INTRODUCTION
Histoplasma capsulatum (H. capsulatum) is endemic in the midwestern United States and central America.1 It causes a wide range of clinical syndromes, ranging from asymptomatic to life-threatening disseminated disease. The extent of disease depends on the number of conidia inhaled and the host immune system. Most of cases (50–90%) in immunocompetent individuals are asymptomatic and 80% of symptomatic infections are self-limited and require no therapy. Initial exposure to H. capsulatum is usually by inhalation of the conidia into the respiratory tract and may result in pneumonia or chronic cavitary pulmonary infection. Central nervous system (CNS) involvement occurs in 5 to 10% of cases of disseminated histoplasmosis. Clinical presentations of CNS histoplasma infection include meningitis, focal brain, or spinal cord lesions (histoplasmoma), stroke syndromes, and encephalitis.
We report a male patient with a recent history of exposure to chickens who presented with confusion, stroke, and a brain lesion. He was treated with liposomal amphotericin B then itraconazole with good clinical response.
CASE REPORT
A 58-year-old man with past medical history of testicular cancer status post left orchiectomy 30 years prior to presentation. He presented with four-days history of confusion, auditory and visual hallucination, ataxia, urinary incontinence, and right-sided weakness. Two to three weeks prior to this presentation, he developed insomnia, worsening headaches, and right facial pain. He denied neck pain, stiffness, fever, bowel incontinence or seizure activity.
He took care of his friend’s chickens for six weeks up until four weeks prior to admission. On examination, he appeared sick, lethargic, and confused. He manifested right-sided weakness (upper and lower extremities) with motor function of 4/5. He had no neck stiffness or Kerning’s sign. The examination was otherwise normal.
Initial workup showed peripheral white blood cells (WBC) 4.8 K/uL (normal 4.5 – 11.0 K/uL), hemoglobin 14.5 gm/dl (normal 13.5 – 16.5 gm/dl), and platelets 255 K/uL (normal 150 – 400 K/uL). The patient had a lumbar puncture with clear cerebrospinal fluid (CSF): opening pressure 14 cm H2O (normal 10 – 25 cm H2O), red blood cells (RBC) 10 cells/μl (normal < 5 cells/μl), WBC 170 cells/μl (normal < 5 cells/μl), neutrophils 69%, lymphocytes 20%, glucose 25 mg/dl (normal 40 – 75 mg/dl), and protein 150 mg/dl (normal 15 – 40 mg/dl). Gram stain showed moderate neutrophils; no organisms were seen. CSF herpes simplex virus and varicella zoster PCR were negative.
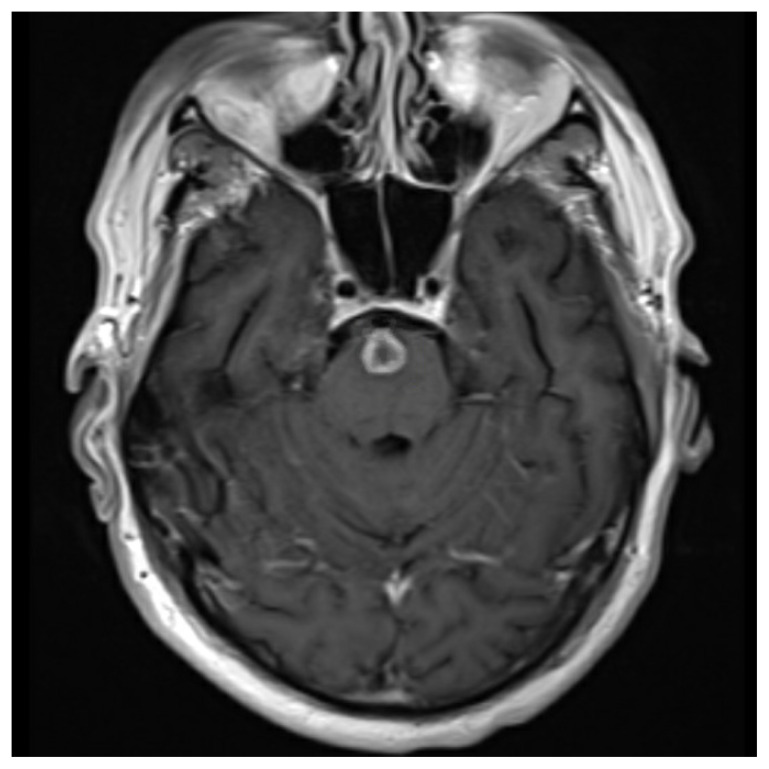
Computed tomography (CT) of the head and cervical spine showed no acute intracranial hemorrhage or fractures. Magnetic resonance image (MRI) of the brain showed a 1 cm rounded enhancing nodule along the anterior pons (Figure 1) and hyperintense lesions within the posterior limb of the left internal capsule and right caudate nucleus (Figure 2). The CT scan of the chest was normal.
Figure 1.
MRI of the head showed a 1 cm round enhancing nodule along the anterior pons.
Figure 2.
MRI revealed hyperintense lesions within the posterior limb of the left internal capsule and right caudate nucleus.
The patient was started on acyclovir, vancomycin, and meropenem for suspected meningoencephalitis. Lumbar puncture was repeated on hospital day three as there was no clinical improvement. CSF WBC was 220 cells/μl, neutrophils 75%, lymphocytes 19%, glucose 20 mg/dl (normal 40 – 75), and protein 187 mg/dl (normal 15 – 40). Repeat MRI on day four showed progression of the acute stroke to involve the left thalamus, anterior limb of the right internal capsule, and right caudate nucleus.
