Abstract
Background
Weight extremes and food insecurity (FIS) represent public-health challenges, yet their associations in childhood remain unclear. We aimed to investigate the longitudinal time-specific relationship between FIS and risk of overweight/obesity and underweight in kindergarten through 8th grade.
Methods
In the prospective Early Childhood Longitudinal Study–Kindergarten Cohort (1998–2007) of 6368 children, household FIS was assessed by the validated US Household Food Security Survey Module in kindergarten, 3rd, 5th and 8th grades. Multivariable linear-regression and Poisson-regression models were computed.
Results
Compared with children experiencing food security (FS), children exposed to FIS in 5th grade had 0.19 [95% confidence interval (CI): 0.07–0.30] and 0.17 (0.06–0.27) higher body mass index z-score (BMIZ) in the 5th and 8th grades, respectively, whereas FIS in the 8th grade was associated with a 0.29 (0.19–0.40) higher BMIZ at the same wave, after adjusting for covariates and FIS at earlier waves. Children with FIS vs FS had 27% (relative risk: 1.27, 95% CI: 1.07–1.51), 21% (1.21, 1.08–1.35) and 28% (1.28, 1.07–1.53) higher risk of overweight/obesity in the 3rd, 5th and 8th grades, respectively, adjusting for covariates and FIS at prior wave(s). Children with FIS vs FS in kindergarten had a 2.76-fold (1.22–6.25) higher risk of underweight in the 8th grade.
Conclusions
Proximal exposure to household FIS was associated with a higher risk of overweight/obesity in the 3rd, 5th and 8th grades. FIS in kindergarten was associated with a risk of underweight in the 8th grade. Thus, FIS coexists in weight extremes during vulnerable early-life windows in the USA, similarly to the global burden of FIS.
Keywords: Food insecurity, overweight, obese, underweight, childhood
Key Messages
In this longitudinal cohort of 6368 school-aged children in the USA, children with food insecurity (FIS) had a higher body mass index z-score than the food-secure children in the 3rd, 5th and 8th grades, respectively.
When FIS exposures at the current and prior waves were assessed simultaneously, proximal exposure to household FIS was associated with a higher risk of overweight or obesity after adjustment for covariates. In contrast, a single, early exposure to FIS, reported in kindergarten, was associated with a higher risk of underweight in the 8th grade, independently of FIS exposures at subsequent waves.
Our findings highlight a double burden of household FIS on the risk of childhood weight extremes characterized by the coexistence of a higher risk of both underweight and overweight or obesity.
Introduction
The prevalence of childhood overweight and obesity in the USA increased at a staggering rate over the last four decades, nearly tripling from 11% to 32% in children aged 2–19 years between 1988–1994 and 2007–2008.1,2 Although the rate of increase has slowed, overweight and obesity remain a major public-health concern for school-aged children, because of the tendency to remain overweight and obese throughout life and of the risk of associated co-morbidities.3,4 The other side of the coin, underweight, is also a public-health concern, as it is typically a marker of undernutrition.5 Despite an overall decreasing trend of underweight in the past few decades, 3%–7% of children and adolescents aged 2–19 years were underweight in the USA in 2007–2008.6
Another significant threat to US children is food insecurity (FIS), defined as limited access or availability to nutritionally adequate food. Nearly 14% of US households with children reported FIS in 2018 compared with the national average of 11.1%.7 Yet, evidence of the association between FIS and overweight/obesity is inconsistent in children; complicating the picture are confounders such as race/ethnicity, poverty, parental factors and the limited longitudinal analyses of exposure to FIS.8–10 Importantly, a paucity of longitudinal data has largely limited the ability to examine the acute vs chronic impact of FIS on childhood growth and identify potential windows of vulnerability in early life. Furthermore, despite the overall low prevalence of underweight among children in the USA, underweight may be disproportionally present among children with socio-economic disadvantage.11 Previous data in developed countries have mostly focused on FIS and childhood overweight/obesity, with scarce data on underweight.12–16 Notably, earlier data were mostly collected in cross-sectional studies and did not account for longitudinal exposure to FIS, which may present missed opportunities to identify specific windows of vulnerability to both ends of childhood weight spectrum in relation to FIS.
Therefore, we aimed to examine the time-specific relationship between exposure to FIS from kindergarten to the 8th grade and risk of overweight/obesity and underweight in the Early Childhood Longitudinal Study–Kindergarten Cohort (ECLS-K), a longitudinal study of a nationally representative sample of children’s early-life experiences and growth in the USA. A better understanding of the role of longitudinal exposure to FIS in childhood overweight/obesity and the understudied area of underweight would inform potential prevention strategies to mitigate risk of childhood weight extremes.
Methods
Study population and design
The ECLS-K had a dual-frame, multi-stage probability cluster sampling design with seven waves of data collection from 1998 through 2007.17 The ECLS-K kindergarten data were representative of all US kindergarteners in 1998–1999, whereas the 8th-grade data were representative of the study population and approximately 80% of US 8th graders in 2006–2007 due to no sample freshening after the 1st grade as described previously in detail.17 In this paper, we examined the four time points with parent-reported data of interest, i.e. the spring of kindergarten (1999), 3rd (2002), 5th (2004) and 8th (2007) grades. Among 20 578 children enrolled in the spring of kindergarten, 9725 remained in the spring of 8th grade, forming the source population.17 In the current analysis, children were excluded if data were missing on household food security (FS) or poverty, health insurance, maternal education, parental depression, sex, race/ethnicity, birthweight and maternal nativity, resulting in a total of 7056 children. Further, we excluded children with missing data on anthropometric measures in the 8th grade (n = 688), rendering a total of 6368 children as our final analytical sample (Supplementary Figure 1, available as Supplementary data at IJE online). The study was approved by the Institutional Review Board of the University of Texas at Austin.
