Highlights
-
•
Air quality is tightly associated with COVID-19 transmission.
-
•
PM2.5 and NO2 strongly promote COVID-19 transmission.
-
•
Temperature is inversely associated with COVID-19 transmission.
Keywords: COVID-19, SARS-CoV-2, Ambient air pollutant, Temperature, AQI
Abstract
Objectives
Although COVID-19 is known to be caused by human-to-human transmission, it remains largely unclear whether ambient air pollutants and meteorological parameters could promote its transmission.
Methods
A retrospective study was conducted to study whether air quality index (AQI), four ambient air pollutants (PM2.5, PM10, NO2 and CO) and five meteorological variables (daily temperature, highest temperature, lowest temperature, temperature difference and sunshine duration) could increase COVID-19 incidence in Wuhan and XiaoGan between Jan 26th to Feb 29th in 2020.
Results
First, a significant correlation was found between COVID-19 incidence and AQI in both Wuhan (R2 = 0.13, p < 0.05) and XiaoGan (R2 = 0.223, p < 0.01). Specifically, among four pollutants, COVID-19 incidence was prominently correlated with PM2.5 and NO2 in both cities. In Wuhan, the tightest correlation was observed between NO2 and COVID-19 incidence (R2 = 0.329, p < 0.01). In XiaoGan, in addition to the PM2.5 (R2 = 0.117, p < 0.01) and NO2 (R2 = 0.015, p < 0.05), a notable correlation was also observed between the PM10 and COVID-19 incidence (R2 = 0.105, p < 0.05). Moreover, temperature is the only meteorological parameter that constantly correlated well with COVID-19 incidence in both Wuhan and XiaoGan, but in an inverse correlation (p < 0.05).
Conclusions
AQI, PM2.5, NO2, and temperature are four variables that could promote the sustained transmission of COVID-19.
Introduction
The outbreak of COVID-19 from Wuhan, China, was officially characterized as a pandemic on March 11th, 2020 (World Health Organization, 2020b), which has led to more than 3.5 million subjected infected and 0.24 million dead worldwide as of May 4th, 2020 (World Health Organization, 2020a). The causative pathogen of COVID-19 has been confirmed as the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (Lu et al., 2020), which belongs to the coronavirus family and previously caused severe acute respiratory syndrome (SARS) (Peiris et al., 2004) and the Middle East respiratory syndrome (MERS) (Zaki et al., 2012).
Air pollution has been an on-going research focus as it is a major environmental threat to human health. Sufficient evidence has tightly linked ambient air pollution to occurrence of numerous respiratory diseases, such as COPD (Ling and van Eeden, 2009) and asthma (Gorai et al., 2016). Moreover, air pollution is also associated with infectious diseases transmission. For example, worse air quality has also been shown to increase SARS fatality (Cui et al., 2003) as well as to increase influenza incidence (Landguth et al., 2020). In laboratory conditions, van Doremalen et al. (2020) demonstrated a long viability of SARS-CoV-2 in ambient aerosols, which could be an important source of COVID-19 transmission (Luo et al., 2020). However, whether ambient air pollutants are associated with increased incidence of COVID-19 in realistic situations remains largely unknown.
Previous study indicated that meteorological parameters can affect spread and thriving of multiple viruses. For example, ambient temperature and relative humidity are inversely associated with influenza A infection rate in Japan (Iha et al., 2016). The coronavirus also exhibited a seasonal oscillation of outbreak, which also suggested a strong association between meteorological parameters and virus transmission and viability (Killerby et al., 2018). Moreover, although the epidemiological characteristics of SARS-CoV-2 are not clear, a recent study predicted SARS-CoV-2 transmits more efficiently in winter than summer (Lipsitch, 2020), indicating the importance of temperature in COVID-19 transmission. However, whether COVID-19 transmission is associated with meteorological parameters, at this moment, is not backed by sufficient investigations and robust evidence.
In this retrospective study, we attempted to conduct an exploratory analysis looking at the association between environment conditions (including ambient pollutants and meteoroidal parameter) and COVID-19 incidence/mortality in Wuhan, given a city-wide lockdown and varying pollution/meteorological data throughout the entire study period.
