HIGHLIGHTS
-
•
Does peer companionship delivered by an aging services agency to socially disconnected older adult primary care patients result in improvement in suicidal ideation, depression, anxiety, and psychological connectedness?
-
•
Older adults who received the peer companionship intervention had greater improvement in symptoms of depression, anxiety, and feelings of being a burden on others than those who did not have a peer companion. Levels of suicidal ideation and feelings of belonging improved in both groups.
-
•
By improving social connectedness, peer companionship as delivered by community-based social services can contribute to the mental health and well-being of older adults.
Key Words: Anxiety, depression, loneliness, peer companionship, social connectedness, suicidal ideation
Abstract
Objectives
To determine whether peer companionship delivered by an aging services agency to socially-disconnected older adult primary care patients was associated with improvement in suicidal ideation depression, anxiety, and psychological connectedness.
Design
Pragmatic, nonblinded, parallel-group, randomized controlled trial comparing peer companionship, The Senior Connection (TSC), to care-as-usual (CAU).
Setting
Lifespan, a nonmedical, community-based aging services agency.
Participants
Adult primary care patients ages 60 years or older who endorsed feelings of loneliness or being a burden on others.
Intervention
TSC was delivered by Lifespan volunteers who provided supportive visits and phone calls in the subjects’ homes. CAU involved no peer companion assignment.
Measurements
The primary outcome was suicidal ideation assessed by the Geriatric Suicide Ideation Scale; secondary outcomes were depression, anxiety, and feelings of belonging and being a burden on others. Data were collected at baseline, 3-, 6-, and 12-months.
Results
Subjects (55% female) had a mean age of 71 years. There was no difference between groups in change in suicidal ideation or belonging. Subjects randomized to TSC had greater reduction in depression (PHQ-9; 2.33 point reduction for TSC versus 1.32 for CAU, p = 0.05), anxiety (GAD-7; TSC 1.52 versus CAU 0.28, p = 0.03), and perceived burden on others (INQ; 0.46 TSC versus 0.09 CAU, p <0.01).
Conclusions
TSC was superior to CAU for improving depression, anxiety, and perceived burden, but not suicidal ideation. Although effect sizes were small, the low-cost and nationwide availability of peer companionship justify further examination of its effectiveness and scalability in improving mental health outcomes of socially disconnected older adults.
OBJECTIVE
Social connectedness refers to structural, functional, and qualitative aspects of relationships that social scientists regard as essential to a healthy life.1 Structural connectedness includes characteristics of social ties and networks that when insufficient may cause social isolation. Functional connectedness includes aspects of relationships that provide support, such as emotional or instrumental support, as well as subjective feelings of loneliness or that one does not belong. Qualitative aspects of connectedness include relationship quality or marital discord. Disruptions in social connections are common in older age. From 20 to over 40% of adults ages 60 years or older report frequent or intense loneliness,2 and older adults who are socially disconnected carry increased risk for reduced quality of life,3 phsyical illness,4 , 5 and death.2 , 6 , 7 Mortality risk related to social disconnection is at least as large as that arising from obesity, physical inactivity, alcohol misuse, and smoking.8
Loneliness is also associated with dementia, anxiety, and depression,3 , 9 and with suicidal behavior both on theoretical10 and empirical bases.11 Case control studies have found significant relationships between suicide and indicators of social disconnection including family discord,12 , 13 insufficient social supports,14 and disengagement from social activities in the second half of life.14 , 15 As the population of older adults grows, so too will the number living in isolation, experiencing loneliness, and dying by suicide. The demography of aging combined with the prevalence and negative outcomes associated with social disconnectedness in older people make it a pressing public health concern.2 , 16 , 17
Social connectedness is increasingly recognized as a potential means to achieve better health outcomes at lower cost.1 , 18 Older adults, including those at risk for suicide, often visit their primary care providers. However, healthcare settings lack capacity to assess and treat social disconnectedness. Nonmedical aging services providers, while well-equipped to address social determinants of health, are rarely well integrated partners in healthcare delivery.
The U.S. Aging Services Network (ASN) is a national network of community-based social service agencies overseen by the Administration on Aging established by the Older Americans Act in 1965 to ensure that adults 60 years or older have the services necessary to maintain independence. It comprises 56 State Agencies on Aging, 622 Area Agencies on Aging, and more than 260 Title VI Native American aging programs delivering services to millions of U.S. older adults.19 Peer companionship is a service regularly offered by ASN agencies to provide supportive relationships for their socially isolated clients. Other peer-based interventions provided outside the ASN include befriending and peer mentoring, which can vary considerably in their objectives, mode of delivery, and services provided.20 , 21 How “peer” is defined also varies across programs and studies.
A meta-analysis of randomized controlled trials that examined effectiveness of peer companion or befriending interventions on depressive symptoms in a variety of groups across the adult age range found modest but significant reductions relative to comparator conditions.21 A second more recent meta-analysis, however, found no specific benefit of peer companion interventions on depression or loneliness, concluding that current evidence does not allow for firm conclusions on their use.20 No studies have focused on suicide-related outcomes. Neither have studies to date specifically examined peer companionship administered to primary care patients by ASN agencies, which arguably offer the greatest scalability and potential impact.
