evaluate the impact of a variety of predictors on patient out-of-pocket costs. In accordance, all models used inflation adjusted cost as the outcome. Variable transformation was not performed, as this was not warranted by Box–Cox testing. Cost outliers (>4 SD beyond the mean) were removed.
Univariate regression models were initially built for each of the predictors (with inflation adjusted cost as the outcome), in addition to a saturated multiple regression model including all variables. The saturated model included the predictor variables: disease, age at transplant, sex, transplant center, number of family member visits, and length of stay. Model selection was performed using a backward elimination technique. The minimum adequate model was found to be a regression model with inflation adjusted cost as the outcome, and disease type and length of stay as the predictors. The assumptions of a multiple regression were met (the data were approximately normally distributed), and variances were equal (regression of residuals versus fitted, P = 0.051). Normality was evaluated using Q-Q plotting, and added variable plotting was used to determine variable relationships. All statistical analyses were performed using R version 3.6.0. The results presented represent the mean ± SEM unless otherwise indicated.
This study was approved by the University of Manitoba’s Conjoint Ethics Review Committee.
RESULTS
Patient Population
Ninety-six of 185 patients were approached during the time intervals of the interviews. No patients were deemed too sick to participate. As was the case for the remaining 89 patients, all 96 participating patients had to travel long distances for their transplant procedures.
As shown in Table 2, the majority of patients were male (57 of 96 [59%]). The mean age at transplantation was 43.1 ± 2.1 y. Three patients were transplanted when under 18 y of age. Subjective responses to questions 1–7 from these patients were not included in the overall analyses.
TABLE 2.
Demographic and clinical features of the study population
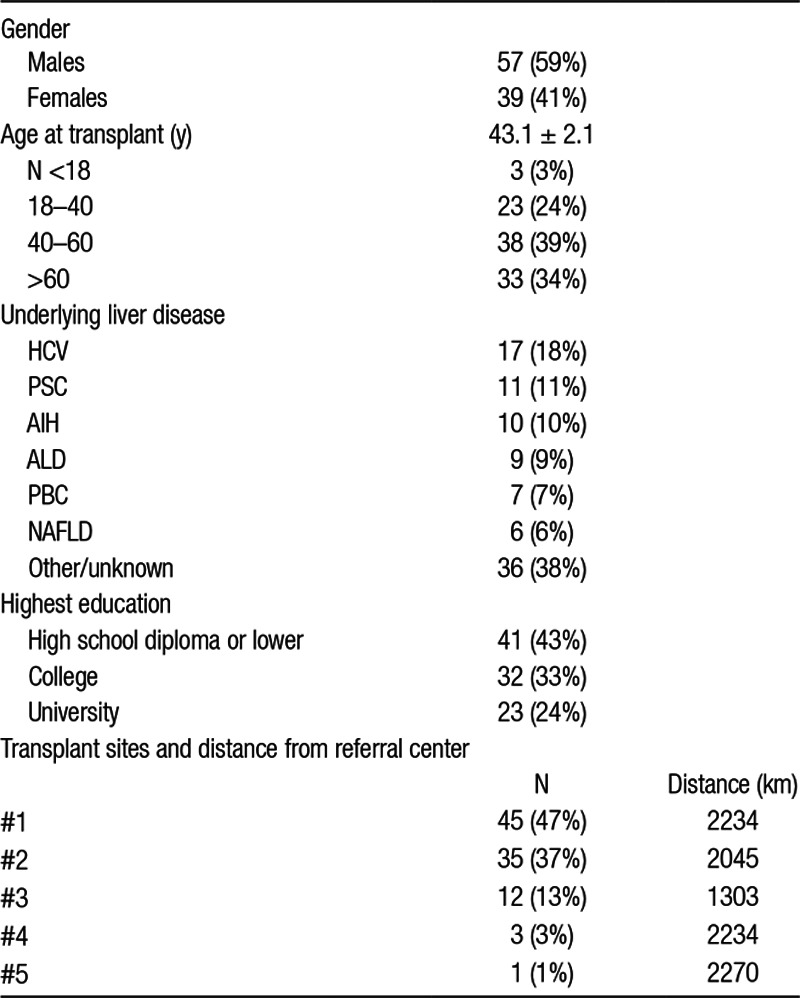
The underlying liver diseases primarily responsible for the transplantation included hepatitis C (18%), primary sclerosing cholangitis (11%), autoimmune hepatitis (10%), alcoholic cirrhosis (9%), primary biliary cholangitis (7%), nonalcoholic fatty liver disease (6%), and other or patient unaware of the underlying diagnosis (38%).