Materials and methods
COVID-19 incidence data
In this time-series analysis, COVID-19 incidence counts in Wuhan and XiaoGan were provided by the Centers for Disease Control and Prevention (CDC) of Hubei Province (Health Commission of the Hubei Province, 2020). The data used in this study are daily case counts of positive diagnoses of COVID-19 from all reporting sources, including laboratory and clinical diagnoses. COVID-19 cases of all ages are included. In total, the COVID-19 incidence data for Wuhan produced over 35 ‘clusters’ of time series between Jan 26th to Feb 29th in 2020.
Environmental condition data
The daily air quality index (AQI), PM2.5, PM10, NO2 and CO concentration were retrieved from the Platform AQI (Platform AQI, 2020). Five meteorological parameters were retrieved from the database of Weather.com (The Weather Channel, 2020), including daily mean temperature, highest temperature, lowest temperature, sunrise and sunset time. Daily temperature difference and sunshine duration were calculated based on the difference of highest and lowest temperature and sunrise and sunset time, respectively. Thus, a total of five meteorological parameters were enrolled as independent variables.
Data analysis
Due to imperfect daily reporting practices, COVID-19 incidence numbers in XiaoGan exhibited data on Feb 19th which was −15. Furthermore, China updated their diagnostic criteria on Feb 12th and 13th, which resulted in a significant increase of COVID-19 incidence cases on these days (Han and Yang, 2020). Thus, these data were excluded from the current study.
All data analyses were done in GraphPad Prism® 8.0 (GraphPad Software, La Jolla, CA, USA). First, a descriptive analysis was performed to provide an overview of COVID-19 incidence and air quality during the study period. Next, we utilized a linear regression model to fit the dependent variables (COVID-19 incidence) for each independent variable (four ambient air pollutants and five meteorological parameters). As SARS-CoV-2 has a median incubation period of 4 days in humans (Guan et al., 2020), all independent variables were used to fit daily COVID-19 incidence from 4 days later. The statistical tests were two-sided, and p-value <0.05 was considered as statistically significant.
Results
Detailed information of daily COVID-19 incidence number was listed in Table 1 , including the AQI, four ambient air pollutants and five meteorological parameters. The AQI values for Wuhan and XiaoGan were 63.63 ± 4.47 and 71.58 ± 5, respectively, both of which were categorized as moderate according to the US EPA standard (United States Environmental Protection Agency, 2019a). The highest and lowest daily COVID-19 incidences were 1690 cases on Feb 16th and 80 cases on Jan 26th in Wuhan, respectively. Meanwhile, incidences in XiaoGan were 424 on Feb 5th and 0 on Feb 29th.
Table 1.
An overview of air quality index (AQI), ambient air pollution and meteorological parameters between Jan 26th to Feb 29th in 2020 in Wuhan and XiaoGan, China.