Our premises are that ASN agencies represent an untapped resource for the detection and management of social disconnectedness, and that given the close associations between social connections and both physical and mental health, ASN-based peer companion interventions should be assessed for their impact on older adult health and suicide prevention. With this study we sought to test the hypothesis that a peer-companion intervention offered by, and typical of, ASN agency programming called The Senior Connection (TSC) would result in greater improvement in outcomes associated with risk for suicide in later life for older adults reporting loneliness or feeling like a burden – suicidal ideation, perceived burden and low belonging (forms of social disconnection posited to increase risk for suicide by the Interpersonal Theory of Suicide10), and symptoms of anxiety, and depression – than in a comparison group of older adults who received no peer-companion intervention. Second, we sought to lay a foundation for subsequent studies of integrated care management that links primary care with ASN agencies by testing the TSC intervention with socially disconnected older adults from primary care practices.
METHODS
Study Design
Details of the TSC trial protocol have been published elsewhere.22 The study was a nonblinded, parallel-group, randomized controlled trial conducted with community-dwelling older adults in Western New York State. Subjects were recruited from primary care practices. The experimental intervention (TSC) was administered and delivered by the region's largest non-medical aging services provider, Lifespan.23
Setting and Participants
Information letters to primary care practice patients introduced the study as “trying to understand the effect of social connections on health in later life (and) seeking adult volunteers who experience feelings of loneliness or of feeling like a burden on others.” Interested individuals completed preliminary phone screens that yielded 427 in-person baseline interviews to assess eligibility. Inclusion criteria were age 60 years or older, English speaking, residing in the community (residents of long-term care facilities were not eligible), able to provide informed consent, and endorsing loneliness (“I feel lonely”) or perceived burdensomeness (“I feel like a burden on others”) in the previous 2 weeks. Exclusion criteria were cognitive impairment (Mini-Cog24 score of ≤3) and alcohol abuse (AUDIT-C25 score of ≥5). To increase the relevance of the study to community-based primary care, symptoms of depression, anxiety, and suicidal ideation without imminent risk were neither inclusion nor exclusion criteria.
Randomization and Masking
Prior to randomization an in-home assessment, routine for Lifespan, was conducted to ensure that subjects’ safety needs were being met and, if assigned to TSC, that it was safe for volunteers to enter the home. Subjects were then randomized to receive TSC or care-as-usual (CAU). Randomization was stratified by gender based on the urn randomization model26 using a sequence generated by the chief biostatistician (XT). The research assessor informed subjects of their group assignment following confirmation of eligibility by random selection of a sealed envelope indicating TSC or CAU. Neither research assessors nor subjects were masked to group assignment.
Procedures
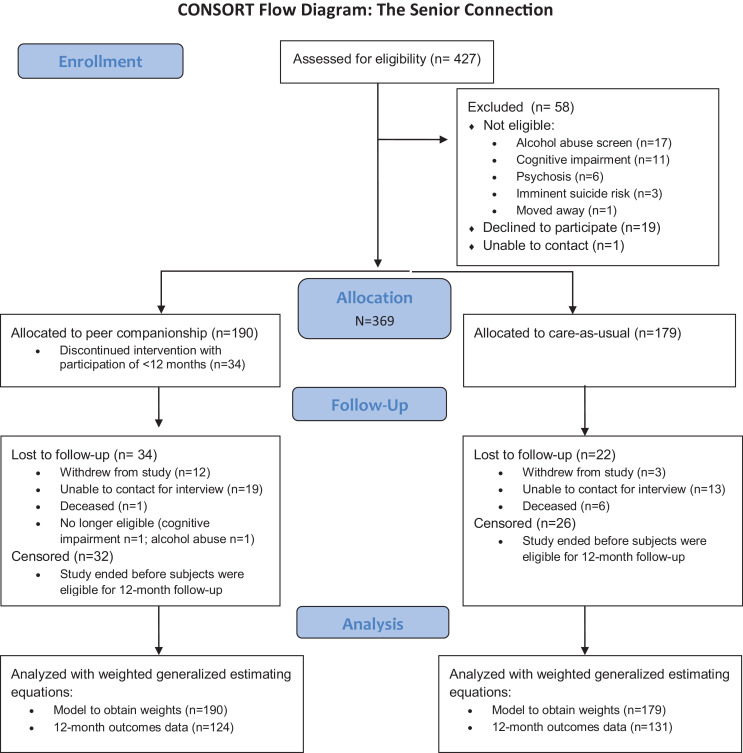
Patients were recruited from primary care clinics from March 2011 to September 2015. Three hundred and sixty-nine subjects were randomized (38 met exclusion criteria, 1 was unable to be contacted, and 19 declined to participate) and constitute our sample for analysis (Fig. 1 ). Peer relationships take several months to establish as they require screening, recruitment and training of a suitably matched volunteer, and time for the matched pair to settle on their preferred pattern of interactions. Original plans were for outcome assessments at 12 and 24 months. However, the pace of recruitment was slowed by demands on our ASN partner agency to identify the volunteers needed. Consequently, there were very less with 24-month data to allow meaningful analysis and, when support for the study ended, our pool of subjects enrolled with enough time to provide 12-month outcomes data was reduced to 313, of which 255 randomized subjects provided 12-month assessments (TSC = 124 and CAU = 131). All reasons for missing data on outcomes at 12-months, including attrition and administrative censoring (due to study closing prior to 12 months of participation), were accounted for as explained further below using weighted generalized estimating equations (WGEE) that included all 369 randomized subjects in the analytic model to create weightings.
