Abstract
In recent years, respiratory infectious diseases had continued to attack China, the recent outbreak of COVID-19 pneumonia had attracted worldwide attention. Through studying the literature, interpreting official documents, analyzing medical and social management data, we summarized and compared some powerful measures taken by the Chinese government, such as declaring emergency state, blocking down the epidemic center, prohibiting crowd gathering activities, forcing residents to wear masks, and mobilizing medical staff and products. We found that these unconventional measures, on the one hand, controlled the spread of the epidemic in China, and on the other hand, exposed some of China’s shortcomings in biosafety, food safety, public health input, and emergency system construction. This paper also recommends that other countries should take strict isolation measures as early as possible when fighting COVID-19 epidemics, and also mobilize citizens to strengthen self-protection.
Keywords: COVID-19, anti-epidemic, risk, legality
Introduction
In December 2019, the Health Department of Wuhan City, Hubei Province, China, received hospital reports, showing an unexplained pneumonia from the traditional market“South China Seafood City”. The earliest case was on December 8, 2019.1 Later, some research institutions predicted that the pneumonia perhaps caused by a new virus.2
During this period, due to the Spring Festival holiday and other factors, there had been a large-scale and nationwide population flow, there were also a large number of commercial and cultural activities in China, and the spread of the virus was amazing. On January 20, 2020, Chinese National Health Commission organized a high-level expert panel to visit Wuhan. The panel confirmed that it was a serious respiratory infectious disease, with the patient size and infectious power no less than that of SARS.3 World Health Organization also issued warning.4 So far, the COVID-19 pneumonia was fully exposed. Then, the epidemic had spread to all provinces in Mainland China and Hong Kong, Macao and Taiwan, at least 84,385 Chinese people had been diagnosed and 4643 had died, and it was difficult to estimate the number of asymptomatic patients accurately.5 Relying on the government’s coercive disease control and the cooperation of residents, China’s epidemic had been quickly alleviated. In this paper, we would describe and evaluate these emergency measures, and discuss how one can promote these measures upgrading to optimization measures that should be more in line with the requirements of the rule of law and the public health.
Materials and Methods
From January to April 2020, China experienced four periods of incubation, outbreak, control and decline of COVID-19 pneumonia. Government, centers for disease control and prevention, hospitals, scientific institutions and pharmaceutical manufacturers constituted a more united action team to fight against the epidemic. Among them, the Chinese government was the main action planner and strong promoter. We collected government executive orders, press conference speeches, health department statistics, case reports, and official media news during this period to analyzed unconventional administrative measures. We mainly study and discuss through the combination of time axis and policy axis methods.
Results
Why Did the Chinese Government Response Slowly at the Early Stage of the Outbreak
Looking back to observe the epidemic, the time when the Chinese government had been truly alerted and taken action was late January 2020, but before this time point the epidemic had been lurking in the crowd for more than a month.6 Through some news reports and statistical data, as well as some local official statements from Hubei Province, we regret to see the decision-making hesitation phenomenon of the Chinese government. We found that two factors may have influenced the Chinese government’s decision.