Forty-one (43%) patients had a high school diploma or less as the maximum formal education achieved, 32 (33%) a college, and 23 (24%) university degree.
Transplant Centers and Visits
Five transplant sites (all Canadian) had been used. For the most part, these sites had been selected based on arrangements established by the referring and recipient healthcare teams and not patient preferences. Transplant site #1 performed the procedure in 47% of patients; site #2, 37%; site #3, 13%; site #4, 3%; and site #5, 1%.
The mean number of patient visits to the transplant center (inclusive of the procedure) was 1.4 ± 0.3 (range, 1–19). The mean total length of stay (for the procedure and immediate, postdischarge retention at the site) was 36.2 ± 2.7 d (range, 6–90 d).
Patients had a mean of 3.7 ± 0.4 (range, 0–19) family or friend visitors during their hospital stay. There were no visits from home-based, spiritual supporters. In most cases, travel to and from these sites by family and/or friends was by air.
Survey Responses
#1. Approximately 80% of patients were neither pleased nor disappointed when informed the transplant procedure would not be performed locally (Figure 1A). Of the remaining patients, twice as many were disappointed as pleased (14% versus 7%, respectively).
#2. The majority of patients (69%) felt they had sufficient time to develop confidence in the transplant team before the procedure, but 31% felt otherwise, with the majority feeling that time and exposure had been inadequate (Figure 1B). Males were more likely than females to develop strong confidence (Likert response 1) in the transplant team (43% versus 22%; P = 0.004) as were university- or college-educated patients compared with those with lower levels of education (47% versus 18%; P = 0.04).
#3. Eighty-five percent of patients felt that confidence in their local healthcare providers had not changed, whereas a total of 8% had less confidence and 7% more on return to their home site (Figure 1C).
#4. Only 10% of patients felt they might have received a transplant earlier had a transplant program been available to them locally. The majority of these individuals were in the oldest age cohort (Figure 1D).
#5. Most patients (85%) felt they received the same attention and quality of care as local patients; however, 4% felt they received less and 10% better care (Figure 1E).
#6. The perception of more limited opportunities for family/friend/spiritual support was of no concern to 50% of patients, whereas a total of 44% felt that it had a negative effect on their overall experience (40% of these feeling very much so) (Figure 1F). Seven percent of patients felt more limited support visits were beneficial. Although not reaching statistical significance, the perceived negative effect was more common in females than in males (62% versus 31%, respectively; P = 0.054).
#7. A total of 70% of patients would have preferred (the majority “strongly”preferred) to have undergone the procedure at their local site, whereas 17% had no preference and 13% preferred to have travelled elsewhere (Figure 1G). Of the latter cohort, university-educated patients more often selected this choice than college and high school or less patients (24%, 13%, and 8% respectively; P = 0.01).
FIGURE 1.