Exposure assessment
Household FS was measured using the validated United States Department of Agriculture 18-item Household Food Security Survey Module (HFSSM).18 The HFSSM was administered by telephone to the parent, usually the mother, at aforementioned waves of the ECLS-K to assess household FIS status over the past year. Households were classified as food-insecure if three or more of the 18 questions were affirmed, otherwise food-secure.19,20
Anthropometric measures
Children’s weight was measured with an electronic scale (SECA, Hamburg, Germany) and height was measured with a Shorr Board (Olney, MD, USA).17 Each measurement was taken in duplicate; the mean was calculated for analysis. The age- and sex-specific body mass index z-scores (BMIZ) were calculated using the Centers for Disease Control and Prevention reference data, with biologically implausible values excluded as recommended.21 Underweight, normal-weight and overweight/obese were classified as an age- and sex-specific BMIZ <5th, 5th–84th and ≥85th percentiles, respectively.22
Covariates
A priori child and parent covariates based on biological and statistical considerations included: child’s sex (male, female), race/ethnicity [non-Hispanic White (NHW), non-Hispanic Black (NHB), Hispanic, Asian/other], birthweight [low (<2500 g), normal (2500–3999 g) or high (>4000 g)], health insurance (yes, no), household poverty (at/above or below the poverty threshold),23 parental depression (yes, no) and maternal nativity (foreign-born, USA-born) and education (<high school, high school or equivalent, some college or above).
Statistical analysis
Data-cleaning procedures for anthropometric measures were described previously.18 We compared measures of central tendency for parental and child characteristics by FIS status and weight status (underweight, normal-weight or overweight/obese) cross-sectionally at each wave using Student’s t-test for continuous variables and Pearson's χ2 test for categorical variables. Child’s BMIZ was compared by FIS status at each wave using the Student’s t-test, with P-values corrected by Bonferroni adjustment for multiple comparisons.
Multivariable linear-regression models estimated the respective beta coefficients (β) and 95% confidence intervals (CIs) of BMIZ in the kindergarten, 3rd, 5th and 8th grades in relation to FIS at current and previous wave(s), adjusting for covariates. Child’s health insurance, household poverty and parental depression were included as time-varying covariates, whereas baseline values of others were used. Similarly, multinomial, multivariable Poisson-regression models with robust standard errors estimated the respective relative risks (RRs) and 95% CIs of overweight/obesity and underweight at each wave. In each model, FIS status at the current and previous wave(s) was simultaneously included to estimate the time-specific association of both proximal exposure to FIS at the current wave and chronic exposures to FIS at previous wave(s) with outcomes of interest (i.e. BMIZ, overweight/obesity or underweight) at a certain study wave, with Bonferroni adjustment for multiple comparisons. All variance inflation factors for each multivariable model were <1.50, suggesting no concern for multicollinearity.24 We also examined the potential interaction between FIS status between two adjacent waves; as none was significant, we did not include interaction terms in the multivariable models.
We explored potential effect modification by major covariates (i.e. race/ethnicity and household poverty). Since no significant effect modification was detected, interaction terms were not included in the final models. Further, we stratified the analysis by child’s sex, but no significant sex dimorphism was observed. To evaluate the potential selection bias due to attrition, we compared the characteristics of participants with missing exposure or covariate data (n = 2669) or missing anthropometric data in the 8th grade (n = 668) with the analytic sample (n = 6368), respectively. Participants with missing covariate data had a slightly smaller proportion of NHWs (66.9%) than the analytic sample (67.5%); no other participant characteristics varied between groups. We accounted for the complex survey design of the ECLS-K by applying the appropriate longitudinal weights to approximate the exact methods for standard error correction, compensate for differential probabilities of selection at each sampling stage and adjust for the effects of non-response.17 All analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
At each wave (kindergarten, 3rd, 5th and 8th grades), children in a food-insecure vs food-secure household were more likely to be NHB, Hispanic or Asian/other, uninsured, born with low birthweight, to live in poverty, have mothers born outside of the USA or with a lower education level and have parents ever depressed (Table 1). Across waves, food-secure children consistently had on average 0.1 affirmed items in the 18-item HFSSM, whereas food-insecure children had 5.4–6.4 affirmed survey items. The HFSSM scores between any two waves were moderately correlated, with coefficients ranging from 0.35 to 0.50; 57%, 22%, 16% and 5% of children were exposed to cumulatively one to four FIS episodes, respectively (data not shown).
Table 1.