The First Factor Was Lack of Knowledge of COVID-19 Pneumonia
At that time, it was impossible to confirm the key issues of the virus sub-type, pathogenesis, mode of transmission, speed of transmission, etc.7 So Wuhan Health Department thought that COVID-19 pneumonia was similar to ordinary flu, can be prevented and controlled by conventional means, such as maintaining indoor air circulation, avoiding to visit closed, airless public places.8 Some researchers suggested that the COVID-19 virus was likely to have interpersonal communication ability,9 but the opinion was not officially accepted. Until January 9, 2020, Chinese Center for Disease Control and Prevention announced for the first time that the pathogen was preliminarily determined as a new type of coronavirus.10
The Second Factor Has Underestimated the Infection Risk of COVID-19 Pneumonia
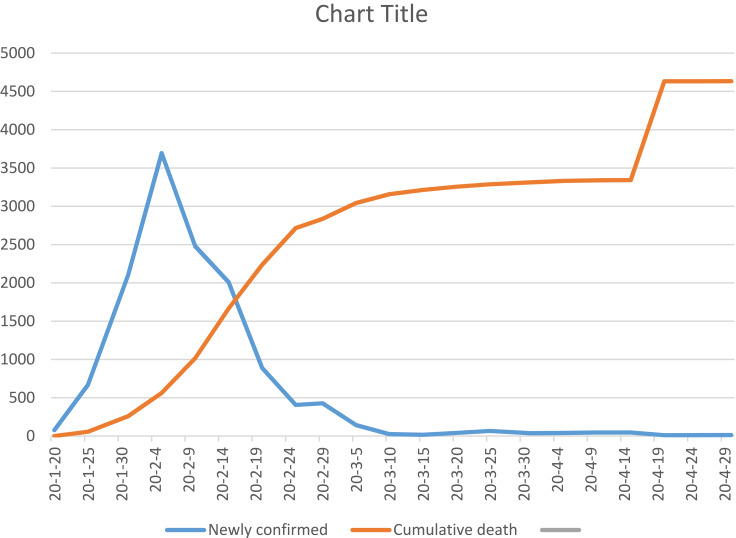
Wuhan Municipal Government was not failing to take control measures, but the selected measures were not thorough. The government only decided to close the seafood market where patients were first identified, but they did not keep isolation measures to close contacts. Wuhan Health Department ordered infectious disease specialist hospitals to treat such patients, but the number of ward and equipment of these special hospitals was not enough. The government recommended that citizens with symptoms of cough and fever wear masks when going out, but there was no restriction on their movement, nor the ability to conduct a comprehensive virus detection on them.11 With the passage of time, the risk of out-of-control conditions had increased significantly from January to March, 2020 (Figure 1).
Figure 1.
Growth trend of COVID-19 epidemic.
Which Emergency Measures Had The Chinese Government Formulated at the Peak of Outbreak
After the medical community made a preliminary judgment that the danger of the COVID-19 pneumonia was very similar to SARS in 2003, the public began to panic, the international community also paid close attention to China’s epidemic. The Chinese government launched a series of emergency measures to respond to the challenges of the epidemic. We observed from the perspectives of policy texts, implementation efforts, investment of resources, and the severity of accountability, found that the intensity of these measures was unconventional. These emergency measures can be divided into several aspects:
The First Category Was Emergency Mobilization Measures Within Government
On January 20, 2020, the Chinese government announced that COVID-19 pneumonia had already been added as Class B infectious disease, and upgraded the control class as same as the standards of Class A infectious diseases.12 According to the Chinese “Provisions On The Prevention And Control Of Infectious Diseases”, there were only two kinds of Class A infectious diseases: plague and cholera.
China’s Central Government, Provinces Governments and Counties Governments all setup headquarters for the COVID-19 pneumonia epidemic, all of the Provinces in Mainland China launched “Level I” public health emergencies response.13 In accordance with “Emergency Response Law”, “National General Emergency Plan for Public Emergencies”, “Regulations on Public Health Emergencies”, and “National Emergency Plan for Public Health Emergencies”, “Level I” response meant that government was authorized to mobilize and expropriate all kinds of personnel, materials, transportation and related facilities to block the epidemic area, to restrict or stop the market, assembly, theater performance and other group gathering activities, to declare the suspension of work, business and class. This high-level authorization allowed government officials to take various powerful measures.
The Second Category Was to Block Down Cities and Communities
From January 23, 2020, Wuhan Municipal Government issued an order to suspend the operation of public transport (including bus, subway, ferry and taxi), airport, railway station and highway were temporarily closed, banned citizens from entering and leaving Wuhan, warned citizens not going out in addition to medical needs and sourcing food.14
Other cities had also followed Wuhan’s example in implementing different levels of traffic control, canceled all kinds of dinner parties, commercial and sports activities, religious activities. People who went to public places were required to wear masks and check the temperature. Enterprises and other institutions are required to extend the Spring Festival holiday to avoid workplace infection.
