Abstract
Background
Helicobacter pylori is a spiral-shaped gram-negative bacteria associated with peptic ulcer, gastritis and gastric cancer. The global burden and occurrence of H. pylori infection remains prevalent and worldwide. Despite this, the trend of the bacterial resistance is not recently studied which can help in the adoption of global, regional and local prevention strategies.
Objective
The aim of the study was to systematically review the existing published literature that presents the estimate of H. pylori antibiotic resistance.
Methods
A protocol was primarily registered in PROSPERO International prospective register of systematic reviews and has given a registration number CRD42017068710. It was registered after checking whether there was similar study being conducted. A database search (PubMed/Medline and Google scholar) was used to collect relevant articles. A standardized form was prepared for the extraction of relevant data from studies which fulfilled the eligibility criteria. A National Institute for Health research (NIH)-based quality assessment tool was utilized to assess the quality of studies included in the study.
Results
Our searching process has retrieved a total of 288 publications which later resulted in 38 articles for full-text review. Among the 38 articles reviewed in full text, 14 studies were included which fulfilled the inclusion criteria. H.pylori-pooled overall prevalence rate of antibiotic resistance was found to be 4.55% (95% confidence interval (CI): 3.96–5.22%) to amoxicillin, 27.22% (95% CI: 25.89–28.58%) to clarithromycin, 39.66% (95% CI: 38.20–41.15%) to metronidazole, and 22.48% (95% CI: 21.24–23.76%) to levofloxacin.
Conclusion
The primary antibiotic resistance pattern of H. pylori is increasing worldwide. Thus, implementation of local drug susceptibility surveillance program, rational prescribing and use of antibiotics are necessary.
Keywords: H. pylori, primary antibiotics resistance, drug resistance, systematic review
Background
Helicobacter pylori is a spiral-shaped gram-negative bacteria which colonize the gastric or intestinal mucosa of humans and induce histologic inflammation.1,2 It is associated with peptic ulcer, gastritis and cancer.2,3 The infection of H. pylori remains a prevalent and worldwide chronic disease. It causes more than 90% and 80% of duodenal and gastric ulcers, respectively.1,4 This shows the world population is highly infected with H. pylori. About one-third of the adult population residing in Northern Europe and Northern America were found infected with H. pylori. Moreover, above 50% of population living in Southern and Eastern Europe, South America and Asia were infected with H.pylori. This was over pronounced in immigrants coming from countries with higher prevalence of H. pylori.5
Worldwide, various eradication strategies are proposed for the treatment of H. pylori infection including triple therapy, sequential therapy, concomitant therapy, quadruple therapy and hybrid therapy.6,7 The Maastricht IV Florence Consensus report overemphasized, eradication of H. pylori infection produces a long-term relief of dyspepsia. However, a long-term treatment with proton pump inhibitors is associated with the development of a corpus-predominant gastritis which accelerates to the development of atrophic gastritis.8
Antibiotic resistance is nowadays the challenging issue in the treatment of bacterial infections. It is still continuing as global public health threat specifically in most of the major microbial pathogens.9,10 Similar to other bacterial resistances, H. pylori drug resistance is also the main factor affecting the efficacy of current treatment regimens.11 Various resistance mechanisms are described earlier however, point mutation on the surface of bacterial chromosome is described as the main causes of treatment failure due to drug resistance.12
H. pylori resistance to antibiotics is the major cause of treatment failure.13 Patients with sensitive isolates of clarithromycin (CLR) isolates have shown 100% eradication compared to none of patients with CLR resistant isolates.14 This indicates CLR resistance was responsible for the treatment failure. In addition to this, there are different mechanisms of resistance the bacteria can remain unharmed. These includes redox intracellular potential, pump efflux systems and membrane permeability for medications including to CLR, metronidazole (MTR), Quinolones, amoxicillin (AMX) and tetracycline.15 Prolonged hospitalization and use of antibiotics without prescription were also indicated as major reasons for the increased incidence of bacterial resistance.16
In vitro antibiotic susceptibility tests of H. pylori need standard culture because it is a relatively fastidious and slow-growing microaerophilic microorganism.17 Antibiotic susceptibility test helps in the proper prescribing and use of medications, and increase patient treatment outcome. Despite this, the trend of bacterial resistance is not yet recently studied which helps in the adoption of appropriate global and regional prevention strategies. Therefore, the purpose of this review was to systematically review and analyze existing published literature that presents estimates of primary antibiotic resistance of H. pylori in adult population.