FIGURE 1.
Consort flow diagram.
The University of Rochester Research Subjects Review Board approved all procedures and subjects provided written informed consent.
Intervention – TSC
TSC is a standardized version of a volunteer-based peer companionship program delivered by Lifespan, the largest ASN agency in the Monroe County, NY region23 designed to address the companionship needs of older adults who report loneliness or feeling like a burden on others, without a requirement of homebound status.
Each subject assigned to TSC was matched with a “peer companion” recruited by Lifespan through its affiliated Retired and Senior Volunteers Program (RSVP).27 Funded by the Corporation for National and Community Service, RSVP matches adults 55 years or older across the United States with volunteer opportunities. For TSC the volunteer companions received manualized training that addressed the program's mission, objectives, and policies and procedures, and instructed volunteers in techniques for connecting with a diverse population of older adults (e.g., active listening skills, accommodations for sensory deficits).
Peer companions were assigned to TSC subjects based on Lifespan's standard practices, which consider geographical proximity, shared interests, and preferences when possible to accommodate. Peer companions were instructed to provide friendly visiting rather than instrumental support such as house chores that had no interpersonal component. Contacts were prescribed four times per month, to include at least two in-person visits; the other contacts could be phone calls. Electronic communications (email, texting) were allowed but not regarded as meeting the expectations for contact.
Comparison Condition – CAU
The comparison CAU condition entailed no engagement with Lifespan or its peer companionship program during the follow-up period. Medical or psychiatric interventions were not restricted; neither were other informal social support or social services interventions.
Baseline and Follow-up Assessments
Subjects in both conditions were assessed at baseline in their homes. Follow-up assessments were conducted by telephone 3 and 6 months after randomization and by a final in-person interview at 12 months.
Outcomes
The primary outcome was severity of suicidal ideation as measured by a continuous total score on the Geriatric Suicide Ideation Scale (GSIS).28 We had four secondary outcomes: depressive symptoms (Patient Health Questionnaire-9 item, total score; PHQ-9),29 anxiety symptoms (Generalized Anxiety Disorder-7 item, total score; GAD-7),30 and feelings of belonging and burdensomeness (score of subscales of the Interpersonal Needs Questionnaire: INQ-Belong, which includes loneliness, and INQ-Burden).31
Covariates were the number of instrumental activities of daily living for which assistance was required (Instrumental Activities of Daily Living scale; IADL),32 lifetime history of a suicide attempt (Paykel Suicide Scale; PSS)33 and severity of feeling like a burden at baseline (INQ-Burden) as these were imbalanced across the groups at baseline and are strong predictors of our outcomes. Age was also a covariate.
Power Analysis
We conducted an a priori power analysis to determine the minimum effect size we could detect in our statistical model given our planned sample size of 400 with 20% attrition. We estimated detectable effect sizes with which to achieve 80% power based on a two-sided type I alpha = 0.05 under three scenarios regarding magnitudes of within-subject correlations. Depending on real within-subject correlations in the outcome, the detectable effect size varied from 0.151 to 0.206 for 1-year, all within the range of small effect size for testing hypotheses.
Statistical Analysis
Of 369 older adults randomized to either TSC (n = 190) or CAU (n = 179), 255 had complete assessments at 12 months. As depicted in Figure 1, the remainder did not provide data at 12 months either because they were lost to follow-up (n = 34 in TSC and n = 22 in CAU) due to death, illness, or study withdrawal for other reasons; or because the study ended before they completed 12 months (administrative censoring) in either TAU (n = 32) or CAU (n = 26). Because these censored subjects were initially randomized, we included them in the intent-to-treat analysis.
