Abstract
Background:
Bacillary dysentery (BD) remains a significant public health issue, especially in developing countries. Evidence assessing the risk of BD from temperature is limited, particularly from national studies including multiple locations with different climatic characteristics.
Objectives:
We estimated the effect of temperature on BD across China, assessed heterogeneity and attributable risks across cities and regions, and projected the future risk of BD under climate change.
Methods:
Daily BD surveillance and meteorological data over 2014–2016 were collected from the Chinese Center for Disease Control and Prevention and the China Meteorology Administration, respectively. A two-stage statistical model was used to estimate city-specific temperature–BD relationships that were pooled to derive regional and national estimates. The risk of BD attributable to temperature was estimated, and the future burden of BD attributable to temperature was projected under different climate change scenarios.
Results:
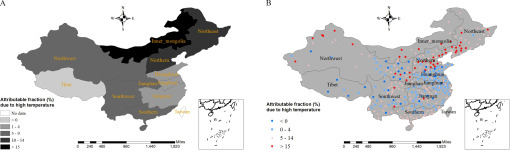
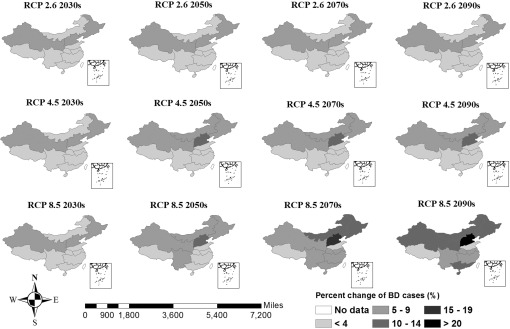
A positive linear relationship for the pooled effect was estimated at the national level. Subgroup analyses indicate that the estimated effect of temperature on BD was similar by age ( or ) and gender. At baseline, estimated attributable risks for BD due to average daily mean temperatures above the 50th percentile were highest for the Inner Mongolia (16%), Northeast China (14%), and Northern China (13%). Most of the individual cities in the same regions and most of the cities in the Northwest, Southern, and Southwest regions, had high attributable risks (). The Northern, Northeast, Inner Mongolia, Northwest, and Southern China regions were identified as high risk for future BD, with estimated increases by the 2090s compared with baseline of 20% (95% confidence interval: 11%, 27%), 15% (6%, 20%), 15% (, 22%), 12% (1%, 19%), and 11% (5%, 15%), respectively, under Representative Concentration Pathway 8.5.
Conclusions:
The positive association between temperature and BD in different climatic regions of China, and the projection for increased risk due to climate change, support efforts to mitigate future risks. https://doi.org/10.1289/EHP5779
Introduction
Bacillary dysentery (BD), also known as shigellosis, is still a leading cause of morbidity and mortality worldwide, disproportionately affecting young children in developing countries (Kotloff et al. 2018). It causes roughly 125 million diarrheal episodes annually, leading to around 160,000 deaths globally (Bardhan et al. 2010). In China, BD is the third leading notifiable infectious disease, particularly in less developed regions, although the morbidity has fallen over the last three decades (Wang et al. 2006).
Climate influences the transmission of enteric infections by affecting pathogens, hosts, and human behavior (Wu et al. 2016). A study conducted in Australia indicates that increases in temperatures were associated with an increase in Salmonella infection in both subtropical and tropical regions (Zhang et al. 2010). In China, BD is seasonal, with most cases occurring from June to September, suggesting that weather variables, especially temperature, may affect the transmission (Chang et al. 2016; Li et al. 2015). Although several studies have explored the association between weather factors and BD in different areas in China (Li et al. 2013, 2015; Liu et al. 2019; Ma et al. 2013; Yan et al. 2017; Zhang et al. 2007, 2008; Zhao et al. 2016), the existing epidemiological evidence is not comparable because most temperature–BD relationship studies were undertaken at a single location, used different models, and yielded inconsistent results. Furthermore, most studies did not explore the attributable risk due to temperature and did not project the future disease burden. Given its vast geographical area and climatic diversity, there is a need for China to undertake an integrated, large-scale national investigation of the heterogeneity of temperature–BD associations in different climatic regions to support region-specific interventions. Furthermore, it is crucial to understand the temperature-attributable risk of BD occurrence and then to project the future BD burden due to climate change in China, so that adaptation strategies and preventive actions can be implemented accordingly.
Using BD surveillance across different climatic regions, we performed a nationwide study in 316 cities to estimate city-specific, region-specific, and national pooled temperature–BD relationships; assess heterogeneity and temperature-attributable risk across regions; and project future BD burdens under different climate change scenarios. Additional aims were to identify potential vulnerable regions and populations and to provide comprehensive scientific evidence to inform decision-making.
Methods
Study Location
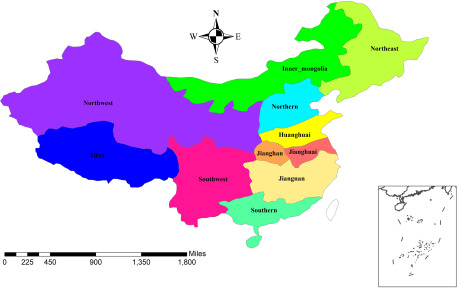
China has 333 prefecture-level cities (including 4 municipalities and 329 prefecture cities) and can be divided into 11 meteorological-geographic regions according to the China Meteorology Administration (CMA) (Figure 1). Because the number of BD cases is very small in smaller cities, an inclusion criterion of above 5% of total BD cases from 2014 to 2016 was adopted. Municipalities and prefecture-level cities were used in this study as the unit for data collection and analysis. Overall, 4 municipalities (Beijing, Shanghai, Tianjin, and Chongqing) and 312 prefecture cities were included (Table S1), and 17 small cities were excluded.