Methods
Search Strategy
Before beginning of the study, the recent publication of the research question was checked to prevent over duplication in PROSPERO International prospective register of systematic reviews and had registered with a registration number; CRD42017068710. A comprehensive systematic search was done using searching key terms; H. pylori antibiotic resistance, amoxicillin, clarithromycin, metronidazole, and levofloxacin adding Boolean terms OR, AND, and NOT to gather relevant articles of a consecutive three years (2015 to 2017). A search engines; PubMed/Medline and Google scholar were used to collect relevant literature (Supp 1 record identification).
Eligibility Criteria
Studies conducted in adult age group greater than eighteen, bacteria confirmed on endoscopic observation/diagnosis from gastric/duodenal biopsy, previously never taken H. pylori treatment, H. pylori infection without gastric/duodenal cancer, had no prior 2-weeks history of acid secretion inhibitors drug intake (proton pump inhibitors or H2-blockers), had not undergone gastric surgery and published in English language between 2015 and 2017 were the eligibility criteria for inclusion in the study.
Selection and Extraction of Data
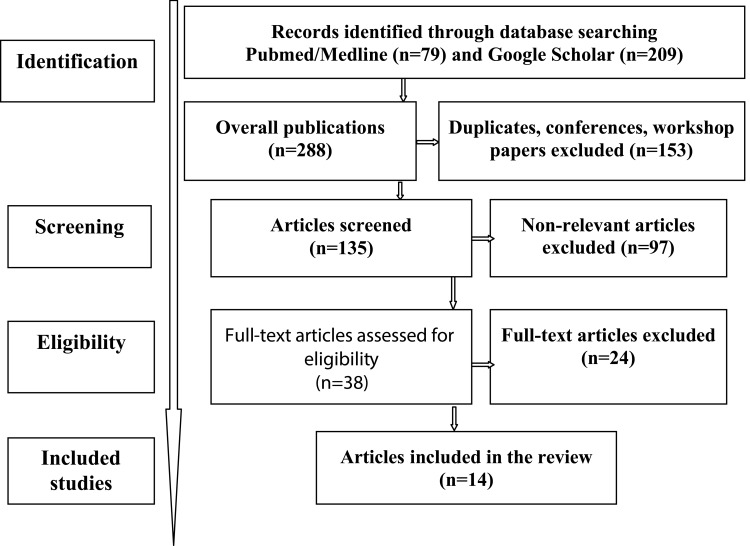
Data were extracted using a standardized pre-prepared table to collect similar evidence from each literature. The evidence extracted includes: author/s name and year of the study, study area or country, number of study participants, study period and prevalence estimate of antibiotic resistance. This was based on the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) statement for reporting systematic reviews and meta-analyses of studies flow chart (Figure 1).18
Figure 1.
PRISMA flow chart representation showing the overall searching and article selection process of a study Helicobacter pylori primary resistance pattern to antibiotics.
Note: Adapted from Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. https://doi.org/10.1371/journal.pmed.1000097.18
Statistical Analysis
An initial extraction and estimation of pooled prevalence using Wilson method of double arcsine transformations were done to estimate a confidence interval for a proportion of studies in Excel.19 A pooled overall prevalence rate was estimated with 95% confidence interval (CI). This was interpreted and compared among countries and continents.
Quality Assessment
Two reviewers (GGK and GTD) carried out the initial screening of the citations retrieved in the searches based on titles and abstracts followed by a full-text assessment of any article identified as being potentially eligible. Any discrepancies during the assessment had resolved by the team. Both reviewers have made a methodological quality assessment on the included eligible studies. The National Institute for Health research (NIH) based Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies was used to assess the methodological quality of studies included in the systematic review rating; good = 2, fair = 1 and poor (cannot be determined, not reported or not applicable) = 0.20
Results
Search results
Our searching process has retrieved a total of 288 publications which later resulted in 38 articles for full-text review. Among 38 articles reviewed in full text, 14 studies have been included for the study which fulfilled the inclusion criteria.21,24–36 The selection and screening process is presented in detail (see Figure 1).