The Third Category Was Nationwide Medical Mobilization
In order to encourage patients to see doctor in time, the Chinese government announced that the medical expenses for the COVID-19 Pneumonia would be mainly borne by the medical insurance and government. At that time, Wuhan could only provide about 4000 beds for COVID-19 pneumonia patients. The Chinese government decided to construct two makeshift hospital within 15 days, especially for the treatment of severe patients. One of which had a building area of 60,000 square meters (Leishenshan Hospital), with 1600 beds, another hospital (Huoshenshan Hospital) had a building area of 33,900 square meters and 1000 beds, negative pressure medical equipment and external respiratory support equipment had been equipped to the hospitals.15 Wuhan Municipal Government expropriated gym and bus station to build 14 shelter hospitals which usually used in the war, can provide 20,000 beds for patients with mild illness.16 Wuhan government also expropriated hotels and university student apartments to isolate thousands of suspected fevers and close contacts.17 Due to the rapid increase of patients and the shortage of medical staff of Wuhan Municipal and Hubei Province, the Chinese government decided to dispatch military medical personnel, requiring other provinces to send medical support teams. At present, 54,000 doctors and nurses have been added to assistant.18
Other cities had resumed “fever clinics”, and designated special hospitals to treat patients with fever and other suspected symptoms. Besides confirmed patients, residents with Wuhan’s living history, travel history and contact history should be tracked, observed and isolated. Starting from April 2020, citizens returning to China from abroad had to also undergo medical examination and isolation.19
The Fourth Category Was to Provide Financial Support and Preferential Policies to Medical Community and Pharmaceutical Industry
In order to reveal the true face of the virus and find the inhibition method, the Chinese government had approved high quota of R&D support fund, convened research teams from Chinese Academy of Sciences, Chinese Academy of Medical Sciences and various universities to seize the time for virus tracing, drug selecting, vaccine and test reagent developing.20 Rely on these support, some researches completed the full gene sequence of the new coronavirus,21 achieved prokaryotic and eukaryotic expression of new coronavirus related antigen proteins.22 Some researchers found that IFN-α, lopinavir and ritonavir, new nucleoside analogues, antiviral drugs such as remdesivir and cyclophilin inhibitors could be used.23 Some experts recommended traditional Chinese medicine prescriptions.24 Pharmaceutical companies had developed 7 kinds of COVID-19 detection kits, two COVID-19 vaccines had entered clinical trials phase.25
In order to solve the shortage of medical materials, the Chinese National Medical Products Administration had opened green approval channel for manufacturers of COVID-19 medical supplies, financial and tax authorities had provided loans and tax reduction support for manufacturers. After policy stimulus, China’s medical production capacity had expanded rapidly. Currently, it can produce 200 million medical masks, 3.4 million N95 masks, and 1.5 million protective suits per day.26
The Fifth Category Was Comprehensive Publicity of Prevention and Treatment Knowledge
In terms of helping diagnosis and treatment, Chinese National Health Commission had revised and published seven versions of the “Diagnosis and Treatment plan for Pneumonia with COVID-19”27 which stipulated the etiology and epidemiological characteristics, clinical symptoms, diagnostic criteria, clinical classification, treatment methods, discharge criteria, patient isolation and transport criteria of the disease.
To guide residents to prevent COVID-19 Pneumonia, China Center for Disease Control and Prevention has issued eight “Public Prevention Guidelines For COVID-19 Pneumonia”, divided into general prevention, tourism prevention, family prevention, public place prevention, public transportation prevention, home observation, home isolation, nursing homes prevention.28 China Center for Disease Control and Prevention also issued two versions of “Plan for Prevention and Control of Pneumonia Caused by New Coronavirus”. The specific contents include monitoring pneumonia cases, epidemiological investigation, suspected exposed persons and close contacts management, specimen collection and transportation, laboratory testing technical guide, medical personnel training, etc.,29 These public health Knowledge had increased the confidence of medical institutions and residents.