Figure 1.
Meteorological-geographic regions of China. Temperate monsoon climate: Huanghuai and Northern; Mongolia Temperate continental climate and temperate monsoon climate: Inner and Northeast; Subtropical monsoon climate: Jianghan, Jianghuai, and Jiangnan; Temperate continental climate: Northwest; Subtropical monsoon climate and tropical monsoon climate: Southern and Southwest; Plateau and mountain climate: Tibet.
Data Collection
De-identified daily reports of BD cases from 1 January 2014 to 31 December 2016 (baseline data) from each study city were obtained from the Chinese Center for Disease Control and Prevention (Chinese CDC). Data included age, sex, date of onset, and the city code of residence. All BD cases, including clinical and lab-confirmed cases, were diagnosed based on the China national standard criteria of management for dysentery (NHFPC 2008). The distribution of BD in China has been described previously (Xu et al. 2014).
Daily meteorological data over the same period from each city were downloaded from the CMA Data Sharing Service System (http://cdc.cma.gov.cn/), including mean temperature, relative humidity, and rainfall. Each city was assigned a representative meteorological station according to CMA. Missing meteorological data were interpolated using the mean of the 5 nearest neighbors (Torgo 2011).
Projected daily temperature series for 2010s (2014–2016), 2030s (2034–2036), 2050s (2054–2056), 2070s (2074–2076), and 2090s (2094–2096) were obtained from the Fast Track database of the Inter-Sectoral Impact Model Inter-Comparison Project (ISI-MIP) (Warszawski et al. 2014). The database provides bias-corrected downscaled temperature series projections with a spatial resolution of for each Representative Concentration Pathway (RCP, including RCP 2.6, RCP 4.5, and RCP 8.5) scenario of five general circulation models (GCMs) (Table S2), considered to be representative of the range of future climate projections (Moss et al. 2010; Warszawski et al. 2014). Projected daily temperature series for the 316 cities were extracted. To avoid possible bias, the modeled temperature series were recalibrated using a method developed and applied in ISI-MIP based on the actual and projected temperature data in 2010s (Hempel et al. 2013; Vicedo-Cabrera et al. 2019). Projections of the population of China for current and future periods were downloaded from the United Nations Population Division (https://population.un.org/wpp/).
Statistical Analysis
The data analysis had three steps: estimating the temperature-BD relationship at city, regional and national levels; estimating the attributable risk of BD due to temperature; and projecting the future burden of BD due to increasing temperature in the context of climate change.
Estimating the temperature–BD relationship at city, regional, and national levels.
A two-stage statistical model was used to first assess the city-specific temperature–BD relationship and then to group them to obtain the pooled associations at regional and national levels (Liu et al. 2018; Xiao et al. 2017). At the first stage, a generalized linear model combined with a distributed lag nonlinear model (DLNM) accounting for meteorological factors, long-term trend, and seasonality was fitted to quantify the city-specific exposure–lag response relationship between temperature and BD (Gasparrini et al. 2010). An exploratory analysis using a bidimensional cross-basis natural cubic spline function with 3 degrees of freedom (df) and 21 d of lag based on previous studies was first applied in DLNM (Hao et al. 2019; Zhao et al. 2018). A linear relationship with 14-d lags was finally adopted according to the exploratory analysis (Figure S1). To allow for overdispersion and autocorrelation, a quasi-Poisson distribution was used and the first-order lagged variable of model residual errors was added to the model (Liu et al. 2018). A natural cubic spline with 7 df per year for time was used to control for long-term trend and seasonality (Zhou et al. 2013). The model was described as follows:
| (1) |
where denotes the daily counts of BD on day t. Daily mean temperature was applied with the cross-basis natural cubic spline function () for both response and lag dimension. In addition, ns refers to natural cubic splines. Daily average humidity and rain on day t represented by and were included in the model as potential confounders. The term means the first-order lagged model residuals.
In the second stage, a multivariate meta-analysis of the city-specific estimates was conducted to obtain the overall cumulative exposure–response relationship at regional and national levels (Gasparrini et al. 2012). The best linear unbiased prediction (BLUP) and a Wald test were used to test the significance of meta-predictors and differences between models (Gasparrini et al. 2012). The Akaike information criterion (AIC) was used to measure the goodness of model fits. The multivariate extension of statistics and the Cochran Q test were applied to measure the residual heterogeneity (Gasparrini et al. 2012). To address the difference of temperature range between the 316 cities, we adopted two separate approaches: first a relative scale measurement of temperature (percentiles) for the national level and then an absolute temperature measurement for each climatic region (Gasparrini et al. 2012; Xiao et al. 2017). For the first approach, subgroup analyses by age and sex were conducted after the main model to identify potential vulnerable groups. Age groups of 0–5 y old and old were adopted because BD is more common among the children under 5 y old (Hao et al. 2019). For the second approach, region-specific estimates of the temperature–BD relationship were obtained using an intercept-only model, i.e., not adding any other confounders in the meta-regression model.