Characteristics of Studies
Primary Resistance to Amoxicillin
Among patients (n=4218) previously never taken the treatment regimen, no resistance was reported in Europe and North America for AMX. In contrast to this, higher resistance rate was reported from Africa (17.7%). Asian and Latin American studies also reported comparable resistance pattern of 3.9% and 4.4%, respectively. A study conducted in Egypt, among 46 study participants almost half of them were non-susceptible to AMX. Similar to this, a study conducted in Nigeria and Peru reported one-third of H. pylori positive patients were non-susceptible. But, no resistances were seen in Morocco, Poland, Turkey, America, Canada and Nepal.
Primary Resistance to Clarithromycin
Clarithromycin (CLR) is a Macrolide derivative used in the treatment of H. pylori eradication. CLR resistance has shown an association in predicting treatment failure of H. pylori eradication therapy.22 Comparable resistance rate was reported in Europe (31.3%) and Asia (30.9%) respectively. Within this the bacterial non-susceptibility rate was reported as 26.7% in Africa. Low rate of resistance was obtained in North America (18.5%) and South America (19.4) in comparison to other continents. Above half patients were non-susceptible in Poland, Egypt and China. H. pylori resistance of CLR has significantly increased in 2009–10 and 2013–14 as a study reported from china.21
Primary Resistance to Metronidazole
Metronidazole (MTR) is an alternative for penicillin-allergic candidates during H. pylori eradication therapy.8 Almost half of Asian patients were non-susceptible (48.9%) to MTR-based H. pylori treatment and higher rate of resistance was reported in Nigeria, Nepal, China, Peru and Poland with a prevalence rate of 99.1%, 88.1%, 66.8%, 61.8% and 56.7%, respectively.
Primary Resistance to Levofloxacin
It is a promising Fluoroquinolones derivative used in the eradication of H. pylori infection.23 However, a substantial prevalence of resistance was observed especially in North America and Asia; 29.2% and 29.9%, respectively. In addition to this, indispensable primary resistance rate was reported in other continents; Europe (13.0%), South America (7.2%), and Africa (5.7%) in descending order.
Primary Dual and Multiple Antibiotic Resistances
A higher multiple antibiotic resistance rate was reported from Turkey (n=98) CLR-MTR-LVX 18.1% and out of 110 American H. pylori positive patients, 1.8% were resistant for CLR-MTR-LVX and for CLR-MTR, 5.5% for CLR-LVX and MTR-LVX.23 In Poland among 67 participants 32.5%, 1.5%, and 4.5% individuals were non-susceptible for CLR-MTR, CLR-LVX and MTR-LVX, respectively.25 Above the multiple drug resistance, a higher dual resistance rate was also seen in Turkey (n=98); 45.4% and 27.2% to CLR-MTR and to CLR-LVX resistance rate were reported, respectively.23 In addition, dual resistance pattern of 1.8% was reported to MTR/CLR in Singapore. About10.5% (n=76) of Peruvian patients were resistant for AMX/CLR which are parts of the standard triple therapy regimen (Table 1).
Table 1.