Parental and child characteristics by household food-security status at each study wave, the Early Childhood Longitudinal Study–Kindergarten Cohort (1999–2007)
| Kindergarten (1999) |
3rd grade (2002) |
5th grade (2004) |
8th grade (2007) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Food-secure (n = 5910) | Food-insecure (n = 458) | P a | Food-secure (n = 6021) | Food-insecure (n = 347) | P a | Food-secure (n = 5899) | Food-insecure (n = 469) | P a | Food-secure (n = 5911) | Food-insecure (n = 457) | P a | |
| Household food-security survey module score,b mean ± SD | 0.1 ± 0.4 | 5.4 ± 2.5 | <0.001 | 0.1 ± 0.3 | 5.8 ± 2.7 | <0.001 | 0.1 ± 0.3 | 5.9 ± 2.9 | <0.001 | 0.1 ± 0.3 | 6.4 ± 3.0 | <0.001 |
| Child characteristics | ||||||||||||
| Male, n (%) | 2900 (49.1) | 236 (51.5) | 0.31 | 2955 (49.1) | 181 (52.2) | 0.26 | 2888 (49.0) | 248 (52.9) | 0.1 | 2901 (49.1) | 235 (51.4) | 0.33 |
| Race/ethnicity, n (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Non-Hispanic White | 4122 (69.7) | 179 (39.1) | 4164 (69.2) | 137 (39.5) | 4109 (69.7) | 192 (40.9) | 4093 (69.2) | 208 (45.5) | ||||
| Non-Hispanic Black | 446 (7.5) | 57 (12.4) | 450 (7.5) | 53 (15.3) | 435 (7.4) | 68 (14.5) | 417 (7.1) | 86 (18.8) | ||||
| Hispanic | 833 (14.1) | 156 (34.1) | 880 (14.6) | 109 (31.4) | 828 (14.0) | 161 (34.3) | 875 (14.8) | 114 (24.9) | ||||
| Asian/other | 509 (8.6) | 66 (14.4) | 527 (8.8) | 48 (13.8) | 527 (8.9) | 48 (10.2) | 526 (8.9) | 49 (10.7) | ||||
| Child uninsured, n (%) | 639 (10.8) | 111 (24.2) | <0.001 | 656 (10.9) | 94 (27.1) | <0.001 | 629 (10.7) | 121 (25.8) | <0.001 | 647 (10.9) | 103 (22.5) | <0.001 |
| Birthweight categories, n (%) | 0.012 | 0.0096 | 0.0003 | 0.074 | ||||||||
| <2500 (low), n (%) | 361 (6.1) | 44 (9.6) | 370 (6.1) | 35 (10.1) | 355 (6.0) | 50 (10.7) | 365 (6.2) | 40 (8.8) | ||||
| 2500–3999 (normal), n (%) | 4783 (80.9) | 354 (77.3) | 4863 (80.8) | 274 (79.0) | 4770 (80.9) | 367 (78.3) | 4773 (80.7) | 364 (79.6) | ||||
| ≥4000 (high), n (%) | 766 (13.0) | 60 (13.1) | 788 (13.1) | 38 (11.0) | 774 (13.1) | 52 (11.1) | 773 (13.1) | 53 (11.6) | ||||
| BMIZ at kindergarten, mean ± SD | 0.4 ± 1.1 | 0.5 ± 1.1 | 0.072 | 0.4 ± 1.1 | 0.5 ± 1.1 | 0.0013 | 0.4 ± 1.1 | 0.6 ± 1.1 | 0.0012 | 0.4 ± 1.1 | 0.6 ± 1.1 | <0.001 |
| BMIZ at 3rd grade, mean ± SD | 0.5 ± 1.1 | 0.7 ± 1.1 | 0.0003 | 0.5 ± 1.1 | 0.7 ± 1.1 | <0.001 | 0.5 ± 1.1 | 0.7 ± 1.1 | <0.001 | 0.5 ± 1.1 | 0.7 ± 1.1 | 0.0001 |
| BMIZ at 5th grade, mean ± SD | 0.6 ± 1.1 | 0.7 ± 1.5 | <0.001 | 0.6 ± 1.1 | 0.8 ± 1.6 | <0.001 | 0.6 ± 1.1 | 0.9 ± 1.1 | <0.001 | 0.6 ± 1.1 | 0.9 ± 1.5 | <0.001 |
| BMIZ at 8th grade, mean ± SD | 0.5 ± 1.1 | 0.8 ± 1.0 | <0.001 | 0.5 ± 1.1 | 0.9 ± 1.0 | 0.5 ± 1.1 | 0.9 ± 1.0 | <0.001 | 0.5 ± 1.1 | 0.9 ± 1.0 | <0.001 | |
| Parental characteristics | ||||||||||||
| Household poverty (below threshold), n (%) | 1141 (19.3) | 289 (63.1) | <0.001 | 1179 (19.6) | 251 (72.3) | <0.001 | 1099 (18.6) | 331 (70.6) | <0.001 | 1115 (18.9) | 315 (68.9) | <0.001 |
| Nativity (foreign-born), n (%) | 923 (15.6) | 153 (33.4) | <0.001 | 973 (16.2) | 103 (29.7) | <0.001 | 910 (15.4) | 166 (35.4) | <0.001 | 978 (16.5) | 98 (21.4) | 0.0071 |
| Maternal education, n (%) | <0.001 | <0.001 | <0.001 | <0.001 | ||||||||
| Less than high school | 451 (7.6) | 139 (30.3) | 489 (8.1) | 101 (29.1) | 456 (7.7) | 134 (28.6) | 482 (8.2) | 108 (23.6) | ||||
| High-school diploma or equivalent | 1830 (31.0) | 198 (43.2) | 1882 (31.3) | 146 (42.1) | 1838 (31.2) | 190 (40.5) | 1831 (31.0) | 197 (43.1) | ||||
| Any college or higher | 3629 (61.4) | 121 (26.4) | 3650 (60.6) | 100 (28.8) | 3605 (61.1) | 145 (30.9) | 3598 (60.9) | 152 (33.3) | ||||
| Parental depression (ever), n (%) | 1546 (26.2) | 275 (60.0) | <0.001 | 1583 (26.3) | 238 (68.6) | <0.001 | 1530 (25.9) | 291 (62.0) | <0.001 | 1531 (25.9) | 290 (63.5) | <0.001 |
BMIZ, body mass index-for-age z-score. Values are unweighted means ± SDs for continuous variables or n (%) for categorical variables.
P-value was obtained by Student’s t-test for continuous variables and Chi-square test for categorical variables.
Raw score obtained by the 18-item US Household Food Security Survey Module (range: 0–18).