Estimating the attributable risk of BD due to temperature.
The attributable fraction of BD due to higher temperature (temperature above the reference, the 50th percentile ) was estimated in the city-specific DLNM-analysis with BLUP method (Gasparrini et al. 2012; Gasparrini and Leone 2014). The attributable risks for all average daily temperatures above the 50th percentile for each city at baseline (in 2014–2016) was estimated with a backward approach (Gasparrini and Leone 2014). Empirical confidence intervals (eCIs) were obtained using Monte Carlo simulations assuming a multivariate normal distribution of the parameters (Gasparrini and Leone 2014). The city-specific excess BD cases attributable to higher temperature were then summed by region to calculate the region-specific attributable fraction.
Projecting the future burden of BD due to increasing temperature in the context of climate change.
To isolate the temperature effect from other important trends, we assumed that populations, adaptation, and exposure–response relationships will remain constant in future (Vicedo-Cabrera et al. 2019). Future excess numbers of BD cases were projected using the of temperature as the reference following a modeling framework tutorial (Vicedo-Cabrera et al. 2019). The equation was described as follows:
| (2) |
where denotes the excess number of BD cases due to temperature. means the modeled BD series in future. and represent the unidimensional overall cumulative exposure–response curves derived from DLNM model. and are, respectively, the modeled future temperature series and the reference temperature.
The excess BD cases were estimated separately for each city under different GCMs, RCPs, and periods; then GCM averaged attributable fractions were computed by region, period, and RCP, using the related total number of BD cases at current as denominator. Empirical CIs were obtained by Monte Carlo simulations (generating 1,000 samples of the coefficients) to quantify the uncertainty in exposure–lag response relationships and climate projections across GCMs (Gasparrini et al. 2017). In addition, other factors, such as the projected changes in population and adaptations, were also estimated. The cohort-component method was used to project population trends until the year 2100 (https://population.un.org/wpp/Methodology/). A 30% decrease in the future temperature–BD exposure–response shape (coefficient, ) was applied to represent adaptation (Vicedo-Cabrera et al. 2019; Gosling et al. 2017).
The sensitivity of main findings at national level was examined. A one-way sensitivity analysis strategy was adopted with respect to a) controlling the autocorrelation of models or not; b) changing the df of natural cubic spline for calendar time; c) varying the confounders for meteorological factors; and d) changing the max lag period. Residual analysis and autocorrelation test were conducted to graphically evaluate the goodness of model fit and autocorrelation.
All analyses were conducted in R (version 3.5.2; R Development Core Team) (http://www.r-project.org), using packages dlnm, tsModel, and mvmeta (Gasparrini 2011; Gasparrini et al. 2012).
Ethical Clearance
This study was approved by the ethical review committee (ERC) of the National Institute for Environmental Health, Chinese CDC (201606), and the ERC of School of Public Health, Shandong University of China (20190402).
Results
Description of the Meteorological and Disease Data
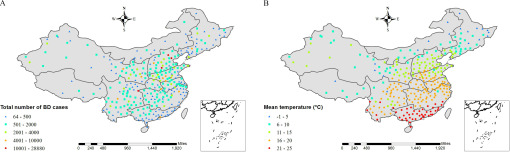
A total of 396,134 BD cases were notified over the period 2014–2016, 99.8% (395,321) of which occurred in the 316 target cities. The western and northern parts of China, including the Northwest region, Tibet, and Inner Mongolia, have sparse populations and relatively fewer BD cases (Figure 2A). The geographic distribution of BD cases varied widely, with most cases occurring in densely populated cities (Figure 2A). There were more BD cases in males (216,842; 55%) than those in females (178,479; 45%), and the most prevalent group was children aged 0–5 y old (139,198; 35%). Temperature in China increases from north to south (Figure 2B). There was a synchronous seasonal trend of BD and temperature, with the most BD cases and higher temperatures occurring from June to September throughout the study period (Figure S2).
Figure 2.
Geographic distribution of total bacillary dysentery cases from 2014 to 2016 (A) and yearly mean temperature (B) from 2014 to 2016 in 316 cities of China.
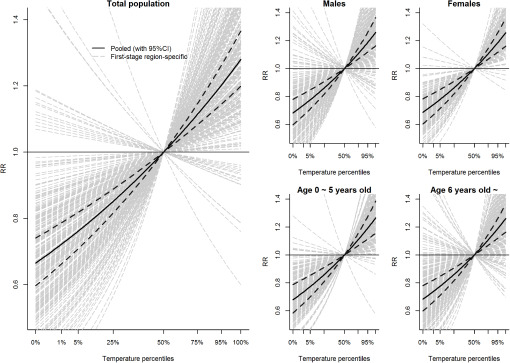
Relationship Between Temperature and BD
Pooled and city-specific temperature–BD relationships for the 316 cities in relative scale for total population, different age groups, and genders are shown in Figure 3. The results suggest a positive linear relationship for the pooled relationship at national level and substantial variation between the city-specific relationships, with an of 35.7% (Q test: ). The subgroup analyses suggest that pooled estimated effect of temperature on BD was similar between age {0–5 y old: relative risk , [95% confidence interval (CI): 1.010, 1.022] vs. : , (95% CI: 1.010, 1.021)} and gender groups [males: , (95% CI: 1.011, 1.022) vs. females: , (95% CI: 1.010, 1.021)] (Figure 3).
