Abstract
N/A.
Keywords: Obesity, Sleep apnea, Renin-angiotensin system, Covid-19, Vitamin D deficiency, Sarcopenia
Dear Editor,
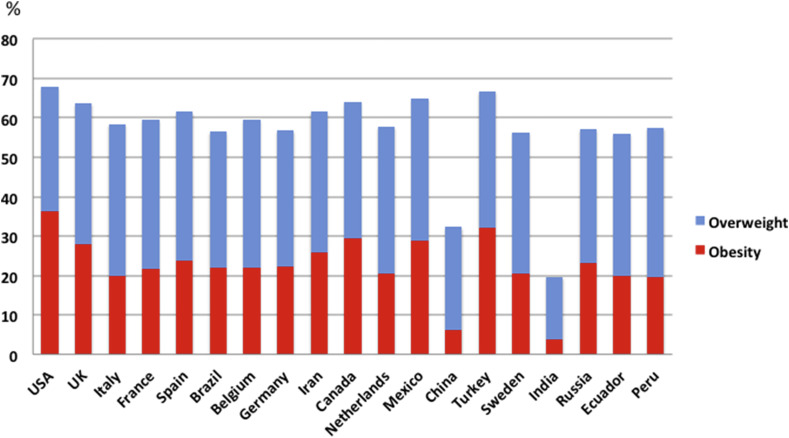
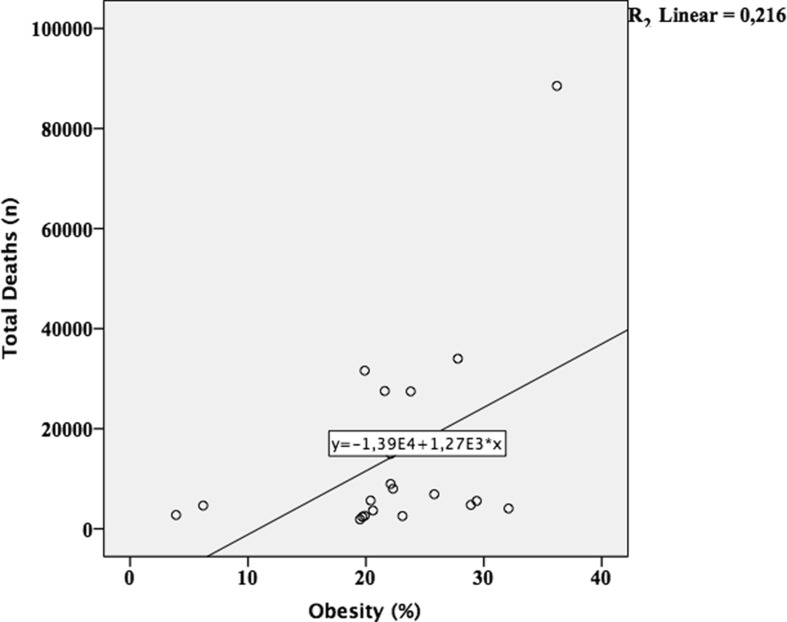
As the high prevalence of obesity in COVID-19 has been shown, the possible interactions between obesity and COVID-19 need to be further deciphered. From this point of view, we determined the obesity prevalence of the top 20 ranked countries by total deaths due to COVID-19. The data regarding the obesity prevalence of countries were obtained from global health services data of the World Health Organization [1,2]. Interestingly, The United States of America ranked first in terms of obesity prevalence (36.2%), overweight prevalence (31.7%), and also the number of total deaths. Overall, most of the countries had a prevalence between 20% and 30% (e.g., UK, Canada, Iran, Mexico, Chile). The obesity prevalence was less than 10% in two countries (India and China) only (Fig. 1 ). When we look at the correlation analysis between the obesity prevalence and the number of total deaths de to COVID-19, the number of total deaths significantly correlated with the obesity prevalence (p = 0.039, r = 0.464) (Fig. 2 ). In other words, as the obesity prevalence increased, the number of total deaths increased. It can be said that obesity-related conditions seem to worsen the effect of COVID-19. Herein, we believe that cardiovascular and metabolic effects, sleep apnea, vitamin D deficiency, dysregulation of the renin-angiotensin-aldosterone system (RAAS) as well as sarcopenia should be taken into account as obesity-related confounders to COVID-19. Therefore, highlighting the possible associations of the aforementioned conditions would be reasonable for the fight against COVID-19.
Fig. 1.
Obesity prevalence and number of total deaths
The graph shows the obesity and overweight prevalence of countries ranked in the top 20 by the total number of deaths due to COVID-19 as of May 20, 2020.
Fig. 2.
Correlation analysis between obesity prevalence and the number of total deaths
A significant correlation between the number of total deaths (as of May 20, 2020) and obesity prevalence was observed (p = 0.039, r = 0.464).