How to View the Effectiveness of These Unconventional Measures
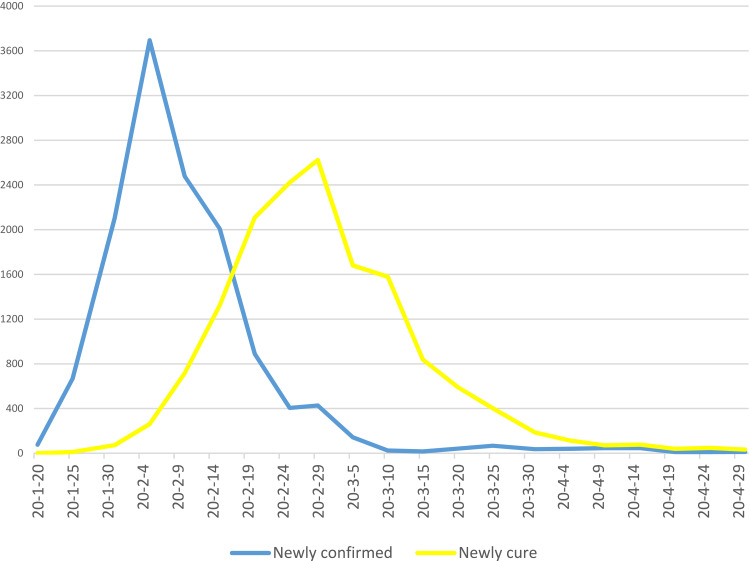
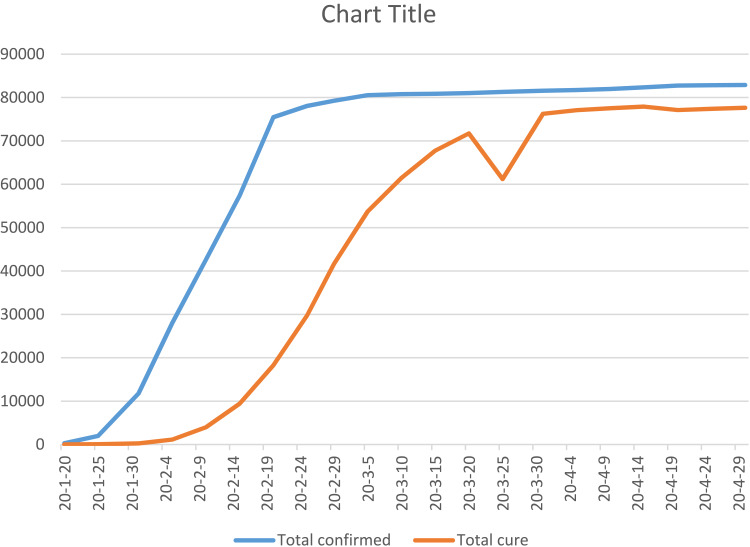
In recent years, the incidence of respiratory infectious diseases in China had been high, the control measures which the Chinese government taken were relatively mild, but during the COVID-19 pneumonia epidemic, various unconventional measures were put on the table. It should be admitted that with the support of these measures and the tenacious efforts of medical staff, China had rapidly treated more than 80,000 patients. The number of new cases per day in China had begun to decline steadily, the number of cure cases were growing, the virus did not break out in other big cities in China outside Wuhan (Figures 2 and 3). From public health perspective, China ’s measures had two major highlights:
Figure 2.
COVID-19 epidemic control efficiency.
Figure 3.
Progress in COVID-19 epidemic control.
The First Highlight Was Resolute Isolation
In the control of infectious diseases, the traditional sequence was to detect and confirm the infected people firstly, then took isolation and treatment measures. However, in the absence of scientific analysis of the virus and the ability to conduct large-scale detection, the Chinese government had skipped the virus detection stage and adopted extreme method directly, that was decided to isolate more than 14 million citizens in Wuhan, whether they were healthy or at high risk of infection. The design principles of isolation mechanism were: first of all, assuming that Wuhan was the only focus of the epidemic, cut off the flow of people in Wuhan could prevent the virus from being brought to other places and abroad. Secondly, the existing population in Wuhan might be divided into healthy people, suspected infected people and infected people. For healthy people, if they did not go out and took protective measures at home, they will not have access to the infected people and can avoid infection. For those suspected of infection, the general incubation period is 3–15 days. They should be isolated and observed at home. If they got sick, they should go to the hospital. If they did not get sick, they would be out of the risk of infection. For the infected people, local government would try to get them all treated. Although this kind of large-scale isolation measure was very chaotic at the beginning, the Chinese government still insisted on carrying out it and achieved the desired effect.
The Second Highlight Was That Chinese Government Had Successfully Persuaded People to Abide Mandatory Administrative Measures
There were two possible reasons. One was that SARS had broken out in China in 2003, many people were more afraid of similar infectious diseases. They consciously put on masks and reduced going out. On the other hand, the Chinese government used policemen, civil servants and community managers to inspect public places, monitor traffic, and force work stoppages. People had no place to go, so they can only reduce social activities according to government requirements.