| Wuhan |
XiaoGan |
|||
|---|---|---|---|---|
| Mean | Std. deviation | Mean | Std. deviation | |
| Air quality index (AQI) | 63.63 | 25.30 | 71.58 | 27.83 |
| Ambient air pollutants | ||||
| PM2.5 (μg/m3) | 44.16 | 21.63 | 50.39 | 24.18 |
| PM10 (μg/m3) | 51.88 | 22.26 | 59.65 | 25.98 |
| NO2 (μg/m3) | 21.47 | 7.66 | 11.35 | 3.95 |
| CO (μg/m3) | 0.88 | 0.04 | 1.16 | 0.04 |
| Meteorological parameters | ||||
| Temperature (°C) | 7.19 | 4.04 | 7.26 | 3.92 |
| Daily highest temp (°C) | 13.25 | 4.19 | 12.97 | 4.96 |
| Daily lowest temp (°C) | 4.38 | 4.55 | 4.87 | 3.91 |
| Daily temp diff (°C) | 8.81 | 3.76 | 7.97 | 3.85 |
| Sunshine duration (h) | 11.04 | 0.28 | 10.91 | 0.27 |
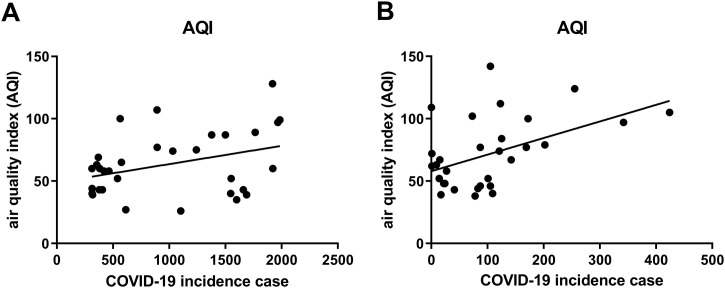
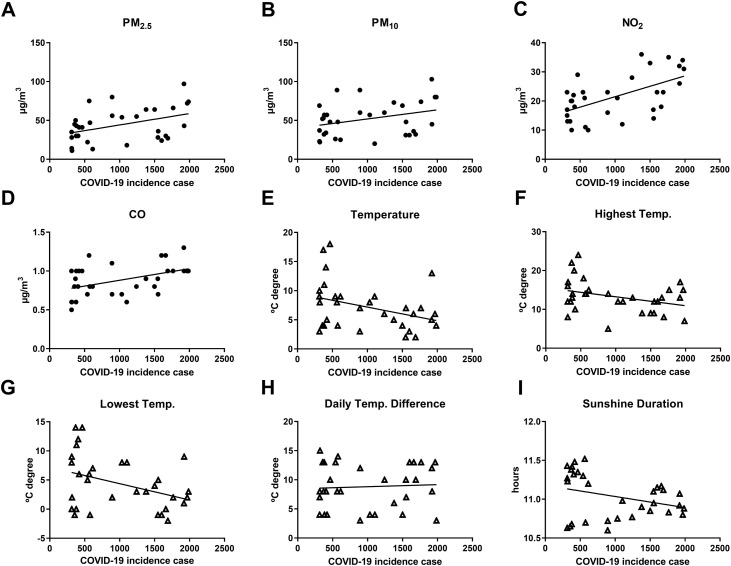
We then looked into the correlation between local AQI and COVID-19 incidence number in each city (Table 2 , Figure 1 ). The data showed that AQI was significantly and positively associated with daily COVID-19 incidence number in both Wuhan (R 2 = 0.13, p < 0.05) and XiaoGan (R 2 = 0.223, p < 0.01), which indicated the important role of AQI in COVID-19 transmission. Thus, we further studied the association of daily newly diagnosed COVID-19 cases with each air pollutant in Wuhan (Table 2, Figure 2 ). Interestingly, all ambient air pollutants showed positive association with daily COVID-19 incidence. Among them, NO2 (R 2 = 0.329, p < 0.01), PM2.5 (R 2 = 0.174, p < 0.05) and CO (R 2 = 0.203, p < 0.001) exhibited statistical significance. Next, we studied the correlation between meteorological parameters and COVID-19 incidence in Wuhan. Among five parameters, daily temperature (R 2 = 0.126, p < 0.05) and daily lowest temperature (R 2 = 0.143, p < 0.05) were predominantly correlated with COVID-19 incidence, but both in an inverse correlation.
Table 2.
The correlation between COVID-19 incidence and three ambient air pollutants along with five meteorological parameters, Jan 26th to Feb 29th in 2020 in Wuhan and XiaoGan, China. The data marked with *, ** and *** indicated statistical significance, where p < 0.05, 0.01 and 0.001, respectively.
| Wuhan |
XiaoGan |
|||
|---|---|---|---|---|
| Slope | R2 | Slope | R2 | |
| Air quality index (AQI) | 0.015 ± 0.007* | 0.127 | 0.133 ± 0.046** | 0.222 |
| Ambient air pollutants | ||||
| PM2.5 | 0.015 ± 0.006* | 0.174 | 0.117 ± 0.046** | 0.23 |
| PM10 | 0.117 ± 0.006 | 0.105 | 0.105 ± 0.044* | 0.158 |
| NO2 | 0.007 ± 0.002*** | 0.329 | 0.015 ± 0.007* | 0.158 |
| CO | 0.000 ± 0.000** | 0.203 | −0.000 + 0.000 | 0.022 |
| Meteorological data | ||||
| Temperature | −0.002 ± 0.001* | 0.126 | −0.014 ± 0.007* | 0.13 |
| Daily highest temp | −0.002 ± 0.001 | 0.114 | −0.014 ± 0.009 | 0.076 |
| Daily lowest temp | −0.003 ± 0.001* | 0.143 | −0.013 ± 0.007 | 0.109 |
| Daily temp diff | 0.000 ± 0.001 | 0.003 | −0.001 ± 0.007 | 0.001 |
| Sunshine duration | −0.000 ± 0.000 | 0.000 | −0.002 ± 0.000*** | 0.407 |
Figure 1.