Among 6368 children, 206 (3.2%), 123 (2.04%), 124 (2.06%) and 153 (2.40%) were underweight and 1633 (25.7%), 2015 (33.5%), 2240 (37.3%) and 2151 (33.8%) were overweight/obese in kindergarten, 3rd, 5th and 8th grades, respectively (Supplementary Table 1, available as Supplementary data at IJE online). Across study waves, the mean age- and sex-specific body mass index (BMI) percentiles ranged from 1.5–2.3, 50.1–52.5 and 93.4–94.4 among the underweight, normal-weight and overweight/obese, respectively. To address whether weight co-varied with height during the study years when we might expect a linear growth spurt in rapidly growing children, we examined height across BMI categories. Across study waves, children who were underweight were consistently shorter than their normal-weight or overweight/obese counterparts, with three exceptions: the occasion of being taller than normal-weight children in kindergarten; that of being similar height to overweight/obese in kindergarten; and that of being similar height to normal-weight in the 3rd grade.
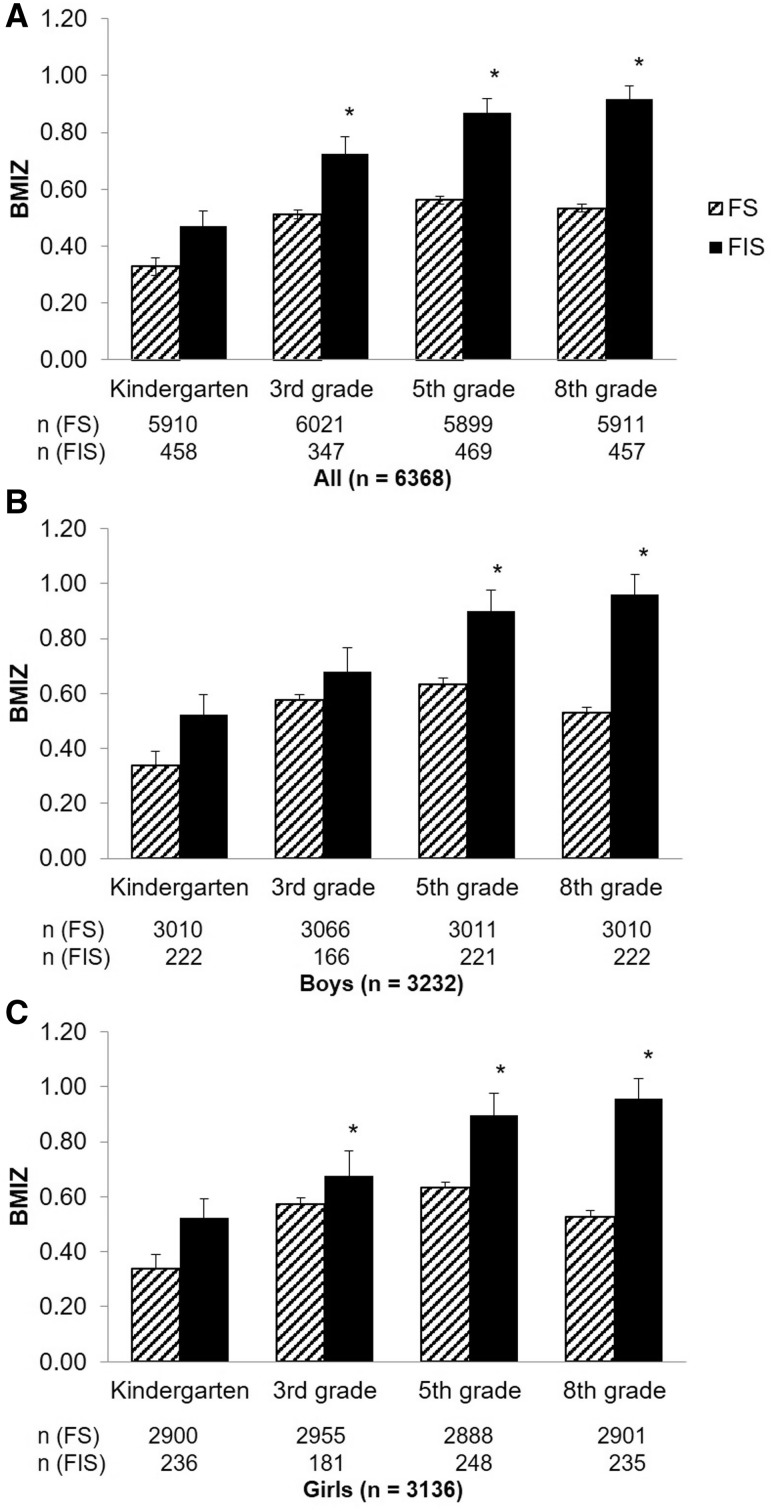
The food-insecure children were consistently heavier and had a higher BMIZ than food-secure children in the 3rd, 5th and 8th grades (Figure 1A). In stratification analysis by sex, food-insecure girls had a higher mean BMIZ than the food-secure girls in the 3rd, 5th and 8th grades; food-insecure boys had a higher mean BMIZ than food-secure boys in the 5th and 8th grades (Figure 1B and C).
Figure 1.
Mean BMI-for-age z-score trajectory by household food-insecurity status at each study wave among all (A), boys (B) and girls (C). BMIZ, body mass index-for age z-score; FS, food security; FIS, food insecurity. *P-value <0.05 after Bonferroni adjustment for multiple comparisons within each panel (i.e. A, B or C).