In order to account for all sources of missing data (attrition and censoring) and the longitudinal design, we used WGEE as our analytic approach.34 WGEE provides valid inference (i.e., unbiased estimates for the intervention effect) in the presence of missing data by weighting observations based on inverse probability of retention, extending the generalized estimating equations (GEE) from valid inference only under missing completely at random to missing at random (MAR). Weights for use in WGEE models were based on the randomized sample of 369 subjects to ensure valid intent-to-treat models for the 255 subjects with complete12-month outcomes. Statistical models for the outcomes included baseline covariates, time, condition, and time by condition interaction. We first compared the intervention groups of the initial randomized sample of 369 (TSC = 190 and CAU = 179) and variables that differentiated the groups at baseline were included as covariates in all subsequent analyses. Although we are interested in change between baseline and 12-month follow-up, we included the baseline, 3-, and 6-month values of the response along with the covariates and predictors when modeling the weights of WGEE for the outcome at 12 months in order to ensure valid statistical inference in the presence of administrative censoring. While the number of subjects who were not able to provide 12-month outcomes was substantial, the majority of this missing data is due to administrative censoring and not drop-out/attrition. With all 369 subjects in the models for missing data we could account for administrative censoring and complete valid intent-to-treat analyses using all subjects who were randomized.
For each outcome we also ran a model that included sex and the three-way interaction of sex by time by condition to examine whether the intervention was differentially effective for men and women.
Missing data for individual items on the outcome measures and covariates were minimized by use of trained interviewers, interim telephone contacts to sustain engagement, and oral administration of measures. Individual items were missing in three subjects and we used mean imputation for total scores in these instances.
RESULTS
Baseline characteristics are presented in Tables 1 and 2 . The sample was 45% male and the mean age was 71 (range 60–97 years). The majority of the sample was non-Hispanic and white. Approximately a third was married and half lived alone. Subjects had an average of 15 years of education. Over one-third reported that their monthly income was less than US $1,750 per month, or 133% of the U.S. Federal Poverty Level. TSC and CAU groups were balanced with regard to demographics at baseline.
TABLE 1.
Demographic Characteristics of TSC and CAU Samples at Baselinea
| Variable | TSC (n = 190) | CAU (n = 179) | Statistic | p Value |
|---|---|---|---|---|
| Age, mean (SD), years | 70.48 (7.61) | 71.33 (7.91) | t(367) = -1.05 | 0.30 |
| Male | 87 (45.79) | 79 (44.13) | χ2 (368) = 0.10 | 0.75 |
| White | 164 (86.32) | 155 (87.08%) | χ2(367) = 0.05 | 0.83 |
| Hispanic | 2 (1.05) | 3 (1.68) | FTb(368) = 188b | 0.68 |
| Education, mean (SD), years | 14.84 (3.17)b | 14.92 (2.90) | t(366) = -0.24 | 0.81 |
| Income ≤ $1,750/month | 66 (35.48) | 62 (35.03) | χ2(362) = 0.01 | 0.93 |
| Lives alone | 107 (56.32) | 87 (48.60) | χ2(368) = 2.20 | 0.14 |
| Currently married | 69 (36.32) | 61 (34.08) | χ2(368) = 0.20 | 0.65 |
CAU: care as usual; SD: standard deviation; TSC: The Senior Connection intervention.
Data are presented as number (percentage) of participants unless otherwise indicated.
Fisher's Exact Test.
TABLE 2.
Clinical Characteristics of TSC and CAU Samples at Baselinea
| Variable | TSC, n = 190 | CAU, n = 179 | Statistic | p Value |
|---|---|---|---|---|
| PSS suicide attempt itemb | 28 (14.74) | 18 (10.06) | χ2(368) = 1.85 | 0.17 |
| PHQ-9, item 9c | 13 (6.84) | 5 (2.79) | χ2(368) = 3.26 | 0.07 |
| PHQ-9 total scored | 7.28 (4.90) | 6.75 (4.65) | t(367) = 1.06 | 0.29 |
| GAD-7 total scoree | 5.25 (4.62)f | 4.91 (4.31) | t(366) = 0.72 | 0.47 |
| IADL total score g | 1.14 (1.67) | 0.86 (1.48)f | t(366) = 1.71 | 0.09 |
| Lonelinessh | 156 (82%) | 140 (79%) | Z(366)i = 1.36 | 0.17 |
| Perceived burdenh | 59 (31%) | 55 (31%) | Z(366)i = 0.37 | 0.71 |
CAU: care as usual; GAD-7: Generalized Anxiety Disorder, 7-item anxiety symptom scale; PHQ-9: Patient Health Questionnaire, 9-item depression symptoms scale; PSS: Paykel Suicide Scale; TSC: The Senior Connection intervention.
Data are presented as mean (SD) unless otherwise indicated.
ThePaykel Suicide Scale item indicates the number (percentage) in each group that endorsed one or more suicide attempts at any time in their lives.
PHQ-9 item 9 indicates the number (percentage) in each group that endorsed that they would be better off dead or considered hurting themselves in some way at least several days in the last 2 week period.
PHQ-9 is a 9-item measure of depressive symptoms with a range of 0–27; higher total scores indicate greater depression. Moderate severity (scores greater than 10) were reported by 29% in TSC and 23% in CAU.
GAD-7 is a 7-item measure of anxiety symptoms with a range of 0–21; higher total scores indicate greater anxiety. Moderate severity (scores greater than 10) were reported by 16% in TSC and 14% in CAU.
One subject had missing data.