The correlation between daily COVID-19 incidence and air quality index (AQI) in Wuhan (A) and XiaoGan (B).
Figure 2.
The correlation between daily COVID-19 incidence and ambient air pollution/five meteorological parameters in Wuhan.
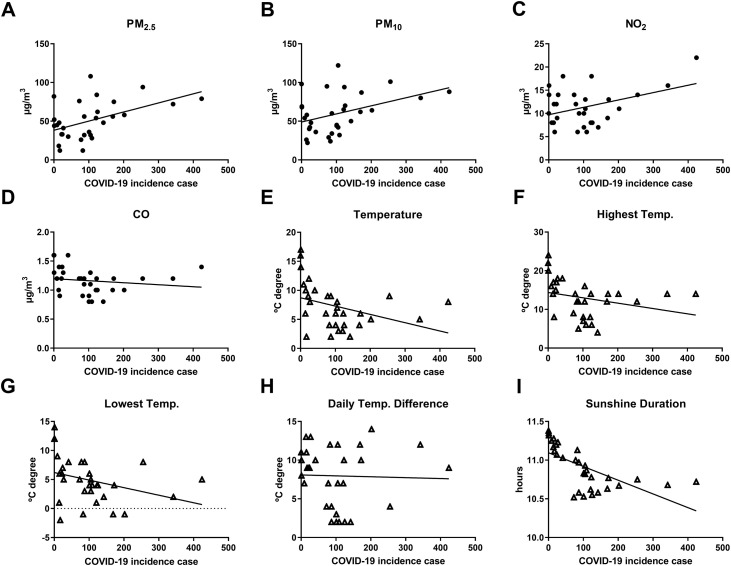
In XiaoGan, both PM2.5 (R 2 = 0.23, p < 0.01) and NO2 (R 2 = 0.158, p < 0.05) were also apparently associated with COVID-19 incidence. Moreover, a notable correlation was also observed between the PM10 and incidence cases (R 2 = 0.158, p < 0.05). Among five meteorological factors, COVID-19 incidence correlated well with the temperature (R 2 = 0.13, p < 0.05) and daily sunshine duration (R 2 = 0.407, p < 0.01), which were, however, in an inverse correlation (Figure 3 ).
Figure 3.
The correlation between daily COVID-19 incidence and ambient air pollution/five meteorological parameters in XiaoGan.
Discussion
Multiple factors could impact viral transmission. For example, influenza viability and activity could be potentiated by ambient air pollutants and some meteorological variables (Iha et al., 2016, Landguth et al., 2020). However, this has not been examined for the SARS-CoV-2. Thus, a preliminary analysis was conducted in the current study to assess the role of air pollution and meteorological parameters on COVID-19 transmission. We found that COVID-19 incidence was enhanced by increased AQI (decreased air quality), PM2.5, and NO2 and weakened by temperature.
The PM is hazardous due to its complicate composition and strong capacity of air suspension. PM could be divided into coarse and fine particulate matter, whose diameters are less than 10 μm and 2.5 μm, respectively. Among various causes of respiratory illness, the PM has been shown to potentiate viral transmissions. For instance, ambient PM2.5 concentration was prominently correlated with influenza-like illness risk during the flu season in Beijing, China (Feng et al., 2016). In a single hospital setting, researchers found that both influenza and respiratory syncytial virus remain airborne for a long time period after they attach to PM, which allows viruses to be transmitted by the airborne route (Lindsley et al., 2010). Additionally, viral replication in the respiratory system is enhanced by the negative effect of PM on the human respiratory barrier integrity (Xian et al., 2020, Zhao et al., 2018). However, it remains particularly unclear whether the ambient air pollutant could assist SARS-CoV-2 transmission. In the current study, the PM2.5 concentration is correlated with the COVID-19 incidence in a positive correlation, which agreed with previous studies. Based on this information, we hypothesize that PM could potentiate the transmission ability of SARS-CoV-2 in two ways: (1) PM2.5 could disrupt the integrity of the human respiratory barrier integrity (Zhao et al., 2018). Thus, the dysfunctional respiratory barriers are more likely to expose deeper respiratory tissue to foreign pathogens. (2) PM could form condensation nuclei for viral attachment (Lee et al., 2014). Due to its relatively smaller size, PM2.5 is more pernicious as it can penetrate the respiratory tract and reach alveoli directly (Tellier, 2009). Since both PMs, especially PM2.5 concentration, were constantly higher than safety guidelines of the US EPA (United States Environmental Protection Agency, 2019b) in both cities, we believed that PM2.5 is a stronger factor promoting SARS-CoV-2 transmission.