The CSF histoplasma antigen was positive at 14.5 ng/ml on hospital day six. Liposomal amphotericin B was started for treatment of CNS histoplasmosis. Acyclovir, vancomycin, and meropenem were discontinued. Urine histoplasma antigen was negative, but the serum antigen was positive at 1.05 ng/ml. He was treated with six weeks of liposomal amphotericin B followed by 18 months of itraconazole. The CSF fungal culture grew H. capsulatum after 13 days of incubation.
Follow-up MRI of the brain, five months later, showed decreasing edema around the ring enhancing lesion. The patient improved with time, his right-sided weakness and ataxia resolved. He was able to cook and perform simple tasks around the house but continued to have minimal impairment in cognition. Repeat lumbar puncture after 18 months showed red blood cells 0 cells/μl, WBC 0 cells/μl, glucose 63 mg/dl (normal 40 – 75), protein 65 mg/dl (normal 15 – 40). Itraconazole was discontinued after 18 months of treatment.
DISCUSSION
Histoplasma capsulatum is a dimorphic fungus and considered one of the most common fungal respiratory infections in the world.1 The most common system involved in symptomatic histoplasma infection is the pulmonary system. CNS involvement occurs in 5 to 10% of cases of disseminated histoplasmosis.2 The CNS invasion is usually hematogenous; the most common source of invasion is pulmonary infection.3 The most common presentation of CNS histoplasmosis is meningitis, either subacute or chronic.2 Other clinical syndromes include focal brain or spinal cord lesions (histoplasmoma), stroke syndromes, and encephalitis. CNS histoplasmosis should be considered in patients with chronic meningitis or brain lesions in endemic area especially if there is a strong exposure history like to chicken or bat droppings. Our patient was immunocompetent and his clinical presentation was suggestive of meninecephalitis and stroke. His brain imaging showed evidence of a stroke with brain lesion.
In a large multicenter retrospective study of 77 patients with CNS histoplasmosis, 22 patients (29%) were immunocompetent.4 The most sensitive test used for diagnosis was histoplasma antigen in the CSF. It was detected in 35 of 53 (66%) with higher sensitivity in immunocompromised patients 30 of 37 (81%). The second most sensitive test was antibody detection by immunodiffusion or complement fixation in the CSF. It was positive in 19 of 32 tested (59%) with comparable results between immunocompetent and immunocompromised patients. CSF culture or brain tissue biopsy were diagnostic of histoplasmosis in 26 of 69 (38%). The most common CSF abnormality was high protein (> 50 mg/dl) seen in 55 of 71 (77%) followed by pleocytosis (WBC > 5 cells/ml) in 48 of 72 (66%).
The Infectious Diseases Society of America (IDSA) guidelines5 recommend initial treatment of CNS histoplasmosis with liposomal amphotericin B for four to six weeks followed by itraconazole for at least one year. The best triazole after induction therapy remains unclear. Previous animal model studies for histoplasma meningitis showed that fluconazole was inferior to itraconazole despite achieving a better concentration in the CSF.6,7
This case highlighted that CNS histoplasmosis can present as meningoencephalitis and stroke in immunocompetent patients. Clinicians should keep a high index of suspicion for CNS histoplasmosis in patients presenting with subacute/chronic meningoencephalitis, stroke, or brain lesion in histoplasma endemic regions.
REFERENCES
- 1.Wheat LJ, Kauffman CA. Histoplasmosis. Infect Dis Clin North Am. 2003;17(1):1–19. vii. doi: 10.1016/s0891-5520(02)00039-9. [DOI] [PubMed] [Google Scholar]
- 2.Wheat LJ, Batteiger BE, Sathapatayavongs B. Histoplasma capsulatum infections of the central nervous system. A clinical review. Medicine (Baltimore) 1990;69(4):244–260. doi: 10.1097/00005792-199007000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Schestatsky P, Chedid MF, Amaral OB, Unis G, Oliveira FM, Severo LC. Isolated central nervous system histoplasmosis in immunocompetent hosts: A series of 11 cases. Scand J Infect Dis. 2006;38(1):43–48. doi: 10.1080/00365540500372895. [DOI] [PubMed] [Google Scholar]
- 4.Wheat J, Myint T, Guo Y, et al. Central nervous system histoplasmosis: Multicenter retrospective study on clinical features, diagnostic approach and outcome of treatment. Medicine (Baltimore) 2018;97(13):e0245. doi: 10.1097/MD.0000000000010245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wheat LJ, Freifeld AG, Kleiman MB, et al. Clinical practice guidelines for the management of patients with histoplasmosis: 2007 update by the Infectious Diseases Society of America. Clin Infect Dis. 2007;45(7):807–825. doi: 10.1086/521259. [DOI] [PubMed] [Google Scholar]
- 6.Nyalakonda H, Albuerne M, Suazo Hernandez LP, Sarria JC. Central nervous system histoplasmosis in acquired immunodeficiency syndrome. Am J Med Sci. 2016;351(2):177–186. doi: 10.1016/j.amjms.2015.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Ellner JJ, Bennett JE. Chronic meningitis. Medicine (Baltimore) 1976;55(5):341–369. doi: 10.1097/00005792-197609000-00001. [DOI] [PubMed] [Google Scholar]