Table 2 displays adjusted β values for BMIZ at each wave by FIS status. Compared with children in food-secure households, children exposed to FIS in the 5th grade had 0.19 (95% CI: 0.07–0.30) standard deviation (SD) higher BMIZ in the 5th grade; the impact of the FIS exposure in the 5th grade persisted until the 8th grade with 0.17 (0.06–0.27) SD higher BMIZ, regardless of the FIS status at previous study waves. Similarly, children in food-insecure households in 8th grade had 0.29 (95% CI: 0.19–0.40) SD higher BMIZ than their food-secure counterparts. In the 3rd, 5th and 8th grades, NHB and Hispanic children had higher BMIZ than NHWs; Asian/other children had higher BMIZ than NHWs in the 5th and 8th grades (Supplementary Table 2, available as Supplementary data at IJE online). At each wave, low birthweight was associated with lower BMIZ (β range: –0.33 to –0.23) and high birthweight was associated with higher BMIZ scores (β range: 0.35–0.47). Being uninsured vs insured in kindergarten was associated with 0.12 (0.04–0.09) SD higher BMIZ in the 8th grade. Girls had higher BMIZ than boys in the 5th grade but not at other waves. Having a mother born outside of vs in the USA was associated with lower BMIZs in the 3rd, 5th and 8th grades (β range: –0.17 to –0.13). Lastly, mother's education of some college or higher was associated with lower BMIZs in the 3rd, 5th and 8th grades (β range: –0.26 to –0.16).
Table 2.
Adjusted beta (95% CIs) of body mass index-for-age z-score in kindergarten, 3rd, 5th and 8th grade years in relation to food insecurity at the current and previous study waves, the Early Childhood Longitudinal Study–Kindergarten Cohort (1998–2007)a
| Kindergarten (n = 6351) | 3rd grade (n = 6021) | 5th grade (n = 6009) | 8th grade (n = 6368) | |
|---|---|---|---|---|
| Food insecurity in kindergarten | –0.04 (–0.14, 0.06) | 0.04 (–0.07, 0.15) | –0.13 (–0.24, –0.01)b | –0.08 (–0.18, 0.03) |
| Food insecurity in 3rd grade | 0.02 (–0.11, 0.14) | 0.11 (–0.02, 0.23) | –0.07 (–0.19, 0.05) | |
| Food insecurity in 5th grade | 0.19 (0.07, 0.30)c | 0.17 (0.06, 0.27)c | ||
| Food insecurity in 8th grade | 0.29 (0.19, 0.40)c |
Point estimates for each factor were adjusted for child’s race/ethnicity, birthweight, health-insurance status, sex, household poverty, maternal nativity, maternal education and parental depression. Sample sizes for regression models at each study wave were slightly different due to missing data on childhood anthropometric measures.
P-value was attenuated and became >0.05 and remained <0.05, after Bonferroni adjustment for multiple comparisons, respectively.
Adjusted RR and 95% CIs of overweight/obesity at each wave appear in Table 3. Compared with food-secure children at the same wave, food-insecure children had a 27% (95% CI: 1.07–1.51), 21% (1.08–1.35) and 28% (1.07–1.53) higher risk of overweight/obesity in the 3rd, 5th and 8th grades, respectively, while adjusting for FIS at prior wave(s) and covariates. Among all the covariates, high birthweight was consistently associated with a higher risk of overweight/obesity across all study waves (adjusted RR ranging from 1.34 to 1.51; Supplementary Table 3, available as Supplementary data at IJE online). Similarly to the pattern observed for FIS and BMIZ, racial/ethnic minority groups compared with NHWs have 25%–40% greater risk of overweight/obesity across study waves. Girls compared with boys had a 14% lower risk for overweight/obesity in the 5th grade only (adjusted RR 0.86; 95% CI: 0.78–0.94).
Table 3.
Multinomial adjusted RRs (95% CIs) of overweight/obesity in the kindergarten, 3rd, 5th and 8th grade years in relation to food insecurity at the current and previous study waves, the Early Childhood Longitudinal Study–Kindergarten Cohort (1998–2007)a
| Kindergarten | 3rd grade | 5th grade | 8th grade | |
|---|---|---|---|---|
| N (overweight/obesity)/N (total) | 1633/6351 | 2015/6021 | 2240/6009 | 2151/6368 |
| Food insecurity in kindergarten | 0.77 (0.60, 0.98)b | 0.92 (0.74, 1.14) | 0.97 (0.82, 1.15) | 0.94 (0.79, 1.13) |
| Food insecurity in 3rd grade | 1.27 (1.07, 1.51)c | 1.07 (0.89, 1.28) | 1.00 (0.82, 1.22) | |
| Food insecurity in 5th grade | 1.21 (1.08, 1.35)c | 1.16 (0.96, 1.39) | ||
| Food insecurity in 8th grade | 1.28 (1.07, 1.53)c |
Point estimates for each factor were adjusted for child’s race/ethnicity, birthweight, health-insurance status, sex, household poverty, maternal nativity, maternal education and parental depression. The reference group was normal-weight (5th percentile ≤ BMIZ < 85th percentile) children at the respective study wave. Sample sizes for regression models at each study wave were slightly different due to missing data on childhood anthropometric measures.
P-value was attenuated and became >0.05 and remained <0.05, after Bonferroni adjustment for multiple comparisons, respectively.
In contrast to the time-specific association of FIS with overweight/obesity, the risk of underweight in the 8th grade was close to three-fold higher for those with FIS in kindergarten (adjusted RR: 2.76, 95% CI: 1.22–6.25), independently of FIS at other waves (Table 4). High birthweight was associated with a lower risk of underweight in kindergarten (adjusted RR: 0.28; 95% CI: 0.13–0.60), 3rd (0.08; 0.02–0.36) and 5th (0.28; 0.11–0.72) grades (Supplementary Table 4, available as Supplementary data at IJE online). Other associations of household FIS status and covariates with underweight did not persist after Bonferroni adjustment for multiple comparisons.