Figure 3.
Pooled estimates [with 95% confidence interval (CI)] and city-specific estimate of temperature on bacillary dysentery in relative scale for total population, different age groups, and genders. Reference: 50th percentile of temperature.
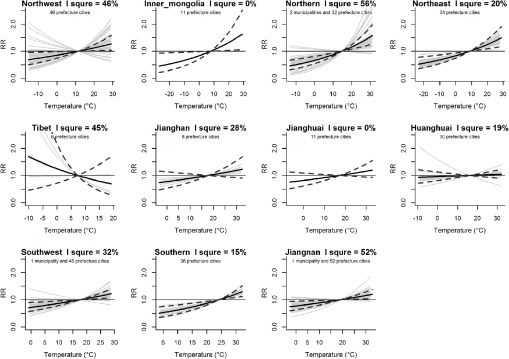
The region-specific temperature–BD relationships (Figure 4) indicated that associations between temperature and BD were similar across cities within Inner Mongolia, Northeast, Jianghuai, Huanghuai, and Southern China regions (), whereas there were moderate levels of heterogeneity across cities within other regions (: ) (Table S3). The risk of BD was significantly increased in association with higher average daily temperatures in the Northwest, Inner Mongolia, Northeast, Northern, Southwest, Jiangnan, and Southern China regions (Table 1, Figure 4). RRs in Table 1 represent the relative risk for a 1°C increase in daily mean temperature. Associations were positive but not significant for Jianghan and Jianghuai and close to the null for Huanghuai. In contrast with other regions, the association was inverse (though not significant) for Tibet.
Figure 4.
Region-specific estimates of mean temperature on bacillary dysentery. Black solid line with dark grey dashed lines represent the regional pooled effect with 95% confidence interval (CI), whereas the solid light grey lines are the city-specific estimates. For Jianghuai and Inner Mongolia, the pooled estimate lines overlie the first-stage estimates.
Table 1.
Risk of bacillary dysentery due to temperature in 11 regions of China.
| Region | RR (95% CI) | RR for adaptation | Attributable fraction (%) |
|---|---|---|---|
| Huanghuai | 1.003 (0.993, 1.013) | 1.002 | 1.9 |
| Inner Mongolia | 1.023 (1.002, 1.043) | 1.016 | 15.7 |
| Jianghan | 1.014 (0.993, 1.035) | 1.010 | 5.6 |
| Jianghuai | 1.012 (0.995, 1.029) | 1.008 | 4.9 |
| Jiangnan | 1.014 (1.003, 1.025) | 1.009 | 4.8 |
| Northeast | 1.021 (1.008, 1.034) | 1.014 | 13.6 |
| Northern | 1.029 (1.015, 1.044) | 1.020 | 12.8 |
| Northwest | 1.014 (1.002, 1.026) | 1.010 | 6.8 |
| Southern | 1.033 (1.015, 1.052) | 1.024 | 6.3 |
| Southwest | 1.019 (1.006, 1.032) | 1.013 | 5.8 |
| Tibet | 0.970 (0.900, 1.046) | 0.979 | |
| National | 1.017 (1.012, 1.021) | 1.012 | 7.0 |
Note: RR represents the regional combined relative risk for a 1°C increase of daily mean temperature derived from the two-stage model during 2014–2016. RR for adaptation used the coefficient () of region-specific relative risks reduced by 30%. Attributable fraction was estimated in the city-specific DLNM-analysis with BLUP method. Higher temperature for attributable fraction means all average daily temperatures above the 50th percentile for each city at baseline (in 2014–2016). BLUP, best linear unbiased prediction; CI, confidence interval; DLNM, distributed lag nonlinear model; RR, relative risk.
Attributable Fraction of BD Due to Temperature
Estimated attributable risks for BD due to average daily mean temperatures above the 50th percentile were the highest for the Inner Mongolia (16%), followed by the Northeast (14%) and Northern (13%) regions (Table 1, Figure 5A). Most of the individual cities in the same regions and most of the cities in the Northwest, Southern, and Southwest regions had high attributable risks () (Figure 5B, Table S4).
Figure 5.
Region-specific (A) and city-specific (B) attributable fraction of bacillary dysentery due to higher temperature in China. Higher temperature means daily temperature above the city-specific 50th percentile from 2014 to 2016. Corresponding numeric data for each region and city are reported in Table 1 and Table S4, respectively.
Projected Future Burden of BD Due to Temperature Increase in the Context of Climate Change
Future temperatures are projected to increase gradually in China for RCP 4.5 and 8.5 but not for RCP 2.6 (Figure S3). The average temperature change in the 2090s compared with the present will exceed 3°C for RCP 4.5 and over 5°C for RCP 8.5 (Table S5). Geographic variation of projected temperature change is not substantial, being slighter higher in the North than in the South of China (Figure S3). According to World Population Prospects 2019 provided by the World Health Organization (WHO), after adopting a medium fertility variant and no change in age structure, we assumed a 3.85% increase in the national population from baseline to the 2030s, followed by decreases of 2.65%, 13.16%, and 22.36% for the 2050s, 2070s, and 2090s, respectively (https://population.un.org/wpp/).