Primary Resistance Pattern of Helicobacter pylori to Antibiotics Across Different Countries 2015–2017
| Author(s) and Year | Country | No. of Participants (n) | Study Period | Prevalence of Primary Antibiotic Resistance | |||
|---|---|---|---|---|---|---|---|
| AMX | CLR | MTR | LVX | ||||
| Zhang et al 201521 | China | 375 | 2009–10 | 0.067(0.0478–0.0996) | 0.399(0.3517–0.4504) | 0.668(0.6202–0.7150) | 0.345(0.3003–0.3962) |
| Zhang et al 201521 | China | 950 | 2013–14 | 0.044(0.0329–0.0592) | 0.526(0.4945–0.5579) | 0.638(0.6079–0.6689) | 0.548(0.5166–0.5798) |
| Caliskan et al 201524 | Turkey | 98 | 2012–13 | 0 | 0.367(0.2786–0.4661) | 0.355(0.2693–0.4557) | 0.295(0.2146–0.3926) |
| Ferenc et al 201725 | Poland | 67 | 2011–13 | 0 | 0.552(0.4336–0.6652) | 0.567(0.4481–0.6790) | 0.059(0.0235–0.1437) |
| Ang et al 201626 | Singapore | 170 | 2012–14 | 0.041(0.0201–0.0825) | 0.171(0.1215–0.2343) | 0.482(0.4085–0.5570) | 0.147(0.1016–0.2081) |
| Boehnke et al 201727 | Peru | 76 | 2011–13 | 0.329(0.2338–0.4406) | 0.355(0.2570–0.4674) | 0.618(0.5060–0.7194) | 0.539(0.4282–0.6469) |
| Tamayo et al 201728 | Spain | 91 | 2014–15 | NA | 0.077(0.0378–0.1504) | NA | NA |
| Shiota et al 201529 | America | 110 | 2009–13 | 0 | 0.145(0.0916–0.2233) | 0.173(0.1135–0.2541) | 0.291(0.2142–0.3817) |
| Eng et al 201530 | Canada | 20 | 2012–13 | 0 | 0.40(0.2188–0.6134) | 0.35(0.1812–0.5671) | 0.30(0.1455–0.5190) |
| Sanches et al 201631 | Brazil | 490 | 2012–15 | NA | 0.169(0.1388–0.2051) | NA | NA |
| Miftahussurur et al 201632 | Nepal | 42 | 2012 | 0 | 0.214(0.1171–0.3594) | 0.881(0.7500–0.9481) | 0.429(0.2912–0.5779) |
| Liou et al 201533 | Taiwan | 1395 | 2000–12 | 0.023(0.0169–0.0330) | 0.112(0.0970–0.1302) | 0.257(0.2351–0.2809) | 0.088(0.0744–0.1042) |
| Bouihat et al 201634 | Morocco | 177 | 2014 | 0 | 0.254(0.1958–0.3231) | 0.401(0.3318–0.4747) | 0.107(0.0698–0.1616) |
| Zaki et al 201635 | Egypt | 46 | 2014–15 | 0.478(0.3412–0.6186) | 0.608(0.4646–0.7361) | 0.217(0.1226–0.3557) | NA |
| Harrison et al 201736 | Nigeria | 111 | 2010–13 | 0.333(0.2525–0.4253) | 0.144(0.0907–0.2214) | 0.991(0.9507–0.9984) | NA |
Abbreviations: AMX, amoxicillin; CLR, clarithromycin; LVX, levofloxacin; MTR, metronidazole; NA, not analyzed.
Overall Resistance
From a total of 14 studies retrieved with a total of 4218 study participants of H. pylori positive patients, the overall pooled primary resistance was found; 4.55% at 95% CI: 3.96–5.22% for AMX, 27.22% at 95% CI: 25.89–28.58% for CLR, 39.66% at 95% CI: 38.20–41.15% for MTR, and 22.48% at 95% CI: 21.24–23.76% for LVX. These studies were from different continents including from Europe, North America, South America, Asia and Africa. These studies had used different methods of testing antibiotic susceptibility (Table 2).
Table 2.
Overall Primary Resistance Pattern of Helicobacter pylori to Antibiotics in Adult Population Across Different Continents 2015–2017
| Country | No. of Participants | Overall Prevalence of Primary Antibiotic Resistance | |||
|---|---|---|---|---|---|
| AMX | CLR | MTR | LVX | ||
| Europe | 256 | 0 | 0.3125(0.2588–0.3717) | 0.2852(0.2333–0.3433) | 0.1289(0.0933–0.1755) |
| North America | 130 | 0 | 0.1850(0.1273–0.2600) | 0.2000(0.1403–0.2769) | 0.2923(0.2210–0.3756) |
| South America | 566 | 0.0442(0.0301–0.0644) | 0.1943(0.1639–0.2290) | 0.0830(0.0630–0.1087) | 0.0724(0.0538–0.0968) |
| Asia | 2732 | 0.0395(0.0328–0.0478) | 0.3093(0.2922–0.3269) | 0.4890(0.4703–0.5078) | 0.2990(0.2822–0.3165) |
| Africa | 334 | 0.1766(0.1395–0.2212) | 0.2665(0.2219–0.3163) | 0.5719(0.5183–0.6238) | 0.0569(0.0367–0.0871) |
| Overall | 4218 | 0.0455(0.0396–0.0522) | 0.2722(0.2589–0.2858) | 0.3966(0.3820–0.4115) | 0.2248(0.2124–0.2376) |
Discussion
The treatment success of H. pylori eradication achieved by first-line treatment with a proton pump inhibitor, CLR and AMX have decreased to 70–85% due to increasing CLR resistance.6 Unlike De Francesco et al15 consideration where improved knowledge in drug resistance strategies can result in better infection control, the safe and effective way of bacterial infection prevention and control seems difficult to touch.