IADLs are measures of instrumental activities of daily living such as shopping, cooking, and using the telephone. Scores represent the number of activities for which assistance is required.
Loneliness was assessed with the item, “In the last 2 weeks, I felt lonely,” and perceived burden with the item, “In the last 2 weeks, I felt like a burden on others.” For both items, a positive response was indicated by reporting “somewhat” or “very true for me,” while a negative response was indicated by “not at all true for me.” Values in the table represent the number and percentage with positive responses. Forty-one percent of participants endorsed both loneliness and perceived burden. Only n = 19 participants endorsed perceived burden but denied loneliness.
Z statistic is for the Cochran-Armitage Trend Test.
Most participants reported only loneliness at baseline (54%) or both loneliness and perceived burden (41%), while 5% reported only perceived burden. The range of PHQ-9 scores was substantial (range 0–21 total scores). The same was true for the GAD-7 anxiety scale, with the full range of scores possible being reported (0–21). Almost 5% reported passive or active suicidal ideation in the past 2 weeks, and 12.5% reported a history of one or more lifetime suicide attempts. The average number of functional impairments reported was 1, but the full range of IADL (0–7) impairments was endorsed.
Peer companions reported an average of one in-person meeting lasting 1.75 hours (range 0–5 meetings; 0–19 hours of visiting time) per month, and two calls lasting, in total, an average of 31 minutes (range 0–6 calls; 0–3.5 hours). They engaged in a diverse array of activities, including having tea/coffee, golfing, dancing, lunches, and phone calls for planning and friendly chats.
The intent-to-treat model for our primary outcome compared TSC and CAU on severity of suicidal ideation (GSIS total score; Table 3 ). Both groups had significantly reduced suicidal ideation, but with no greater change in the peer companionship arm than CAU. Both depression (PHQ-9; ß = 1.01, 95% confidence interval [CI] = −0.02 to 2.05, p = 0.05) and anxiety symptom severity (GAD-7; ß = 1.23, 95% CI = 0.15–0.32, p = 0.03) showed a statistically significant time by condition interaction, with symptom decreases greater for TSC. Mean scores at baseline and 12-month follow-up (Table 3) indicate that TSC subjects evidenced a drop of 2.33 points on the PHQ-9 and 1.55 points on the GAD-7, while CAU subjects evidenced a drop of 1.31 points on the PHQ-9 and 0.27 points on GAD-7. The percentage of subjects with scores classified as “severe” decreased by 9% and 5% for TSC (PHQ-9 and GAD-7, respectively) and 4% and 3% for CAU. Both groups improved on feelings of belonging (i.e., low loneliness), but no more so in the TSC than CAU arm. Results for INQ-Burden, however, showed a statistically significant time by condition interaction indicating greater reduction for TSC than CAU (ß = 0.38, 95% CI = 0.12–0.64, p <0.01).
TABLE 3.
Condition (TSC vs CAU) by Time Interaction in Intent to Treat Analyses for 12-Month Follow-Upa
| Outcome | TSC Mean (SE) |
CAU Mean (SE) |
ß (SE) | p Value | ||
|---|---|---|---|---|---|---|
| Baseline (n = 190) | 12 months (n = 124) | Baseline (n = 179) | 12 months (n = 131) | |||
| GSIS total scoreb | 62.62 (3.12) | 57.51 (3.18) | 61.03 (3.22) | 55.59 (3.37) | −0.34 (1.60) | 0.83 |
| PHQ-9 total scorec | 8.67 (0.91) | 6.34 (0.90) | 8.28 (0.91) | 6.96 (0.94) | 1.01 (0.53) | 0.05 |
| GAD-7 total scored | 8.08 (1.02) | 6.56 (1.02) | 7.86 (1.04) | 7.58 (1.11) | 1.23 (0.55) | 0.03 |
| INQ – Belonginge | 5.27 (0.67) | 3.71 (0.69) | 5.00 (0.68) | 3.38 (0.69) | −0.06 (0.39) | 0.89 |
| INQ – Burdene | 1.65 (0.41) | 1.19 (0.41) | 1.43 (0.42) | 1.34 (0.42) | 0.38 (0.13) | <0.01 |
CAU: care as usual; GAD-7: Generalized Anxiety Disorder, 7-item anxiety symptom scale; GSIS: Geriatric Suicide Ideation Scale; INQ: Interpersonal Needs Questionnaire; PHQ-9: Patient Health Questionnaire, 9-item depression symptoms scale; SE: standard error; TSC: The Senior Connection intervention.
Statistics are provided for the condition by time interaction, which indicates the presence/absence of an effect of peer companionship on outcomes. Means (SE) are adjusted for covariates in the model. Parameter estimates and p values were derived from WGEE analyses with baseline covariates (total instrumental activities of daily living impairments at baseline, presence of suicide ideation on the PHQ-9 at baseline, level of perceived burden at baseline, and lifetime suicide attempt). The variables used to determine weights for the GEE model included: perception of being burden to others, suicide ideation in the past two weeks (thoughts of better off dead or harming oneself on the PHQ-9), number of IADL impairments, and four indicators of recent suicide ideation (active ideation, considering methods, expectancy of future attempt if circumstances worsen, and perception that lack of energy is preventing an attempt) at baseline.