Projected BD had a similar increasing trend for different scenarios and years but a very different geographic variation in comparison with the projected temperature (Figure 6). An increasing trend of BD cases due to average temperature increase was projected in most regions of China, especially for RCP 8.5 (Figure 6). Identified high risk regions are Northern, Northeast, Inner Mongolia, Northwest, and Southern China regions with percent change and 95% CI under RCP 8.5 of 20% (11%, 27%), 15% (6%, 20%), 15% (, 22%), 12% (1%, 19%), and 11% (5%, 15%), respectively, during 2090s in comparison with their current burdens (Table S5). When we performed a sensitivity analysis that assumed a 30% reduction in the exposure–response function to account for adaptation (using the RR for adaptation in Table 1), estimated percentage differences in future BD due to projected temperatures (relative to the reference value) were smaller but remained positive for all regions except Tibet, where there was a smaller net decline relative to the primary estimates (Table S5). When we adjusted for projected changes in the overall population in addition to adaptation, estimated temperature-related changes in BD increased in magnitude for the 2030s (when the projected population increased relative to baseline), but decreased (in some cases below the null) for the 2050s, and indicated a decline in temperature-related BD relative to baseline for all regions in the 2070s and 2090s (Table S5).
Figure 6.
Projected percent change of bacillary dysentery due to temperature increase by scenarios and years in China under assumptions of no change in population sizes and adaptation. Corresponding numeric data are reported in Table S5.
Sensitivity Analysis
Sensitivity analyses were performed to test the robustness of our models. The shape of the association between temperature and BD was similar when controlling autocorrelation or not (Figure S4), adjusting for rain and humidity (Figure S5), changing the df of the natural cubic spline for calendar time (Figure S6), and changing the maximum lag period (Figure S7). We did not observe evidence of autocorrelation, and residuals for the DLNM models followed a normal distribution, as illustrated based on estimates for Beijing, Tianjin, Chongqing, and Shenzhen (Figures S8, S9, S10, and S11, respectively). Results are similar and not shown for other cities.
Discussion
To our knowledge, this is the first epidemiological study to estimate the risk of BD attributable to temperature and to project the future BD burden in the context of climate change at city, regional, and national levels. Our analysis covered approximately 99.8% of the notified BD cases in China over the study period. Our estimates suggested that higher daily average temperature is associated with an increased risk of BD in most regions of China, though associations varied among cities and regions with different climatic characteristics. Our findings also identified regions that may be at particularly high risk of BD as a consequence of increasing temperatures in the future, particularly under the RCP 8.5 scenario. The results will contribute to the development of national preventive strategies and measures for the reduction of likely increasing risks of BD due to climate change in China. The study findings may also be applicable to other countries with similar climate characteristics and socioeconomic status and may also be useful for the control and prevention of other diarrheal diseases.
In this study, we found that high temperature was associated with a significant increase in the risk of BD at national level, which is consistent with the findings of previous single city studies in China (Cheng et al. 2017; Li et al. 2013, 2015; Liu et al. 2019; Ma et al. 2013; Zhang et al. 2008; Zhao et al. 2016). The biological mechanism linking temperature and BD is complex. Shigella can be transmitted through person-to-person contact or by consumption of contaminated food or water (Kotloff et al. 2018). Increasing BD may be explained by changes in the microbes of contaminated food or water driven by increasing temperatures. Higher temperatures can lengthen the survival period and growth rate of microbes (Black and Lanata 1995; Kovats et al. 2004; Mackey and Kerridge 1988). Simultaneously, higher temperature may change human diet and eating habits and behaviors, such as eating more barbecued foods, ice cream, and salads, which increase the exposure to microbes (Kovats et al. 2004). Moreover, people drink more water on hot days, which will dilute the gastric juice and weaken its bactericidal function (Kovats et al. 2004). However, previous theories have not clearly explained the heterogeneity of temperature–BD relationship across different meteorological-geographic regions, which was evident in our analysis despite use of a unified data format and time-series model for all cities in this study. This heterogeneity may partly be due to variation in other social, geographic, and climatic characteristics. Several studies have also suggested that associations among climatic factors and BD and Hand, Foot, and Mouth disease may be modified by characteristics including geographic location, economic factors, and humidity (Guo et al. 2016; Liu et al. 2018, 2019; Zhu et al. 2016). The subgroup analysis suggested that associations between temperature and BD were similar for men and women, and for children 0–5 y old and those old, in contrast with other studies that reported that children ages 0–5 y old and female children were at higher RR than others in Hefei city, China, whereas another multicity study conducted in Anhui province, China, indicated that RR of high temperature for children old was higher than the RR for children under 5 y old (Li et al. 2016; Hao et al. 2019).