Table 4.
Multinomial adjusted RRs (95% CIs) of underweight in the kindergarten, 3rd, 5th and 8th grade years in relation to food insecurity at the current and previous study waves, the Early Childhood Longitudinal Study–Kindergarten Cohort (1998–2007)a
| Kindergarten | 3rd grade | 5th grade | 8th grade | |
|---|---|---|---|---|
| N (underweight)/N (total) | 206/6351 | 123/6021 | 124/6009 | 153/6368 |
| Food insecurity in kindergarten | 0.77 (0.34, 1.74) | 1.62 (0.47, 5.60) | 2.41 (1.08, 5.40)b | 2.76 (1.22, 6.25)c |
| Food insecurity in 3rd grade | 1.15 (0.23, 5.86) | 0.52 (0.08, 3.34) | 2.22 (0.56, 8.85) | |
| Food insecurity in 5th grade | 1.19 (0.32, 4.38) | 1.49 (0.38, 5.93) | ||
| Food insecurity in 8th grade | 1.11 (1.03, 1.20)b |
Point estimates for each factor were adjusted for child’s race/ethnicity, birthweight, health-insurance status, sex, household poverty, maternal nativity, maternal education and parental depression. The reference group was normal-weight (5th percentile ≤ BMIZ < 85th percentile) children at the respective study wave. Sample sizes for regression models at each study wave were slightly different due to missing data on childhood anthropometric measures.
P-value was attenuated and became >0.05 and remained <0.05, after Bonferroni adjustment for multiple comparisons, respectively.
Discussion
In this longitudinal cohort of school-aged children, children exposed to household FIS had a higher BMIZ than the food-secure in the 3rd, 5th and 8th grades, when compared cross-sectionally. When FIS exposures at the current and prior waves were assessed simultaneously, proximal exposure to household FIS was associated with a higher risk of overweight/obesity after adjustment for covariates. In contrast, a single, early exposure to FIS reported in kindergarten was associated with a higher risk of underweight in the 8th grade, independently of FIS exposures at subsequent waves.
Given the relatively small number of underweight children across waves (range: 123–206), future investigation with a larger sample size is warranted to confirm our findings. To assess whether the underweight were taller, possibly illustrative of a linear growth spurt, than the normal and overweight/obese, we compared the mean height across the BMIZ categories across study waves. The underweight were overall shorter than the normal and overweight. The age- and sex-specific BMI percentiles among the underweight ranged from 1.5–2.3 across waves—clearly not close to the cut-off of the 5th percentile and, thus, indicating concern for the extreme weight in this group.
To our knowledge, this is the first study to examine the relationship between time-specific, longitudinal exposures to FIS in early to mid-childhood and risk of overweight/obesity and underweight in the USA. Notably, between-wave correlation coefficients of FIS survey scores were moderate (ranging from 0.35 to 0.50), suggesting the temporal variation in FIS exposures and highlighting the importance of examining the time-specific FIS–weight status associations during childhood. Similar to the inconsistent findings from other studies on childhood FIS and weight, previous investigations revealed conflicting associations between FIS and overweight/obesity in the ECLS-K. In a cross-sectional analysis in the fall of kindergarten, no significant association was observed for FIS with overweight, underweight or height-for-age.12 In contrast, a cross-sectional analysis from the spring of kindergarten revealed food-insecure children had lower odds for overweight than food-secure children.13 In an analysis of two waves of the ECLS-K, girls, but not boys, who experienced FIS in kindergarten gained more weight and had higher BMIs in the 3rd grade.14 However, another analysis using two waves of ECLS-K data found an inverse association of FIS in both the spring of kindergarten and 3rd grade with BMI in the 3rd grade.13 Some reported that FIS was not a significant predictor of childhood BMI, whereas others reported significant yet minimal differences in BMI growth (a term coined by the authors) between children in food-secure vs food-insecure households.15,16 The inconsistent findings could be attributed to failure to account for longitudinal exposure to FIS episodes across the waves, apply study sampling weights and examine both ends of childhood weight extremes (underweight and overweight/obese). Indeed, the previous approach to combining underweight and normal-weight children as the reference group may have resulted in missed opportunities to identify potential associations between FIS and weight extremes.
Our study extends the literature by revealing a positive association between an early exposure to FIS in kindergarten with a higher risk of underweight in the 8th grade. Despite a decreasing trend of underweight among children in the past few decades in the USA, this weight extreme was still observed in 3%–7% of children and adolescents aged 2–19 years in 2007–2008.6 Previous data on FIS and underweight among children in high-income countries are scarce; however, data among low- to middle-income countries share certain similar patterns to those observed herein. Household FIS has been linked to underweight, but not overweight/obesity, among both preschool and school-aged children in countries such as Colombia, Bangladesh, Ethiopia and Vietnam.25–27 In contrast, we found that positive associations of FIS with risk of underweight and overweight/obesity coexisted in this USA-representative sample of children. Although the reasons underlying the differential associations between FIS and weight extremes in high- vs low- to middle-income countries remain to be elucidated, national economic levels may serve as an effect modifier, as illustrated by previous reviews and meta-analyses on FIS and risk of weight extremes and type 2 diabetes among adults.28,29
Several mechanisms have been posited to drive the FIS–obesity relationship, including cyclic fasting and overconsumption related to fluctuations in food availability, overconsumption of energy-dense cheaper foods as a means of saving money and stress-related metabolic or behavioural coping mechanisms.30,31 These factors might have contributed to a positive association between proximal exposure to FIS and risk of overweight/obesity at each study wave. On the other hand, FIS has been associated with fewer total calories,32 disrupted eating patterns33 and iron-deficiency anemia,34 which in turn have been linked to negative health consequences. This set of factors may contribute to the risk of undernutrition, i.e. underweight, as observed in the long-lasting association between an early FIS exposure in kindergarten and risk of underweight in the 8th grade. Whereas the mechanisms underlying the different time-specific patterns of FIS exposure and risk of weight extremes remain unknown, future investigations would benefit from longitudinal data collection on dietary intakes, behavioural coping mechanisms and parenting strategies.