The GSIS total score reflects overall suicidal ideation, with higher scores indicating more frequent and intense suicidal thoughts. Analyses (not shown) were rerun using observations that met the MAR assumption with 3-month and 6-month data in the missing model, reducing the GSIS sample size and yielding similar results.
PHQ-9 is a 9-item measure of depressive symptoms with a range of 0–27; higher total scores indicate greater depression.
GAD-7 is a 7-item measure of anxiety symptoms with a range of 0–21; higher total scores indicate greater anxiety.
The Interpersonal Needs Questionnaire subscales measure lack of belonging (INQ-Belonging) and the respondent's perception of being a burden on others (INQ-Burden). Higher scores indicate greater distress in each interpersonal domain.
Finally, we looked at the sensitivity of the models that included a main effect of sex and a three-way interaction between time, condition, and sex to examine sex as a potential moderator. None of the models produced significant main or moderation effects for sex.
CONCLUSIONS
The COVID-19 pandemic and the “social distancing” it requires serve as reminders of the importance of social connections to health and of the vulnerability of older adults to their loss. TSC is the first rigorous test to our knowledge of a social connectedness intervention for older adults delivered by a community-based aging services agency. Its primary objective was to examine the impact of peer companionship on suicidal ideation and factors that place older adults at risk of becoming suicidal – psychological indices of social connectedness, depression, and anxiety. Older adults with low social connectedness who were assigned a peer companion experienced significantly greater reductions from baseline in symptoms of depression, anxiety, and feelings that they are a burden on others than those who were not. Feelings of belonging increased and suicidal ideation decreased in both TSC and CAU groups, but there was no significant difference between them on either outcome.
Strengths of the design include use of primary care practices for subject recruitment and of Lifespan, an ASN agency comparable to others across the United States, for delivery of the peer companion intervention. ASN providers have the knowledge and skills to optimize independent functioning, quality of life, and social engagement in their clients. They also have established infrastructure for identifying and treating social disconnectedness in seniors nationwide through peer companionship and programs such as Meals-on-Wheels and Senior Nutrition Programs that provide potentially potent social supports in addition to nutrition assistance. Yet programs in the human services sector are rarely integrated with healthcare services. Findings reported here reinforce the potential benefits of engaging ASN providers as partners in integrated healthcare delivery, including for the management of common mental disorders in later life.
Limiting the study, research and Lifespan staff could not feasibly be blinded to condition. Also, the effects observed may reflect the nature of peer companionship received, including the frequency and types of contacts and the duration of exposure, and of characteristics of the peer dyad (e.g., gender, age, race matching, and shared interests). Our ability to explore these dimensions of peer companionship was limited, however. Understanding their influence on outcomes would be of value to RSVP in optimizing the peer companion program's impact, and warrants further research. In practice, however, peer companionship programs experience high degrees of satisfaction by both members of the dyad. Matches often last for years, evolving to close friendships. Our subjects and their companions reported becoming “like members of a family.”
Although the changes we report between groups in feelings of burdensomeness, depression, and anxiety were relatively small, they were both statistically significant and clinically meaningful. The levels of depression and anxiety observed are associated with adverse consequences in older adults, and even small reductions as we found may reduce incident major affective disorders.35 Furthermore, changes in measures of perceived burdensomeness and loneliness on the order of those observed here are clinically meaningful.36 , 37 As a volunteer-delivered intervention, TSC has low implementation costs making wide dissemination more feasible. Even small gains over a large population of socially disconnected older people may have a large cumulative impact on health in later life.
The groups did not differ with regard to changes in feelings of belonging or severity of suicidal ideation. Given that social disconnection was an inclusion criterion for the study, voluntary participation in in-person research interviews and interim telephone contacts to sustain engagement were sources of social connection for subjects in both conditions that likely muted the findings. Also, older adults rarely report suicidal ideation and since subjects for the study were not selected on that basis, it is unsurprising that significant changes were not observed. Future studies could investigate whether subgroups of socially disconnected older adults, such as those with more severe isolation, depression, or functional impairment that limits social interaction, might benefit more from peer companionship. Other limitations include the need to replicate the findings in other ASN agencies and geographic regions, and our inability to measure benefits of the TSC intervention to subjects’ physical health and functioning. Because there is such a strong association between social connectedness and physical health outcomes, one would expect to observe such benefits, most likely over a longer time frame than the 12-month duration reported here. Given that financing of a peer support intervention could be derived from cost reductions related to improved health and reduced utilization, further study of its impact on physical health, service utilization and cost are warranted.