Climate change has been recognized as one of the biggest global threats to human health (Watts et al. 2015). Under different RCP scenarios, temperature simulations from GCMs indicate that warming will occur in all regions of China, especially in Northern regions (Xu and Xu 2012). The ensemble-averaged warming in China by the end of the 21st century is for RCP 2.6, for RCP 4.5, and for RCP 8.5 (Xu and Xu 2012). Estimates assuming no adaptation or change in the population suggested that increasing temperatures under the RCP 4.5 and RCP 8.5 scenarios will increase the risk of BD over time in most regions, with the greatest increases by the 2090s (relative to 2014–2016 under RCP 8.5) estimated for the Northern (20%), Northeast (15%), Inner Mongolia (15%), Northwest (12%), and Southern (11%) regions. Such increases could impose a huge additional health burden on China’s already overloaded health-care system. For example, the estimated annual health-care cost for BD in 2014–2016 was for Beijing alone (Jian et al. 2010) and will increase to at 2090s under RCP 8.5. Effective health adaptation strategies and measurements should be developed and implemented to protect population health, especially in these vulnerable regions. Population changes projected by WHO suggest that the overall population in China will decrease by 22% in the 2090s in comparison with that of the 2010s, which would also reduce the numbers of future BD cases accordingly. Another study from China used similar population projection methods from the United Nations with different population variation scenarios to project temperature-related mortality risks (Li et al. 2018). However, population projections may be unreliable due to the influence of changes in population policy and other factors (Xu et al. 2016). The reductions-in-slope method recommended by Simon et al. was conducted in our study to handle the adaptation in the future (Gosling et al. 2017). However, caution should be exercised when explaining the adaptation because it may introduce another source of uncertainty that could be greater than the uncertainty from emissions and climate modeling (Gosling et al. 2017).
Some of the regions estimated to be at higher risk of increased BD due to climate change may also be at increased risk because of insufficient infrastructure, lower socioeconomic status, and health-care service limitations, including the Inner Mongolia, Northeast, and Northern regions. A well-designed health-care plan and resource allocation strategy will be important, together with an effective community health education campaign. Our estimates suggested that, in addition to less-developed regions, Chinese megacities, including Beijing, Tianjin, and Shenzhen, will also have a high risk of temperature-related BD due to climate change. In our analyses, we were not able to account for changes in the structure of city populations, which may include increasing numbers of migrant workers from rural areas who may be at higher risk due to poorer living conditions and health-care services (Hesketh et al. 2008). Steps to reduce future risks of BD should focus not only on populations in less developed areas but also on urban populations, including rural-to-urban migrant workers in megacities.
Some limitations of this study should be acknowledged. First, underreporting is inevitable, although there have been improvements in China (Wang et al. 2006). Second, some confounders like pathogen mutation, individual hygiene habits, and immune levels have not been considered. Last, our model relied on projections of future climate-change scenarios, future population changes, and adaptations that are uncertain and may be affected by a variety of factors, such as government policy and adaptive actions.
Conclusions
Our study supports a positive association between temperature and BD in China, with temperatures above the local median accounting for 13%–16% of the current BD disease burden in high-risk regions, but with weaker or null associations in other regions. Our findings also suggest that global warming will increase BD infections in China as a whole, and in both less-developed and urban areas, thus supporting the need for national strategies to reduce the risk of BD due to climate change.
Supplementary Material
Acknowledgments
We thank the Chinese CDC and the National Meteorological Information Center of China for sharing with us the data required for our study. We acknowledge the modeling groups for providing their data for analysis, the Program for Climate Model Diagnosis and Intercomparison (PCMDI), and the World Climate Research Programme’s (WCRP’s) Coupled Model Intercomparison Project for collecting and archiving the model output and organizing the model data analysis activity.
This work was supported by Special Foundation of Basic Science and Technology Resources Survey of Ministry of Science and Technology of China (2017FY101202). Z.L. was supported by the scholarship from Chinese Scholarship Council (201806220220).
References
- Bardhan P, Faruque AS, Naheed A, Sack DA. 2010. Decrease in shigellosis-related deaths without Shigella spp.-specific interventions, Asia. Emerg Infect Dis 16(11):1718–1723, PMID: 21029529, 10.3201/eid1611.090934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black R, Lanata C. 1995. Epidemiology of Diarrheal Diseases in Developing Countries. New York: Raven Press, 13–36. [Google Scholar]