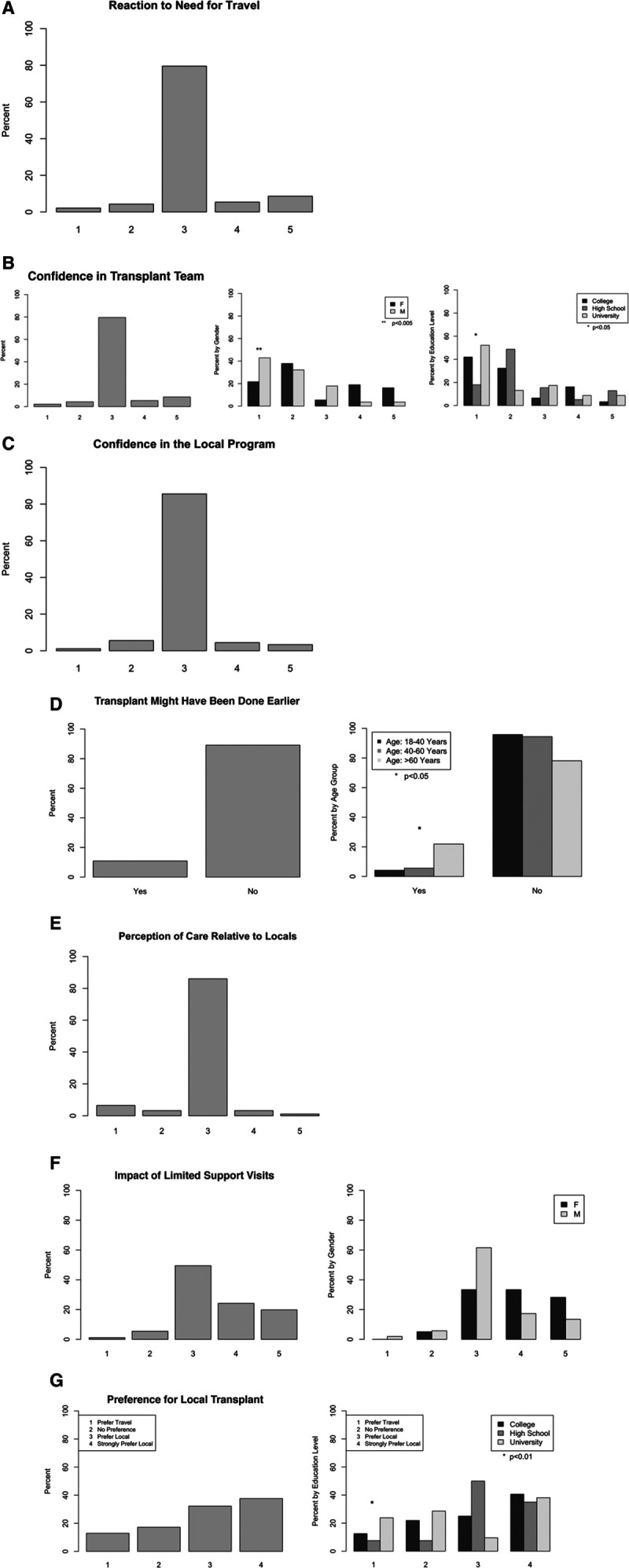
Responses to questions regarding the psychological impact of being informed distant travel was required for the procedure (A); confidence level in transplant team (the difference between males [M] and females [F] having strong confidence in the transplant team [Likert response 1] was significant at P = 0.004 as were the mean responses of university/college-educated individuals vs those with high school or lower levels of education [P = 0.04]) (B); confidence in local healthcare team (C); possibility of being transplanted earlier (older individuals [>60 y] felt they might have been transplanted earlier had they resided near or at the transplant site than younger individuals [P < 0.05]) (D); quality of care relative to local patients (E); impact of limited support visits (the more common negative impact among women did not reach statistical significance when compared with that of men [P = 0.054]) (F); and preference for the procedure to have been performed locally (university educated individuals more often preferred to have traveled for the procedure than college- or high school–educated individuals [P < 0.01]) (G). In all but (A) and (D), Likert scale of 1–5 was used with 1 representing the most positive and 5 the most negative options.
Patient/family Costs
The median out-of-pocket expenses to the patient and/or their family/friends who travelled to the transplant center was $4645 (range, $0–$117 624). These costs predominantly consisted of transportation, accommodations, and food. Older patients and length of stay positively correlated with out-of-pocket expenses (data not shown).
Third-party Payer Costs
As shown in Figure 2A, total costs to the patient’s third-party payer have not significantly changed when corrected for inflation over the past 20 y (R2 = 0.023; P = 0.48) with the mean cost remaining relatively stable at $231 285 ± 21 842. Similarly, travel (Figure 2B) and drug (Figure 2C) costs over the same period have also remained stable over this time period (R2 = 0.00346 and −0.04757, respectively).
FIGURE 2.