In older adulthood men are less likely than women to endorse emotional distress and seek help for mental illness.38 Rates of suicide death soar among men with advancing age in the United States whereas they peak in mid-life and drop in later years for women.39 Studies of interventions to reduce suicide risk in later life have tended to show benefit for women but not men, however, underscoring the challenge of suicide prevention in this group.40 We saw no apparent sex difference in intervention responsiveness, offering hope that peer companionship may provide benefits to both sexes.
Given the likelihood that COVID-19 and other viral pathogens will continue to threaten the well-being of older adults and require social distancing intermittently in the future, implementation of TSC using telehealth technology warrants urgent study. Research is also needed on the steps required to ensure uptake and dissemination of peer companionship interventions by the primary care sector through collaborations with aging services given that these partnerships are not widespread.1 Because social disconnectedness has both medical and social impacts, health and aging service systems should partner to address it.
AUTHOR CONTRIBUTIONS
YC was the principal investigator and obtained funding. YC, KVO, DS, WM, JR, CP, and XT designed the study. KVO oversaw its implementation and supervised the research assessments. JR supervised the peer companions. XR, SM, and KK analyzed the data and YC, KVO, XT, CP, and SM interpreted the findings. YC, KVO, XT, and SM were involved in writing the text and all authors reviewed and approved of the paper before submission.
Acknowledgments
Dr. Stone and Ms. McIntosh were employees of the Center for Disease Control and Prevention, which funded the study. Drs. Conwell, Tu, and Van Orden receive funding from the U.S National Institutes of Health for research unrelated to this study. None of the authors have conflicts of interest to disclose, currently or in the last three years, including specific financial interests and relationships and affiliations relevant to the subject of this manuscript.
The study was supported by a grant from the U.S. Centers for Disease Control and Prevention (U01CE001942) We wish to thank all members of the TSC team, participating primary care practices, the staff of Lifespan, and the volunteers who gave so much time and effort to help show the effects of peer companionship on older adult health.
Previous presentation: The study protocol and preliminary findings were reported in oral presentations at the annual meetings of the American Association of Geriatric Psychiatry, held in Orlando, FL from March 14–17, 2014 and the Gerontological Society of America, also held in Orlando from November 19–22, 2015. The study protocol was also published without inclusion of findings (Van Orden et al: The Senior Connection: Design and rationale of a randomized trial of peer companionship to reduce suicide risk in later life. Contemp Clin Trials. 2013;35:117-126).
Footnotes
TRIAL REGISTRATION: ClinicalTrials.gov Identifier: NCT01408654
References
- 1.National Academies of Sciences, Engineering, and Medicine . 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the HealthCare System. Washington, DC. [DOI] [PubMed] [Google Scholar]
- 2.Perissinotto CM, StijacicCenzer I, Covinsky KE. Loneliness in older persons: a predictor of functional decline and death. Arch Intern Med. 2012;172:1078–1083. doi: 10.1001/archinternmed.2012.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol. 2009;28:354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawkley LC, Masi CM, Berry JD. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- 5.Pressman SD, Cohen S, Miller GE. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychol. 2005;24(3):297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- 6.Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453–463. doi: 10.1037/a0017216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holt-Lunstad J, Smith TB, Baker M. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sc. 2015;10(2):227–237. doi: 10.1177/1745691614568352. [DOI] [PubMed] [Google Scholar]
- 8.Holt-Lunstat J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7 doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhong BL, Chen SL, Tu X. Loneliness and cognitive function in older adults: findings from the Chinese Longitudinal Healthy Longevity Survey. J Gerontol B Psychol Sci Soc Sci. 2017;72:120–128. doi: 10.1093/geronb/gbw037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Van Orden KA, Witte TK, Cukrowicz KC. The interpersonal theory of suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stickley A, Koyanagi A. Loneliness, common mental disorders and suicidal behavior: findings from a general population survey. J Affect Disord. 2016;197:81–87. doi: 10.1016/j.jad.2016.02.054. [DOI] [PubMed] [Google Scholar]
- 12.Duberstein PR, Conwell Y, Conner KR. Suicide at 50 years of age and older: perceived physical illness, family discord and financial strain. Psychol Med. 2004;34:137–146. doi: 10.1017/s0033291703008584. [DOI] [PubMed] [Google Scholar]
- 13.Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32:1–9. doi: 10.1521/suli.32.1.1.22184. [DOI] [PubMed] [Google Scholar]