- Chang Z, Zhang J, Ran L, Sun J, Liu F, Luo L, et al. 2016. The changing epidemiology of bacillary dysentery and characteristics of antimicrobial resistance of shigella isolated in China from 2004–2014. BMC Infect Dis 16(1):685, PMID: 27863468, 10.1186/s12879-016-1977-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng J, Xie MY, Zhao KF, Wu JJ, Xu ZW, Song J, et al. 2017. Impacts of ambient temperature on the burden of bacillary dysentery in urban and rural Hefei, China. Epidemiol Infect 145(8):1567–1576, PMID: 28294081, 10.1017/S0950268817000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A. 2011. Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw 43:1–20, PMID: 22003319. [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2010. Distributed lag non-linear models. Stat Med 29(21):2224–2234, PMID: 20812303, 10.1002/sim.3940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B, Kenward MG. 2012. Multivariate meta-analysis for non-linear and other multi-parameter associations. Stat Med 31(29):3821–3839, PMID: 22807043, 10.1002/sim.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Guo Y, Sera F, Vicedo-Cabrera AM, Huber V, Tong S, et al. 2017. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet Health 1(9):e360–e367, PMID: 29276803, 10.1016/S2542-5196(17)30156-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Leone M. 2014. Attributable risk from distributed lag models. BMC Med Res Methodol 14:55, PMID: 24758509, 10.1186/1471-2288-14-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gosling SN, Hondula DM, Bunker A, Ibarreta D, Liu J, Zhang X, et al. 2017. Adaptation to climate change: a comparative analysis of modeling methods for heat-related mortality. Environ Health Perspect 125(8):087008, PMID: 28885979, 10.1289/EHP634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo C, Yang J, Guo Y, Ou QQ, Shen SQ, Ou CQ, et al. 2016. Short-term effects of meteorological factors on pediatric hand, foot, and mouth disease in Guangdong, China: a multi-city time-series analysis. BMC Infect Dis 16(1):524, PMID: 27682137, 10.1186/s12879-016-1846-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao Y, Liao W, Ma W, Zhang J, Zhang N, Zhong S, et al. 2019. Effects of ambient temperature on bacillary dysentery: a multi-city analysis in Anhui province. China Sci Total Environ 671:1206–1213, 10.1016/j.scitotenv.2019.03.443. [DOI] [PubMed] [Google Scholar]
- Hempel S, Frieler K, Warszawski L, Schewe J, Piontek F. 2013. A trend-preserving bias correction—the ISI-MIP approach. Earth System Dynamics 4(2):219–236, 10.5194/esd-4-219-2013. [DOI] [Google Scholar]
- Hesketh T, Jun YX, Lu L, Mei WH. 2008. Health status and access to health care of migrant workers in China. Public Health Rep 123(2):189–197, PMID: 18457071, 10.1177/003335490812300211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jian L, Huan-yu W, Bao-ke G, Yan-ting L, Hui-ming J. 2010. Disease economic burden associated with bacillary Shigeliosis in Shanghai. Chinese J Epidemol 31:1196–1197, . [DOI] [Google Scholar]
- Kotloff KL, Riddle MS, Platts-Mills JA, Pavlinac P, Zaidi A. 2018. Shigellosis. Lancet 391(10122):801–812, 10.1016/S0140-6736(17)33296-8. [DOI] [PubMed] [Google Scholar]
- Kovats RS, Edwards SJ, Hajat S, Armstrong BG, Ebi KL, Menne B. 2004. The effect of temperature on food poisoning: a time-series analysis of salmonellosis in ten European countries. Epidemiol Infect 132(3):443–453, PMID: 15188714, 10.1017/s0950268804001992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li K, Zhao K, Shi L, Wen L, Yang H, Cheng J, et al. 2016. Daily temperature change in relation to the risk of childhood bacillary dysentery among different age groups and sexes in a temperate city in China. Public Health 131:20–26, PMID: 26655018, 10.1016/j.puhe.2015.10.011. [DOI] [PubMed] [Google Scholar]
- Li T, Horton RM, Bader DA, Liu F, Sun Q, Kinney PL. 2018. Long-term projections of temperature-related mortality risks for ischemic stroke, hemorrhagic stroke, and acute ischemic heart disease under changing climate in Beijing, China. Environ Int 112:1–9, PMID: 29241068, 10.1016/j.envint.2017.12.006. [DOI] [PubMed] [Google Scholar]
- Li Z, Wang L, Sun W, Hou X, Yang H, Sun L, et al. 2013. Identifying high-risk areas of bacillary dysentery and associated meteorological factors in Wuhan, China. Sci Rep 3:3239, PMID: 24257434, 10.1038/srep03239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li ZJ, Zhang XJ, Hou XX, Xu S, Zhang JS, Song HB, et al. 2015. Nonlinear and threshold of the association between meteorological factors and bacillary dysentery in Beijing, China. Epidemiol Infect 143(16):3510–3519, PMID: 26027678, 10.1017/S0950268815001156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z, Liu Y, Zhang Y, Lao J, Zhang J, Wang H, et al. 2019. Effect of ambient temperature and its effect modifiers on bacillary dysentery in Jinan, China. Sci Total Environ 650(pt 2):2980–2986, PMID: 30373074, 10.1016/j.scitotenv.2018.10.053. [DOI] [PubMed] [Google Scholar]
- Liu Z, Zhang F, Zhang Y, Li J, Liu X, Ding G, et al. 2018. Association between floods and infectious diarrhea and their effect modifiers in Hunan province, China: a two-stage model. Sci Total Environ 626:630–637, PMID: 29396332, 10.1016/j.scitotenv.2018.01.130. [DOI] [PubMed] [Google Scholar]
- Ma W, Sun X, Song Y, Tao F, Feng W, He Y, et al. 2013. Applied mixed generalized additive model to assess the effect of temperature on the incidence of bacillary dysentery and its forecast. PLoS One 8(4):e62122, PMID: 23637978, 10.1371/journal.pone.0062122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackey B, Kerridge A. 1988. The effect of incubation temperature and inoculum size on growth of salmonellae in minced beef. Int J Food Microbiol 6(1):57–65, PMID: 3079462, 10.1016/0168-1605(88)90085-2. [DOI] [PubMed] [Google Scholar]