The present study found higher resistance rate of CLR recorded in Europe, Asia and Africa. In addition, highest rate of non-susceptibility was seen in Asia for MTR and LVX. Concurrent to this, other worldwide systematic review reported, the overall rate of H. pylori antibiotic resistance was found 11.2% to AMX, 17.2% to CLR, 26.7% to MTR, and 16.2% to LVX. The prevalence rate of CLR, MTR and LVX resistance was significantly increased from Europe to Asia, Northern America and Africa.13 This might be due to irrational use of antibiotics. Similarly, other study also addressed the rate of H. pylori antibiotic resistance were 14.7% to AMX, 19.7% to CLR, 47.2% to MTR, and 18.9% to LVX. The prevalence rate of MTR and AMX resistance was higher in Africa, while CLR and LVX resistance was higher in North America and Asia, respectively.37 Compared to these studies, the primary resistance rate towards CLR substantially increased from 17.2%13 19.7%37 to 27.2%. LVX resistance was also increased from 16.2%13 to 22.5%. Despite the over consumption of AMX and MTR the frequency of non-susceptibility rate of these antibiotics was found decreased. This was in contrary to previous studies.13,37 This might be due to the recent implementation of antimicrobial stewardship and rational antimicrobial practice awareness creation.38 However, even in the recent implementation of the programs the other above mentioned antibiotics resistance rate is substantially increased which necessities other studies to be undertaken.
Country specific systematic review studies reported 16.0%, 22.4%, 61.6%, and 5.3% in Iran;39 9.7%, 24.8%, 33.7%, and 23.8% in Turkey;38 4%, 12%, and 53% in Latin America (no for LVX);41 3.1%, 28.9%, 63.8%, and 28.0%, in China42 to AMX, CLR, MTR and LVX, respectively. The resistance pattern for MTR and LVX was diffused and higher especially to MTR. AMX resistance in Latin America and China was comparable however Turkish and Iranian reviews reported double and almost four times higher from the present study.39–42 This shows the antibiotic susceptibility pattern of H. pylori could not be predicted arbitrary in any country mandating that implementation of local drug susceptibility surveillance program and appropriate or rational prescribing and use of antibiotics is necessary.
Individual and dual antibiotic resistance significantly influences the successful eradication of the bacterial infection. The Maastricht V 2016 guideline report articulates resistance to CLR affect the efficacy of both sequential and triple treatment methods and resistance to MTR affects the treatment success by sequential therapy. Moreover, the report also had reported resistance to CLR and MTR affects the efficacy of sequential, hybrid and concomitant therapy of H. pylori eradication treatment protocols. According to this empirical triple therapy is discouraged. When the resistance of H. pylori is greater than 15% towards CLR at the specified area the treatment should be based on susceptibility pattern to other antibacterials.43
Multi-resistant strains of H. pylori result in life-long infection that might lead to death.44,45 With the reserved treatment alternatives,43,46 a study conducted by Olleik et al on temporin-SH and its analogs resulted in good activity against resistant strains of H, pylori which should be taken as promising treatment alternatives for the eradication of resistant H. pylori infection.47
Appropriate surveillance programs, improved antimicrobial regulations and increased public awareness to region-specific resistance rate of H. pylori isolates are possible mechanisms of prevention for H. pylori associated drug resistance.41,48,49 Therefore, drug susceptibility result of these antibiotics is necessary to select the appropriate drug for the successful eradication of the infection. This fosters rational drug prescribing practice improve patient treatment outcome and avoid unnecessary medical and nonmedical expenditure.