The angiotensin-converting enzyme 2 (ACE2) is shown to be the entry point of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). This makes sense in patients with obesity because dysregulation/increase of the RAAS has deleterious influences on several systems, has been shown in patients with obesity. For instance, the dysregulation of the RAAS causes vasoconstriction, increased blood pressure, oxidative stress, inflammation, endothelial dysfunction, maladaptive immune modulation as well as fibrosis [3]. As such, obesity is a significant risk factor of diabetes mellitus, increased blood pressure, cardiovascular diseases, and respiratory diseases. Further, myeloid and lymphoid responses within the RAAS receptor signaling are associated with abnormal cytokine profiles. The adipose tissue can manifest as a reservoir for a wider viral spread with increased shedding, immune activation, and cytokine amplification in relevant patients as well [4,5].
On the other hand, obstructive sleep apnea (OSA) is a sleep-related breathing disorder, which is characterized by hypoxia and apnea/hypopnea due to the intermittent collapse of the upper airways during sleep. First of all, obesity is a predominant risk factor for OSA (obesity hypoventilation syndrome), and OSA patients may be vulnerable to COVID-19. Obesity hypoventilation syndrome contributes to respiratory failure in patients with acute respiratory distress syndrome [6]. This fact is vital for patients, particularly with respiratory distress and followed-up in intensive care units [7]. Sleep efficacy has multisystemic effects and is accepted as a very important factor for the regulation and maintenance of the immune system. Worse sleep efficacy is associated with decreased immune system activity [4]. The dysregulation/increase of the RAAS has been shown in OSA patients, likewise in obesity [6].
Vitamin D deficiency, very common in people with obesity, is accepted as another pandemic and has unfavorable impacts on several systems. Immunomodulant, anti-inflammatory and protective effects against infections have been shown. Additionally, it should be kept in mind that vitamin D deficiency worsens obesity by enhancing lipogenesis [8]. On the other hand, sarcopenia, the age-related loss of muscle mass and function, with obesity (sarcopenic obesity) is seen in approximately one-fifth of older populations. Sarcopenia is a physical determinant of frailty, and sarcopenic obesity is highly in association with increased risk of disability, institutionalization, and even mortality [9].
In short, presenting this letter, we would like to highlight that fighting against COVID-19 on the basis of obesity should encompass several multisystem approaches such as inhibition of the RAAS, weight loss, vitamin D supplementation, management of OSA as well as prevention of sarcopenia/frailty.
Funding
None.
CRediT authorship contribution statement
Timur Ekiz: Writing - original draft. Ahmet Cemal Pazarlı: Writing - original draft.
Declaration of competing interest
None.
References
- 1.2016. Global health services data, obesity and overweight: World Health Organization.https://www.who.int/gho/ncd/risk_factors/overweight_obesity/obesity_adults/en/ available at: [Accessed May 2020] [Google Scholar]
- 2.Coronavirus disease (Covid-2019) World Health Organization; Geneva: 2020. Situation reports.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/ available at: [Google Scholar]
- 3.Zores F., Rebeaud M.E. COVID and the renin-angiotensin system: are hypertension or its treatments deleterious? Front Cardiovasc Med. 2020;7:71. doi: 10.3389/fcvm.2020.00071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryan P.M., Caplice N.M. Is adipose tissue a reservoir for viral spread, immune activation and cytokine amplification in COVID-19. Obesity. 2020 doi: 10.1002/oby.22843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malavazos A.E., Corsi Romanelli M.M., Bandera F., Iacobellis G. Targeting the adipose tissue in COVID-19. Obesity. 2020 doi: 10.1002/oby.22844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pazarlı A.C., Ekiz T., İlik F. Coronavirus disease 2019 and obstructive sleep apnea syndrome. Sleep Breath. 2020 doi: 10.1007/s11325-020-02087-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malhotra A., Hillman D. Obesity and the lung: 3. Obesity, respiration and intensive care. Thorax. 2008;63:925-31. doi: 10.1136/thx.2007.086835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Oliveira L.F., de Azevedo L.G., da Mota Santana J., de Sales L.P.C., Pereira-Santos M. Obesity and overweight decreases the effect of vitamin D supplementation in adults: systematic review and meta-analysis of randomized controlled trials. Rev Endocr Metab Disord. 2020;21:67–76. doi: 10.1007/s11154-019-09527-7. [DOI] [PubMed] [Google Scholar]
- 9.Bouchonville M.F., Villareal D.T. Sarcopenic obesity: how do we treat it? Curr Opin Endocrinol Diabetes Obes. 2013;20:412–419. doi: 10.1097/01.med.0000433071.11466.7f. [DOI] [PMC free article] [PubMed] [Google Scholar]