- Moss RH, Edmonds JA, Hibbard KA, Manning MR, Rose SK, van Vuuren DP, et al. 2010. The next generation of scenarios for climate change research and assessment. Nature 463(7282):747–756, PMID: 20148028, 10.1038/nature08823. [DOI] [PubMed] [Google Scholar]
- NHFPC (National Health and Family Planning Commission). 2008. Ws 287-2008. Diagnostic Criteria and Principles of Management of Bacillary and Amebic Dysentery. [Chinese]. http://www.nhc.gov.cn/wjw/s9491/200802/39040/files/9c939b0b5de04a14be37e02421adc661.pdf [accessed 21 May 2020]. [Google Scholar]
- Torgo L. 2011. Data Mining with R: Learning with Case Studies. Boca Raton, FL: Chapman and Hall/CRC. [Google Scholar]
- Vicedo-Cabrera AM, Sera F, Gasparrini A. 2019. Hands-on tutorial on a modeling framework for projections of climate change impacts on health. Epidemiology 30(3):321–329, PMID: 30829832, 10.1097/EDE.0000000000000982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang XY, Tao F, Xiao D, Lee H, Deen J, Gong J, et al. 2006. Trend and disease burden of bacillary dysentery in China (1991–2000). Bull World Health Organ 84(7):561–568, PMID: 16878230, 10.2471/blt.05.023853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warszawski L, Frieler K, Huber V, Piontek F, Serdeczny O, Schewe J. 2014. The inter-sectoral impact model intercomparison project (ISI-MIP): project framework. Proc Natl Acad Sci USA 111(9):3228–3232, PMID: 24344316, 10.1073/pnas.1312330110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watts N, Adger WN, Agnolucci P, Blackstock J, Byass P, Cai W, et al. 2015. Health and climate change: policy responses to protect public health. Lancet 386(10006):1861–1914, 10.1016/S0140-6736(15)60854-6. [DOI] [PubMed] [Google Scholar]
- Wu X, Lu Y, Zhou S, Chen L, Xu B. 2016. Impact of climate change on human infectious diseases: empirical evidence and human adaptation. Environ Int 86:14–23, PMID: 26479830, 10.1016/j.envint.2015.09.007. [DOI] [PubMed] [Google Scholar]
- Xiao X, Gasparrini A, Huang J, Liao Q, Liu F, Yin F, et al. 2017. The exposure-response relationship between temperature and childhood hand, foot and mouth disease: a multicity study from mainland China. Environ Int 100:102–109, PMID: 28069250, 10.1016/j.envint.2016.11.021. [DOI] [PubMed] [Google Scholar]
- Xu C, Xu Y. 2012. The projection of temperature and precipitation over China under RCP scenarios using a CMIP5 multi-model ensemble. Atmos Oceanic Sci Letts 5(6):527–533, 10.1080/16742834.2012.11447042. [DOI] [Google Scholar]
- Xu Z, Hu W, Zhang Y, Wang X, Tong S, Zhou M. 2014. Spatiotemporal pattern of bacillary dysentery in China from 1990 to 2009: what is the driver behind? PLoS One 9(8):e104329, PMID: 25093593, 10.1371/journal.pone.0104329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X, Zuo H, Rao Y, Zhang L, Wang LL, Zhao Y. 2016. Intention to have a second child among Chinese women one year after the implementation of selective two-child policy: a cross-sectional survey. Lancet 388:S96, 10.1016/S0140-6736(16)32023-2. [DOI] [Google Scholar]
- Yan L, Wang H, Zhang X, Li MY, He J. 2017. Impact of meteorological factors on the incidence of bacillary dysentery in Beijing, China: a time series analysis (1970–2012). PLoS One 12(8):e0182937, PMID: 28796834, 10.1371/journal.pone.0182937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Bi P, Hiller JE. 2008. Weather and the transmission of bacillary dysentery in Jinan, northern China: a time-series analysis. Public Health Rep 123(1):61–66, PMID: 18348481, 10.1177/003335490812300109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Bi P, Hiller JE. 2010. Climate variations and salmonella infection in Australian subtropical and tropical regions. Sci Total Environ 408(3):524–530, PMID: 19922981, 10.1016/j.scitotenv.2009.10.068. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Bi P, Hiller JE, Sun Y, Ryan P. 2007. Climate variations and bacillary dysentery in northern and southern cities of China. J Infect 55(2):194–200, PMID: 17258812, 10.1016/j.jinf.2006.12.002. [DOI] [PubMed] [Google Scholar]
- Zhao Q, Li S, Cao W, Liu DL, Qian Q, Ren H, et al. 2018. Modeling the present and future incidence of pediatric hand, foot, and mouth disease associated with ambient temperature in mainland China. Environ Health Perspect 126(4):047010, PMID: 29681142, 10.1289/EHP3062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, Zhu Y, Zhu Z, Qu B. 2016. Association between meteorological factors and bacillary dysentery incidence in Chaoyang city, China: an ecological study. BMJ Open 6(12):e013376, PMID: 27940632, 10.1136/bmjopen-2016-013376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X, Zhou Y, Chen R, Ma W, Deng H, Kan H. 2013. High temperature as a risk factor for infectious diarrhea in Shanghai, China. J Epidemiol 23(6):418–423, PMID: 23994865, 10.2188/jea.je20130012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L, Wang X, Guo Y, Xu J, Xue F, Liu Y. 2016. Assessment of temperature effect on childhood hand, foot and mouth disease incidence (0-5 years) and associated effect modifiers: a 17 cities study in Shandong province, China, 2007–2012. Sci Total Environ 551–552:452–459, PMID: 26891011, 10.1016/j.scitotenv.2016.01.173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.