The strengths of this study include: a longitudinal, repeated-measures design utilizing data on a large, diverse and stable cohort; the use of the validated HFSSM to measure household FS across waves; and oversampling of ethnic minorities. The observed prevalence of FIS exposure in these analyses was comparable to national data.35 Some limitations of the study merit discussion. We were limited by the absence of maternal characteristics, such as parental feeding behaviours and coping strategies, which might be associated with residual confounding.36,37 We did not have data on children’s dietary intakes, which, however, may be potential mediators and inclusion in the multivariable models may introduce over-adjustment. Finally, we have data on household-level, not child-level, FIS.
In conclusion, there was double burden of household FIS on risk of childhood weight extremes characterized by coexistence of a higher risk of both underweight and overweight/obesity in this longitudinal cohort of school-aged children in the USA. Further, the associations between household FIS and risk of childhood weight extremes exhibited different time-specific patterns. We observed a positive association between proximal exposure to household FIS and risk of overweight/obesity in the 3rd, 5th and 8th grades, whereas an early exposure to FIS in kindergarten was associated with risk of underweight in the 8th grade. Further longitudinal studies based on larger samples are warranted to confirm our findings and examine the potential association between household FIS with longer-term growth and health consequences.
Funding
This work was partially supported by a research grant from the Eunice Kennedy Shriver National Institute of Child Health and Human Development to the Population Research Center at the University of Texas at Austin (Grant No. P2CHD042849) and a research grant from the National Institute of Diabetes and Digestive and Kidney Diseases (Grant No. K01DK120807) to Y.Z.
Supplementary Material
Acknowledgements
We thank all the participants and research staff in the Early Childhood Longitudinal Study–Kindergarten Cohort.
Y.Z., L.D.M. and M.R.F. contributed substantially to the conception and design of the work. Y.Z. performed the statistical analysis and drafted the manuscript along with L.D.M. and M.R.F. L.D.M., M.D.H. and M.R.F. contributed to the interpretation of data in the manuscript and revised the manuscript. All authors approved the final version of the manuscript. Y.Z. and M.R.F. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Conflict of interest: None declared.
References
- 1. Ogden CL, Carroll MD, Kit BK, Flegal KM.. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA 2012;307:483–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ogden CL, Flegal KM, Carroll MD, Johnson CL.. Prevalence and trends in overweight among us children and adolescents, 1999-2000. JAMA 2002;288:1728–32. [DOI] [PubMed] [Google Scholar]
- 3. Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH.. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med 1997;337:869–73. [DOI] [PubMed] [Google Scholar]
- 4. Biro FM, Wien M.. Childhood obesity and adult morbidities. Am J Clin Nutr 2010;91:1499S–505S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Becker PJ, Nieman Carney L, Corkins MR. et al. Consensus statement of the academy of nutrition and dietetics/American society for parenteral and enteral nutrition: indicators recommended for the identification and documentation of pediatric malnutrition (undernutrition). J Acad Nutr Diet 2014;114:1988–2000. [DOI] [PubMed] [Google Scholar]
- 6. Fryar CD, Ogden CL. Prevalence of Underweight among Children and Adolescents Aged 2–19 Years: United States, 1963–1965 through 2011–2012. 2012. https://www.cdc.gov/nchs/data/hestat/underweight_child_07_10/underweight_child_07_10.pdf (15 October 2018, date last accessed)
- 7. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A.. Household Food Security in the United States in 2018 Washington, DC: US Department of Agriculture Economic Research Service—Economic Research Report, 2019.
- 8. Eisenmann JC, Gundersen C, Lohman BJ, Garasky S, Stewart SD.. Is food insecurity related to overweight and obesity in children and adolescents? A summary of studies, 1995-2009. Obes Rev 2011;12:e73–83. [DOI] [PubMed] [Google Scholar]
- 9. Kaur J, Lamb MM, Ogden CL.. The association between food insecurity and obesity in children—the national health and nutrition examination survey. J Acad Nutr Diet 2015;115:751–58. [DOI] [PubMed] [Google Scholar]
- 10. Whitaker RC, Orzol SM.. Obesity among US urban preschool children: relationships to race, ethnicity, and socioeconomic status. Arch Pediatr Adolesc Med 2006;160:578–84. [DOI] [PubMed] [Google Scholar]
- 11. Boone-Heinonen J, Tillotson C, O’Malley J. et al. Characterizing a ‘big data’ cohort of over 200, 000 low-income US infants and children for obesity research: the ADVANCE Early Life Cohort. Matern Child Health J 2017;21:421–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stormer A, Harrison GG.. Does Household Food Security Affect Cognitive and Social Development of Kindergarteners? Discussion Paper No. 1276–03. Madison, WI: Institute for Research on Poverty, 2003. [Google Scholar]
- 13. Rose D, Bodor JN.. Household food insecurity and overweight status in young school children: results from the early childhood longitudinal study. Pediatrics 2006;117:464–73. [DOI] [PubMed] [Google Scholar]
- 14. Jyoti DF, Frongillo EA, Jones SJ.. Food insecurity affects school children's academic performance, weight gain, and social skills. J Nutr 2005;135:2831–39. [DOI] [PubMed] [Google Scholar]
- 15. Bhargava A, Jolliffe D, Howard LL.. Socio-economic, behavioural and environmental factors predicted body weights and household food insecurity scores in the Early Childhood Longitudinal Study-Kindergarten. Br J Nutr 2008;100:438–44. [DOI] [PubMed] [Google Scholar]
- 16. Burke MP, Frongillo EA, Jones SJ, Bell BB, Hartline-Grafton H.. Household food insecurity is associated with greater growth in body mass index among female children from kindergarten through eighth grade. J Hunger Environ Nutr 2016;11:227–41. [Google Scholar]
- 17. Tourangeau K, Nord C, Lê T, Sorongon AG, Najarian M.. Early Childhood Longitudinal Study, Kindergarten Class of 1998–99 (ECLS-K): Combined User's Manual for the ECLS-K Eighth-Grade and K-8 Full Sample Data Files and Electronic Codebooks. NCES 2009–004. Washington, DC: National Center for Education Statistics, 2009.