A number of studies demonstrate the adverse health effects of NO2 exposure. For example, short-term increase of outdoor NO2 concentration can significantly increase the risk of upper respiratory tract infection (Li et al., 2018). This phenomenon was particularly notable in children, as this subpopulation is highly susceptible to NO2 induced lung injury (Ghosh et al., 2012, Lin et al., 2013, Moshammer et al., 2006). Viral infection was common after NO2 exposure. According to Chauhan et al. (2003), four viruses were frequently detected in NO2-related respiratory tract infection, and coronavirus was one of them. Previous study indicated that preceding NO2 exposure can decrease host immunity and thus significantly increase infection risk of cytomegalovirus in mice (Rose et al., 1988). Moreover, recovered mice tended to be re-infected after re-exposing to NO2 (Rose et al., 1989). In the current study, although the NO2 level was constantly lower than the US EPA standards (United States Environmental Protection Agency, 2016), our data revealed that COVID-19 incidence was highly correlated with the ambient NO2 concentration. This finding agreed with epidemiological studies from other regions of the world (Chauhan et al., 2003, Lin et al., 2013).
So far, epidemiological studies identified at least nine virus categories that are capable of infecting the respiratory tract (Nichols et al., 2008, Pavia, 2011). Although all feature seasonal oscillation of outbreaks, only three viruses show peak incidences in the winter months, which are the Influenza, human coronavirus, and human respiratory syncytial virus (Killerby et al., 2018, Midgley et al., 2007). Although the epidemiological characteristics of SARS-CoV-2 are not clear, recent study predicted that SARS-CoV-2 transmits more efficiently in winter than summer (Lipsitch, 2020), indicating the importance of temperature. These data agreed with our results as temperature seems to decrease the incidence of COVID-19, indicating an inhibitory effect of temperature on SARS-CoV-2 transmission. This phenomenon might be related to life-style as people tend to huddle indoors together during the winter season. Future study needs to investigate the direct effect of temperature on viral activity as well.
Other than the PM and NO2, the data from Wuhan also indicated that CO has a strong positive effect on SARS-CoV-2 transmission. However, the data from XiaoGan failed to repeat the same result. So far, only a few studies are available concerning the effect of CO on viral transmission. For example, Su et al. (2019) presented that CO can increase the risk of influenza-like illness. Ali also identified that CO had a weak positive association with influenza transmissibility (Ali et al., 2018). We believe our current results could not fully represent the potency of CO on SARS-CoV-2 transmission due to relatively limited study period and location. Thus, we cannot conclude the effect of CO on SARS-CoV-2 transmission based on current data. Further studies are required to elaborate on this issue.
The current study has some limitations. First, there are only two cities enrolled, which might result in some results deviation from the exact effect of ambient pollution and meteorological parameters on SARS-CoV-2 transmission. Second, the study period is relatively short compared to other epidemiological study. In future study, we will enroll more data from multiple countries and areas to validate the results from current study.
In conclusion, we found that AQI, PM2.5, NO2 and temperature are four variables that could potential promote the sustained transmission of SARS-CoV-2. Personal protective devices, especially the facial mask, shall be suggested to residents for coronavirus protection in highly polluted regions.
Conflict of interest
There is no conflict of interest in this study.
Funding
The current study is supported by the Natural Science Foundation of Liaoning Province, China (20180551153).
Ethical approval
The current study has been approved by the ethics committee of Shanghai Rui-Jin Hospital.
Acknowledgements
We want to thank all medical workers for their great contribution and sacrifice during this COVID-19 pandemic.