Conclusion
The primary antibiotic resistance of H. pylori is increasing worldwide. The overall resistance rate was found to be 4.55% at 95% CI (3.96–5.22) for amoxicillin; 27.22% at 95% CI (25.89–28.58) for clarithromycin; 39.66% at 95% CI (38.20–41.15) for metronidazole; and 22.48% at 95% CI (21.24–23.76) for levofloxacin. The antibiotic susceptibility pattern of the H. pylori could not be predicted arbitrary in any country mandating that implementation of local drug susceptibility surveillance program and appropriate or rational prescribing and use of antibiotics as necessary.
Abbreviations
AMX, amoxicillin; CLR, clarithromycin; H. pylori, Helicobacter pylori; LVX, levofloxacin; MTR, metronidazole; NHS, National Institute for Health research.
Data Sharing Statement
The datasets used for this study should be accessed from the corresponding author on reasonable request.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare they have no conflicts of interest in this work.
References
- 1.CDC. Helicobacter Pylori. Fact Sheet for Health Care Providers. Department of Health and Human Services; 1–4. 1998. [Google Scholar]
- 2.Blanchard TG, Nedrud JG. Laboratory maintenance of Helicobacter species. Curr Protoc Microbiol. 2012;24:8B.1.1-8B.1.19. doi: 10.1002/9780471729259.mc08b01s24 [DOI] [PubMed] [Google Scholar]
- 3.Smith SM, O’morain C, Mcnamara D. Antimicrobial susceptibility testing for Helicobacter pylori in times of increasing antibiotic resistance. World J Gastroenterol. 2014;20:9912. doi: 10.3748/wjg.v20.i29.9912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chey WD, Wong BC. American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007;102:1808. doi: 10.1111/j.1572-0241.2007.01393.x [DOI] [PubMed] [Google Scholar]
- 5.Eusebi LH, Zagari RM, Bazzoli F. Epidemiology of Helicobacter pylori infection. Helicobacter. 2014;19:1–5. doi: 10.1111/hel.12165 [DOI] [PubMed] [Google Scholar]
- 6.Fuccio L, Laterza L, Zagari RM, Cennamo V, Grilli D, Bazzoli F. Treatment of Helicobacter pylori infection. BMJ. 2008;15:337. [DOI] [PubMed] [Google Scholar]
- 7.Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of Helicobacter pylori infection. Am J Gastroenterol. 2017;112:212–239. doi: 10.1038/ajg.2016.563 [DOI] [PubMed] [Google Scholar]
- 8.Malfertheiner P, Megraud F, O’morain CA, et al. Management of Helicobacter pylori infection, the Maastricht IV/Florence consensus report. Gut. 2012;61:646–664. doi: 10.1136/gutjnl-2012-302084 [DOI] [PubMed] [Google Scholar]
- 9.Levy SB, Marshall B. Antibacterial resistance worldwide: causes, challenges and responses. Nat Med. 2004;10:S122–S129. doi: 10.1038/nm1145 [DOI] [PubMed] [Google Scholar]
- 10.Graham DY, Shiotani A. New concepts of resistance in the treatment of Helicobacter pylori infections. Nat Clin Pract Gastroenterol Hepatol. 2008;5(6):321–331. doi: 10.1038/ncpgasthep1138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishizawa T, Suzuki H. Mechanisms of Helicobacter pylori antibiotic resistance and molecular testing. Front Mol Biosci. 2014;1. doi: 10.3389/fmolb.2014.00019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu W, Yang Y, Sun G. Recent insights into antibiotic resistance in Helicobacter pylori eradication. Gastroenterol Res Pract. 2012;2012:1–8. doi: 10.1155/2012/723183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.De Francesco V, Giorgio F, Hassan C, et al. Worldwide H.pylori antibiotic resistance: a systematic review. J Gastrointestin Liver Dis. 2010;19. [PubMed] [Google Scholar]
- 14.Lee JW, Kim N, Kim JM, et al. Prevalence of primary and secondary antimicrobial resistance of helicobacter pylori in Korea from 2003 through 2012. Helicobacter. 2013;18:206–214. doi: 10.1111/hel.12031 [DOI] [PubMed] [Google Scholar]
- 15.De Francesco V, Giorgio F, Ierardi E, et al. Primary clarithromycin resistance in Helicobacter pylori: the multicentric Italian clarithromycin resistance observational (MICRO) study. J Gastrointestin Liver Dis. 2011;20:235–239. [PubMed] [Google Scholar]
- 16.Alzoubi K, Ayoub N, Al-Sakaji S, Al-Azzam S, Mhaidat N, Masadeh M. Awareness of bacterial resistance among physicians, pharmacists and nurses. Int J Occup Med Environ Health. 2009;22:363–372. doi: 10.2478/v10001-009-0034-3 [DOI] [PubMed] [Google Scholar]
- 17.Owen R. Molecular testing for antibiotic resistance in Helicobacter pylori. Gut. 2002;50:285–289. doi: 10.1136/gut.50.3.285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7): e1000097. 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974–978. doi: 10.1136/jech-2013-203104 [DOI] [PubMed] [Google Scholar]
- 20.Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed May4, 2020.