- 18. Mangini LD, Hayward MD, Dong YQ, Forman MR.. Household food insecurity is associated with childhood asthma. J Nutr 2015;145:2756–64. [DOI] [PubMed] [Google Scholar]
- 19. Coleman-Jensen A, Rabbitt MP, Gregory CA, Singh A.. Household Food Security in the United States in 2016 Washington, DC: Report, United States Department of Agriculture, 2017. [Google Scholar]
- 20. Bickel G, Nord M, Price C, Hamilton W, Cook J.. Guide to Measuring Household Food Security, 2000 edn Alexandria, VA: United States Department of Agriculture, 2000. [Google Scholar]
- 21.Centers for Disease Control and Prevention. A SAS Program for the 2000 CDC Growth Charts (Ages 0 to <20 Years) Growth Chart Training 2019, 26 February 2019. https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm (2 July 2019, date last accessed).
- 22. Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics 2007;120:S164–92. [DOI] [PubMed] [Google Scholar]
- 23. Burke MP, Jones SJ, Fram MS, Frongillo EA.. U.S. households with children are exposed to nonpersistent and persistent food insecurity. J Hunger Environ Nutr 2012;7:349–62. [Google Scholar]
- 24. Craney TA, Surles JG.. Model-dependent variance inflation factor cutoff values. Qual Eng 2002;14:391–403. [Google Scholar]
- 25. Ali D, Saha KK, Nguyen PH. et al. Household food insecurity is associated with higher child undernutrition in Bangladesh, Ethiopia, and Vietnam, but the effect is not mediated by child dietary diversity, 2. J Nutr 2013;143:2015–21. [DOI] [PubMed] [Google Scholar]
- 26. Saha KK, Frongillo EA, Alam DS, Arifeen SE, Persson LÅ, Rasmussen KM.. Household food security is associated with growth of infants and young children in rural Bangladesh. Public Health Nutr 2009;12:1556–62. [DOI] [PubMed] [Google Scholar]
- 27. Isanaka S, Mora-Plazas M, Lopez-Arana S, Baylin A, Villamor E.. Food insecurity is highly prevalent and predicts underweight but not overweight in adults and school children from Bogota, Colombia. J Nutr 2007;137:2747–55. [DOI] [PubMed] [Google Scholar]
- 28. Moradi S, Mirzababaei A, Dadfarma A. et al. Food insecurity and adult weight abnormality risk: a systematic review and meta-analysis. Eur J Nutr 2019;58:45–61. [DOI] [PubMed] [Google Scholar]
- 29. Abdurahman AA, Chaka EE, Nedjat S, Dorosty AR, Majdzadeh R.. The association of household food insecurity with the risk of type 2 diabetes mellitus in adults: a systematic review and meta-analysis. Eur J Nutr 2019;58:1341–50. [DOI] [PubMed] [Google Scholar]
- 30. Pan L, Sherry B, Njai R, Blanck HM.. Food insecurity is associated with obesity among US adults in 12 states. J Acad Nutr Diet 2012;112:1403–09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S.. Exploring mediators of food insecurity and obesity: a review of recent literature. J Community Health 2012;37:253–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Casey PH, Szeto K, Lensing S, Bogle M, Weber J.. Children in food-insufficient, low-income families: prevalence, health, and nutrition status. Arch Pediatr Adolesc Med 2001;155:508–14. [DOI] [PubMed] [Google Scholar]
- 33. Kendall A, Olson CM, Frongillo EA.. Relationship of hunger and food insecurity to food availability and consumption. J Am Diet Assoc 1996;96:1019–24. [DOI] [PubMed] [Google Scholar]
- 34. Skalicky A, Meyers AF, Adams WG, Yang Z, Cook JT, Frank DA.. Child food insecurity and iron deficiency anemia in low-income infants and toddlers in the United States. Matern Child Health J 2006;10:177–85. [DOI] [PubMed] [Google Scholar]
- 35. Wilde PE, Nord M, Zager RE.. In longitudinal data from the survey of program dynamics, 16.9% of the U.S. population was exposed to household food insecurity in a 5-year period. J Hunger Environ Nutr 2010;5:380–98. [Google Scholar]
- 36. Metallinos-Katsaras E, Must A, Gorman K.. A longitudinal study of food insecurity on obesity in preschool children. J Acad Nutr Diet 2012;112:1949–58. [DOI] [PubMed] [Google Scholar]
- 37. Kursmark M, Weitzman M.. Recent findings concerning childhood food insecurity. Curr Opin Clin Nutr Metab Care 2009;12:310–16. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.