- 14.Duberstein PR, Conwell Y, Conner KR. Poor social integration and suicide: fact or artifact? A case-control study. Psychol Med. 2004;34:1331–1337. doi: 10.1017/s0033291704002600. [DOI] [PubMed] [Google Scholar]
- 15.Rubenowitz E, Waern M, Wilhelmson K. Life events and psychosocial factors in elderly suicides–a case-control study. Psychol Med. 2001;31:1193–1202. doi: 10.1017/s0033291701004457. [DOI] [PubMed] [Google Scholar]
- 16.Jeste DV, Lee EE, Cacioppo S. Battling the modern behavioral epidemic of loneliness: suggestions for research and interventions. JAMA Psychiatry. 2020;77:553–554. doi: 10.1001/jamapsychiatry.2020.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perissinotto C, Holt-Lunstad J, Periyakoil VS. A practical approach to assessing and mitigating loneliness and isolation in older adults. J Am Geriatr Soc. 2019;67:657–662. doi: 10.1111/jgs.15746. [DOI] [PubMed] [Google Scholar]
- 18.Bath PA, Gardiner A. Social engagement and health and social care use and medication use among older people. Eur J Ageing. 2005;2:56–63. doi: 10.1007/s10433-005-0022-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Administration on Aging Elder Locator; the aging network: Available at: https://eldercare.acl.gov/Public/About/Aging_Network/Index.aspx. Accessed April 1, 2020
- 20.Siette J, Cassidy M, Priebe S. Effectiveness of befriending interventions: a systematic review and meta-analysis. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-014304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mead N, Lester H, Chew-Graham C. Effects of befriending on depressive symptoms and distress: systematic review and meta-analysis. Br J Psychiatry. 2010;196:96–101. doi: 10.1192/bjp.bp.109.064089. [DOI] [PubMed] [Google Scholar]
- 22.Van Orden KA, Stone DM, Rowe J. The Senior Connection: design and rationale of a randomized trial of peer companionship to reduce suicide risk in later life. Contemp Clin Trials. 2013;35:117–126. doi: 10.1016/j.cct.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lifespan of Greater Rochester, Inc. Available at: http://www.lifespan-roch.org. Accessed April 1, 2020
- 24.Borson S, Scanlan JM, Watanabe J. Simplifying detection of cognitive impairment: comparison of the Mini-Cog and Mini-Mental State Examination in a multiethnic sample. J Am Geriatr Soc. 2005;53:871–874. doi: 10.1111/j.1532-5415.2005.53269.x. [DOI] [PubMed] [Google Scholar]
- 25.Bush K, Kivlahan DR, McDonell MB. The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- 26.Wei LJ, Lachin JM. Properties of the urn randomization in clinical trials. Control Clin Trials. 1988;9:345–364. doi: 10.1016/0197-2456(88)90048-7. [DOI] [PubMed] [Google Scholar]
- 27.Senior Corps Programs - RSVP; Available at: https://www.nationalservice.gov/programs/senior-corps/senior-corps-programs/rsvp. Accessed June 29, 2019
- 28.Heisel MJ, Flett GL. The Development and initial validation of the Geriatric Suicide Ideation Scale. Am J Geriatr Psychiatry. 2006;14:742–751. doi: 10.1097/01.JGP.0000218699.27899.f9. [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lowe B, Decker O, Muller S. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46:266–274. doi: 10.1097/MLR.0b013e318160d093. [DOI] [PubMed] [Google Scholar]
- 31.Van Orden KA, Cukrowicz KC, Witte TK. Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012;24:197–215. doi: 10.1037/a0025358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 33.Paykel ES, Myers JK, Lindenthal JJ. Suicidal feelings in the general population: a prevalence study. Br J Psychiatry. 1974;124:460–469. doi: 10.1192/bjp.124.5.460. [DOI] [PubMed] [Google Scholar]
- 34.Salazar A, Ojeda B, Dueñas M. Simple generalized estimating equations (GEEs) and weighted generalized estimating equations (WGEEs) in longitudinal studies with dropouts: guidelines and implementation in R. Statistics in Medicine. 2016;35:3424–3448. doi: 10.1002/sim.6947. [DOI] [PubMed] [Google Scholar]
- 35.Kroenke K. Minor depression: midway between major depression and euthymia. Ann Intern Med. 2006;144:528–530. doi: 10.7326/0003-4819-144-7-200604040-00013. [DOI] [PubMed] [Google Scholar]
- 36.Hill RM, Pettit JW. Pilot randomized controlled trial of LEAP: a selective preventive intervention to reduce adolescents' perceived burdensomeness. J Clin Child Adolesc Psychol. 2016:1–12. doi: 10.1080/15374416.2016.1188705. [DOI] [PubMed] [Google Scholar]
- 37.VanderWeele TJ, Hawkley LC, Thisted RA. A marginal structural model analysis for loneliness: implications for intervention trials and clinical practice. J Consult ClinPsychol. 2011;79(2):225–235. doi: 10.1037/a0022610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Angst J, Gamma A, Gastpar M. Gender differences in depression. Epidemiological findings from the European DEPRES I and II studies. Eur Arch Psychiatry Clin Neurosci. 2002;252:201–209. doi: 10.1007/s00406-002-0381-6. [DOI] [PubMed] [Google Scholar]
- 39.Centers for Disease Control and Prevention. Web-based injury statistics query and reporting system. Available at: https://www.cdc.gov/injury/wisqars/index.html. Accessed April 1, 2020
- 40.Conwell Y. Suicide prevention in later life: a glass half full, or half empty? Am J Psychiatry. 2009;166:845–848. doi: 10.1176/appi.ajp.2009.09060780. [DOI] [PMC free article] [PubMed] [Google Scholar]