- 21.Zhang YX, Zhou LY, Song ZQ, Zhang JZ, He LH, Ding Y. Primary antibiotic resistance of Helicobacter pylori strains isolated from patients with dyspeptic symptoms in Beijing: a prospective serial study. World J Gastroenterol. 2015;21:2786. doi: 10.3748/wjg.v21.i9.2786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Agudo S, Pérez-Pérez G, Alarcón T, López-Brea M. High prevalence of clarithromycin-resistant Helicobacter pylori strains and risk factors associated with resistance in Madrid, Spain. J Clin Microbiol. 2010;48:3703–3707. doi: 10.1128/JCM.00144-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rispo A, Capone P, Castiglione F, Pasquale L, Rea M, Caporaso N. Fluoroquinolone-based protocols for eradication of Helicobacter pylori. World J Gastroenterol. 2014;20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Caliskan R, Tokman HB, Erzin Y, et al. Antimicrobial resistance of Helicobacter pylori strains to five antibiotics, including levofloxacin, in Northwestern Turkey. Rev Soc Bras Med Trop. 2015;48:278–284. doi: 10.1590/0037-8682-0027-2015 [DOI] [PubMed] [Google Scholar]
- 25.Ferenc S, Gnus J, Kościelna M, et al. High antibiotic resistance of Helicobacter pylori and its effect on tailored and empiric eradication of the organism in Lower Silesia, Poland. Helicobacter. 2017;22:e12365. doi: 10.1111/hel.12365 [DOI] [PubMed] [Google Scholar]
- 26.Ang TL, Fock KM, Ang D, Kwek ABE, Teo EK, Dhamodaran S. The changing profile of Helicobacter pylori antibiotic resistance in Singapore: a 15 year study. Helicobacter. 2016;21:261–265. doi: 10.1111/hel.12291 [DOI] [PubMed] [Google Scholar]
- 27.Boehnke KF, Valdivieso M, Bussalleu A, et al. Antibiotic resistance among Helicobacter pylori clinical isolates in Lima, Peru. Infect Drug Resist. 2017;10:85–90. doi: 10.2147/IDR.S123798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tamayo E, Montes M, Fernández-Reyes M, et al. Clarithromycin resistance in Helicobacter pylori and its molecular determinants in Northern Spain, 2013–2015. J Glob Antimicrob Resist. 2017;9:43–46. doi: 10.1016/j.jgar.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 29.Shiota S, Reddy R, Alsarraj A, El-Serag HB, Graham DY. Antibiotic resistance of Helicobacter pylori among male United States veterans. Clin Gastroenterol Hepatol. 2015;13:1616–1624. doi: 10.1016/j.cgh.2015.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eng NF, Ybazeta G, Chapman K, et al. Antimicrobial susceptibility of Canadian isolates of Helicobacter pylori in Northeastern Ontario. Can J Infect Dis Med Microbiol. 2015;26:137–144. doi: 10.1155/2015/853287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanches BS, Martins GM, Lima K, et al. Detection of Helicobacter pylori resistance to clarithromycin and fluoroquinolones in Brazil: a national survey. World J Gastroenterol. 2016;22:7587. doi: 10.3748/wjg.v22.i33.7587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Miftahussurur M, Shrestha PK, Subsomwong P, Sharma RP, Yamaoka Y. Emerging Helicobacter pylori levofloxacin resistance and novel genetic mutation in Nepal. BMC Microbiol. 2016;16:256. doi: 10.1186/s12866-016-0873-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liou JM, Chang CY, Chen MJ, et al. The primary resistance of Helicobacter pylori in Taiwan after the national policy to restrict antibiotic consumption and its relation to virulence factors—a nationwide study. PLoS One. 2015;10:e0124199. doi: 10.1371/journal.pone.0124199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bouihat N, Burucoa C, Benkirane A, et al. Helicobacter pylori primary antibiotic resistance in 2015 in morocco: a phenotypic and genotypic prospective and multicenter study. Microb Drug Resist. 2016. [DOI] [PubMed] [Google Scholar]