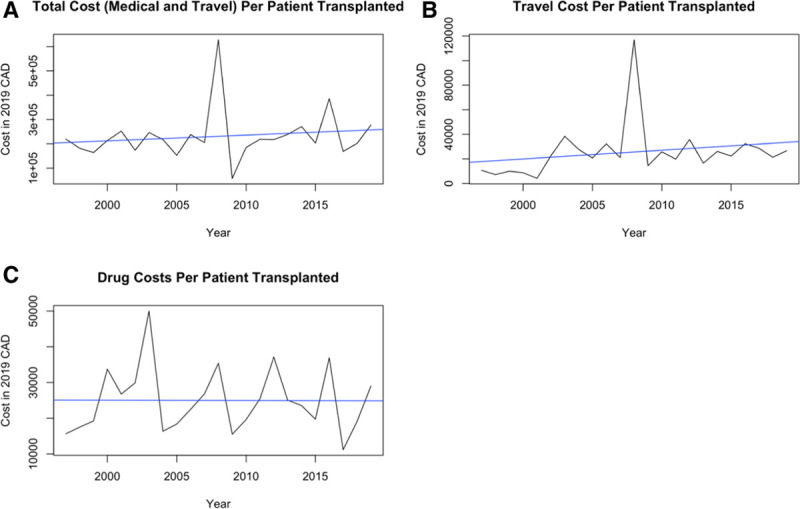
Third-payer costs of liver transplantation (A); “out-of-pocket” expenses (B); and drug costs (C) per patient over 20 y (1996/1997 to 2016/2017).
DISCUSSION
Overall, the results of this study suggest that liver transplant patients who must travel long distances to undergo the procedure do not have a diminished sense of confidence in their healthcare providers (transplant center or local) or feel their care has been compromised as a result of the distances involved. Women and individuals with a high school education or lower were less confident in the transplant center’s staff, but this opinion constituted <20% of all responses. However, dissatisfaction with the relatively limited opportunities for family/friend/spiritual support visits was evident, particularly among women. The results also indicate that out-of-pocket expenses are under $5000 and third-party payer costs have been stable at approximately $230 000 over the past 20 y.
Lack of patient confidence in healthcare providers can lead to “decreased patient compliance, worse clinical outcomes, corrosive physician–patient interactions, and physician burnout.”10,11 Thus, responses to questions 2 and 3 were particularly important to determine whether patients who had to travel long distances felt they had sufficient time to develop confidence in their new healthcare team and whether the process of receiving what might be considered a higher level of care from that team diminished their confidence in the local healthcare providers on return home from the transplant center. That 69% of patients felt they had sufficient time to develop confidence in the transplant team and 92% had the same or a higher level of confidence in their local healthcare providers indicates that for the most part, such concerns are not warranted. Nonetheless, additional efforts by the transplant team to instill trust in women and patients with more limited education should be considered.
Another question of confidence was addressed in questions 4 and 5 where a patient’s confidence and trust in the “system” were addressed. Here, 90% of patients who had to travel long distances felt they were not being denied an earlier transplant by virtue of not being “local” to the transplant center and 96% felt they received the same level of care or better than local patients. Relevant to this issue are data from previous reports indicating that patients who live remote distances from transplant centers are less likely to be transplanted than patients living in close proximity to these sites, albeit for a variety of reasons.12
Additional studies are required to determine the precise explanation for why females were twice as likely as males to be negatively impacted by more limited family, friend, and spiritual visits and what can be done to resolve that impression. Of note, the survey was not designed to rate that experience. Thus, less favorable could reflect a change from a very favorable to somewhat less favorable but not necessarily of practical relevance. Nonetheless, this perception may have been the principal reason why the majority of patients (70%) would have preferred the procedure had been performed locally.
The advent of social media has facilitated efforts to provide financial support for worthwhile causes. Even in countries with socialized healthcare systems, public campaigns to support patient/family travel and/or procedure-related costs are common. Although the methodology used in this study to determine the extent of such out-of-pocket expenses was relatively limited and the responses unsubstantiated, the amounts identified will help to serve as a general target for such campaigns in the future.
When adjusted for inflation, the overall travel and drug costs to third-party payers for liver transplantation at transplant sites distant from the patient’s residence have remained relatively stable. The explanation for this somewhat unexpected finding may reflect a balance between increasing direct/indirect costs and shortening hospital stays, particularly in high-cost areas such as intensive and intermediate care units. It remains to be determined whether hospital stays have reached the minimum duration of time. Were that the case, future increases in third-party payer costs are likely to be incurred.