References
- Ali S., Wu P., Cauchemez S., He D., Fang V., Cowling B. Ambient ozone and influenza transmissibility in Hong Kong. Eur Respir J. 2018;51(5):1800369. doi: 10.1183/13993003.00369-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A., Inskip H., Linaker C., Smith S., Schreiber J., Johnston S. Personal exposure to nitrogen dioxide (NO2) and the severity of virus-induced asthma in children. Lancet. 2003;361(9373):1939–1944. doi: 10.1016/S0140-6736(03)13582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z., Froines J., Zhao J., Wang H., Yu S. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ Health. 2003;2(1):15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng C., Li J., Sun W., Zhang Y., Wang Q. Impact of ambient fine particulate matter (PM2.5) exposure on the risk of influenza-like-illness: a time-series analysis in Beijing, China. Environ Health. 2016;15:17. doi: 10.1186/s12940-016-0115-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh R., Joad J., Benes I., Dostal M., Sram R.J., Hertz-Picciotto I. Ambient nitrogen oxides exposure and early childhood respiratory illnesses. Environ Int. 2012;39(1):96–102. doi: 10.1016/j.envint.2011.10.001. [DOI] [PubMed] [Google Scholar]
- Gorai A., Tchounwou P., Tuluri F. Association between Ambient air pollution and asthma prevalence in different population groups residing in eastern Texas, USA. Int J Environ Res Public Health. 2016;13(4):378. doi: 10.3390/ijerph13040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W.-J., Ni Z.-Y., Hu Y., Liang W.-H., Ou C.-Q., He J.-X. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Y., Yang H. The transmission and diagnosis of 2019 novel coronavirus infection disease (COVID-19): a Chinese perspective. J Med Virol. 2020 doi: 10.1002/jmv.25749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Commission of the Hubei Province . 2020. The real time corona virus epidemiological situation of Hubei province. Available from: http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/index.shtml. [Google Scholar]
- Iha Y., Kinjo T., Parrott G., Higa F., Mori H., Fujita J. Comparative epidemiology of influenza A and B viral infection in a subtropical region: a 7-year surveillance in Okinawa, Japan. BMC Infect Dis. 2016;16(1):650. doi: 10.1186/s12879-016-1978-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killerby M., Biggs H., Haynes A., Dahl R., Mustaquim D., Gerber S. Human coronavirus circulation in the United States 2014–2017. J Clin Virol. 2018;101:52–56. doi: 10.1016/j.jcv.2018.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landguth E., Holden Z., Graham J., Stark B., Mokhtari E., Kaleczyc E. The delayed effect of wildfire season particulate matter on subsequent influenza season in a mountain west region of the USA. Environ Int. 2020;139:105668. doi: 10.1016/j.envint.2020.105668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee G., Saravia J., You D., Shrestha B., Jaligama S., Hebert V. Exposure to combustion generated environmentally persistent free radicals enhances severity of influenza virus infection. Part Fibre Toxicol. 2014;11:57. doi: 10.1186/s12989-014-0057-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Xiao C., Li J., Tang J., Geng X., Cui L. Association between air pollution and upper respiratory tract infection in hospital outpatients aged 0–14 years in Hefei, China: a time series study. Public Health. 2018;156:92–100. doi: 10.1016/j.puhe.2017.12.006. [DOI] [PubMed] [Google Scholar]
- Lin Y., Chang C., Chang S., Chen P., Lin C., Wang Y. Temperature, nitrogen dioxide, circulating respiratory viruses and acute upper respiratory infections among children in Taipei, Taiwan: a population-based study. Environ Res. 2013;120:109–118. doi: 10.1016/j.envres.2012.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsley W., Blachere F., Davis K., Pearce T., Fisher M., Khakoo R. Distribution of airborne influenza virus and respiratory syncytial virus in an urgent care medical clinic. Clin Infect Dis. 2010;50(5):693–698. doi: 10.1086/650457. [DOI] [PubMed] [Google Scholar]
- Ling S., van Eeden S. Particulate matter air pollution exposure: role in the development and exacerbation of chronic obstructive pulmonary disease. Int J Chronic Obstr Pulm Dis. 2009;4:233–243. doi: 10.2147/copd.s5098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M. 2020. Seasonality of SARS-CoV-2: will COVID-19 go away on its own in warmer weather? Available from: https://ccdd.hsph.harvard.edu/will-covid-19-go-away-on-its-own-in-warmer-weather/ [Google Scholar]