- 35.Zaki MES, Sherif DM, Ali MA, et al. molecular study of primary clarithromycin resistant Helicobacter pylori strains from Egyptian Centre. Int J Curr Microbiol App Sci. 2016;5:165–173. doi: 10.20546/ijcmas.2016.501.014 [DOI] [Google Scholar]
- 36.Harrison U, Fowora MA, Seriki AT, et al. Helicobacter pylori strains from a Nigerian cohort show divergent antibiotic resistance rates and a uniform pathogenicity profile. PLoS One. 2017;12:e0176454. doi: 10.1371/journal.pone.0176454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ghotaslou R, Leylabadlo HE, Asl YM. Prevalence of antibiotic resistance in Helicobacter pylori: A recent literature review. World J Methodol. 2015;5:164. doi: 10.5662/wjm.v5.i3.164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62:1197–1202. doi: 10.1093/cid/ciw217 [DOI] [PubMed] [Google Scholar]
- 39.Khademi F, Poursina F, Hosseini E, Akbari M, Safaei HG. Helicobacter pylori in Iran: A systematic review on the antibiotic resistance. Iran J Basic Med Sci. 2015;18. [PMC free article] [PubMed] [Google Scholar]
- 40.Kocazeybek B, Tokman HB. Prevalence of primary antimicrobial resistance of H. pylori in Turkey: a systematic review. Helicobacter. 2016;21:251–260. doi: 10.1111/hel.12272 [DOI] [PubMed] [Google Scholar]
- 41.Camargo MC, García A, Riquelme A, et al. The problem of Helicobacter pylori resistance to antibiotics: a systematic review in Latin America. Am J Gastroenterol. 2014;109:485–495. doi: 10.1038/ajg.2014.24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hu Y, Zhu Y, Lu NH. Primary antibiotic resistance of helicobacter pylori in China. Dig Dis Sci. 2017;1–9. [DOI] [PubMed] [Google Scholar]
- 43.Malfertheiner P, Megraud F, O’morain C, et al. Management of Helicobacter pylori infection, the Maastricht V/Florence consensus report. Gut. 2016;1–25. [DOI] [PubMed] [Google Scholar]
- 44.Acar JF. Consequences of bacterial resistance to antibiotics in medical practice. Clin Infect Dis. 1997;24:17–18. doi: 10.1093/clinids/24.Supplement_1.S17 [DOI] [PubMed] [Google Scholar]
- 45.Friedman ND, Temkin E, Carmeli Y. The negative impact of antibiotic resistance. Clin Microbiol Infect. 2016;22:416–422. doi: 10.1016/j.cmi.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 46.Miftahussurur M, Waskito LA, Syam AF, et al. Alternative eradication regimens for Helicobacter pylori infection in Indonesian regions with high metronidazole and levofloxacin resistance. Infect Drug Resist. 2019;12:345. doi: 10.2147/IDR.S187063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Olleik H, Baydoun E, Perrier J, et al. Temporin-SHa and its analogs as potential candidates for the treatment of helicobacter pylori. Biomolecules. 2019;9:598. doi: 10.3390/biom9100598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shmuely H, Domniz N, Yahav J. Regional antibiotic resistance of helicobacter pylori. JSM Gastroenterol Hepatol. 2016;4:1074. [Google Scholar]
- 49.Seck A, Burucoa C, Dia D, et al. Primary antibiotic resistance and associated mechanisms in Helicobacter pylori isolates from Senegalese patients. Ann Clin Microbiol Antimicrob. 2013;12:3. doi: 10.1186/1476-0711-12-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed May4, 2020.