There are a number of limitations to this study that warrant emphasis. First, the study was single-centered which also precluded comparisons with patients who do not have to travel long distances for liver transplantation. Second, although developed by a professional psychologist, the questionnaire has yet to be validated. Third, the accuracy of responses regarding out-of-pocket expenses could not be verified. Fourth, a response bias may have occurred as result of the survey being performed and conducted by the patient’s local healthcare providers. Finally, the analysis was confined to costs incurred in a socialized healthcare system.
In conclusion, the results of this study did not identify substantial or common negative psychological effects, high out-of-pocket expense, or increasing liver transplant-related costs to third-party payers as compelling reasons for establishing a liver transplant program at sites where such programs do not presently exist.
Footnotes
Published online 22 May, 2020.
D.P., M.G.V.I., M.B., and G.Y.M. involved in conception or design of the work; involved in drafting the work or revising it critically for important intellectual content; involved in final approval of the version to be published; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
The authors declare no funding or conflicts of interest.
REFERENCES
- 1.Bodzin AS, Baker TB. Liver transplantation today: where we are now and where we are going. Liver Transpl. 2018; 24:1470–1475. doi:10.1002/lt.25320 [DOI] [PubMed] [Google Scholar]
- 2.Dang BN, Westbrook RA, Njue SM, et al. Building trust and rapport early in the new doctor-patient relationship: a longitudinal qualitative study. BMC Med Educ. 2017; 17:32 doi:10.1186/s12909-017-0868-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kelly C, Hulme C, Farragher T, et al. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open. 2016; 6:e013059 doi:10.1136/bmjopen-2016-013059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaylin DS, Held PJ, Port FK, et al. The impact of comorbid and sociodemographic factors on access to renal transplantation. JAMA. 1993; 269:603–608 [PubMed] [Google Scholar]
- 5.Wolfe RA, Ashby VB, Milford EL, et al. Differences in access to cadaveric renal transplantation in the United States. Am J Kidney Dis. 2000; 36:1025–1033. doi:10.1053/ajkd.2000.19106 [DOI] [PubMed] [Google Scholar]
- 6.Oniscu GC, Schalkwijk AA, Johnson RJ, et al. Equity of access to renal transplant waiting list and renal transplantation in Scotland: cohort study. BMJ. 2003; 327:1261 doi:10.1136/bmj.327.7426.1261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tonelli M, Hemmelgarn B, Kim AK, et al. ; Alberta Kidney Disease Network. Association between residence location and likelihood of kidney transplantation in Aboriginal patients treated with dialysis in Canada. Kidney Int. 2006; 70:924–930. doi:10.1038/sj.ki.5001607 [DOI] [PubMed] [Google Scholar]
- 8.Axelrod DA, Dzebisashvili N, Schnitzler MA, et al. The interplay of socioeconomic status, distance to center, and interdonor service area travel on kidney transplant access and outcomes. Clin J Am Soc Nephrol. 2010; 5:2276–2288. doi:10.2215/CJN.04940610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.van der Hilst CS, Ijtsma AJ, Slooff MJ, et al. Cost of liver transplantation: a systematic review and meta-analysis comparing the United States with other OECD countries. Med Care Res Rev. 2009; 66:3–22. doi:10.1177/1077558708324299 [DOI] [PubMed] [Google Scholar]
- 10.Weng FL, Lee DC, Dhillon N, et al. Characteristics and evaluation of geographically distant vs geographically nearby living kidney donors. Transplant Proc. 2016; 48:1934–1939. doi:10.1016/j.transproceed.2016.03.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schulz K, Kroencke S. Psychosocial challenges before and after organ transplantation. Dovepress. 2015; 2015:45–58. doi:10.2147/TRRM.S53107 [Google Scholar]
- 12.Goldberg DS, French B, Forde KA, et al. Association of distance from a transplant center with access to waitlist placement, receipt of liver transplantation, and survival among US veterans. JAMA. 2014; 311:1234–1243. doi:10.1001/jama.2014.2520 [DOI] [PMC free article] [PubMed] [Google Scholar]