- Lu R., Zhao X., Li J., Niu P., Yang B., Wu H. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo C., Yao L., Zhang L., Yao M., Chen X., Wang Q. Possible transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in a public bath center in Huai’an, Jiangsu Province, China. JAMA Netw Open. 2020;3(3):e204583. doi: 10.1001/jamanetworkopen.2020.4583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Midgley C., Haynes A., Baumgardner J., Chommanard C., Demas S., Prill M. Determining the seasonality of respiratory syncytial virus in the United States: the impact of Increased molecular testing. J Infect Dis. 2007;216:345–355. doi: 10.1093/infdis/jix275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moshammer H., Hutter H., Hauck H., Neuberger M. Low levels of air pollution induce changes of lung function in a panel of schoolchildren. Eur Respir J. 2006;27:1138–1143. doi: 10.1183/09031936.06.00089605. [DOI] [PubMed] [Google Scholar]
- Nichols W., Campbell A., Boeckh M. Respiratory viruses other than influenza virus: impact and therapeutic advances. Clin Microbiol Rev. 2008;21(2):274–290. doi: 10.1128/CMR.00045-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavia A. Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis. 2011;52(Suppl. 4):S284–S289. doi: 10.1093/cid/cir043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris J., Guan Y., Yuen K. Severe acute respiratory syndrome. Nat Med. 2004;10(12 Suppl):S88–S97. doi: 10.1038/nm1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platform AQI . 2020. Online air quality monitoring and analysis platform. Available from: https://www.aqistudy.cn/ [Google Scholar]
- Rose R., Fuglestad J., Skornik W., Hammer S., Wolfthal S., Beck B. The pathophysiology of enhanced susceptibility to murine cytomegalovirus respiratory infection during short-term exposure to 5 ppm nitrogen dioxide. Am Rev Respir Dis. 1988;137:912–917. doi: 10.1164/ajrccm/137.4.912. [DOI] [PubMed] [Google Scholar]
- Rose R., Pinkston P., Skornik W. Health Effects Institute; 1989. Altered susceptibility to viral respiratory infection during short-term exposure to nitrogen dioxide. Research Report 24; pp. 1–24. [PubMed] [Google Scholar]
- Su W., Wu X., Geng X., Zhao X., Liu Q., Liu T. The short-term effects of air pollutants on influenza-like illness in Jinan, China. BMC Public Health. 2019;19(1):1319. doi: 10.1186/s12889-019-7607-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tellier R. Aerosol transmission of influenza A virus: a review of new studies. J R Soc Interface. 2009;6(Suppl. 6):S783–S790. doi: 10.1098/rsif.2009.0302.focus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Weather Channel . 2020. Wuhan, Hubei, People's Republic of China monthly weather. Available from: https://weather.com/weather/monthly/l/2637660151899903e8cbdd23636051470b6731863286ec74b3033421cb87e1e8. [Google Scholar]
- United States Environmental Protection Agency . 2016. NAAQS table. Available from: https://www.epa.gov/criteria-air-pollutants/naaqs-table. [Google Scholar]
- United States Environmental Protection Agency . 2019. Understanding the AQI. Available from: https://cfpub.epa.gov/airnow/index.cfm?action=aqibasics.aqi. [Google Scholar]
- United States Environmental Protection Agency . 2019. What are the air quality standards for PM? Available from: https://www3.epa.gov/region1/airquality/pm-aq-standards.html. [Google Scholar]
- van Doremalen N., Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . 2020. Coronavirus disease (COVID-19) outbreak situation. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Google Scholar]
- World Health Organization . 2020. Situation Report – 51. Coronavirus disease 2019 (COVID-19) [Google Scholar]
- Xian M., Ma S., Wang K., Lou H., Wang Y., Zhang L. Particulate matter 2.5 causes deficiency in barrier integrity in human nasal epithelial cells. Allergy Asthma Immunol Res. 2020;12(1):56–71. doi: 10.4168/aair.2020.12.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki A., van Boheemen S., Bestebroer T., Osterhaus A., Fouchier R. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia. N Engl J Med. 2012;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- Zhao R., Guo Z., Zhang R., Deng C., Xu J., Dong W. Nasal epithelial barrier disruption by particulate matter ≤2.5 μm via tight junction protein degradation. J Appl Toxicol. 2018;38(5):678–687. doi: 10.1002/jat.3573. [DOI] [PubMed] [Google Scholar]