Ancient Roman author Phaedrus once wrote “If you draw the bowsrting too tight, your bow will soon break”. During the COVID-19 epidemic, China also had paid great cost for these unconventional measures. Industry, commerce and transportation had been suspended for up to 3 months. It was expected that a number of SME enterprises would bankrupt and many people would lose their jobs, direct economic losses and long-term impacts were difficult to estimate. Some hospitals were forced to stop due to epidemic, making residents with ordinary diseases very passive. More than 3000 medical staff were infected at work, and at least 14 medical staff died.30 Due to insufficient detection capacity at the beginning of the outbreak, and the diagnosis criteria established by the Chinese National Health Commission did not consider patients with positive nucleic acid tests but no fever, so the number of asymptomatic infections in China were still difficult to estimate.
Discussion
Through this epidemic, we had not only seen the active efforts of the Chinese government but also perceived the “window-breaking effect” of the Chinese public health system at the deeper level. These system should be upgraded and optimized from the following aspects:
Food Safety Risk Management Should Enforce Before Medical Treatment
Food safety was the root of disease eradication. In recent years, China had revised “Food Safety Law”, which provided for more severe penalties, but there was a gap between legislation and real life. First, China had a large population base, increasing consumer demand, and the Chinese government strictly controlled the price of food. In order to reduce costs, some animal and plant breeders tried to increase the breeding density, shorten the breeding time, and even abuse the growth hormones and antibiotics, make food unsafe. Secondly, according to Article 34 of the “Food Safety Law”, any meat product that failed to be quarantined or failed to pass the quarantine inspection or failed to pass the inspection shall be banned from sale, but this did not cover completely. Law enforcement agencies mainly inspected shopping malls and supermarkets, while a large number of food in the retail market and wholesale market, unpacked food and non-standard food were difficult to supervise, the COVID-19 outbreak happened just in the traditional market. Thirdly, the COVID-19 pneumonia was highly suspected to be related to the wild animals. As for edible wild animals, China had some bad traditions, which were even regarded as a kind of pride by some affluent social classes. For this reason, a huge illegal animal sales chain had been formed and hard to get rid of it. Fourth, the food safety regulatory force was weak in the face of the crisis. Before 2018, China Food and Drug Administration (CFDA) was also responsible for the supervision of food and drugs. After 2018, CFDA was changed into the National Medical Products Administration (NMPA), which gave the authority of food supervision to the State Administration for Market Regulation, that may cause a regulatory gap. Chinese Ministry of Agriculture and Rural Affairs was in charge of protecting and supervising wild animals, but they mainly focused on the capture, breeding and other links, less focusing market trading activities. According to the “Food Safety Law”, the Chinese government had set up the National Food Safety Committee, but this Committee still needed more powerful measures when implementing cross-sector issues involving various links of the food industry chain, such as food safety risk assessment and food source traceability system.
Environmental Safety Was an Important Variable in the Prevention of Infectious Diseases Outbreak
Taking Wuhan, the outbreak center of COVID-19 pneumonia, as an example. Wuhan was the capital of Hubei Province. In recent years, the permanent population of Wuhan had reached 11 million, and the floating population was about 3 million, accounting for 23.6% of the total population of Hubei Province. Wuhan was an urban area with more people and less land, with a population density of 1284.42 people/km2. The COVID-19 pneumonia broke out in Jianghan District, the old urban area of Wuhan, with a population density of 13,892 people/km2. In 2019, Wuhan’s gross domestic product (GNP) reached 160 million yuan, accounting for more than one-third of Hubei Province.31 As a super city, Wuhan had great pressure on air quality, urban water use, pollution discharge, epidemic prevention, etc., especially in the old urban areas, it was also faced with problems such as land use progress, living space relief, public facilities supporting renewal, etc. In the early stage, the Chinese government proposed to control the scale of large cities, and improving the level of public health services in cities, however the realization of these ideas also required more precise planning and sufficient investment.
Risk from Imbalance of Public Health Resources Need to Be Actively Filled
In recent years, some changes had taken place in China’s medical reform and medical security, the construction of hospitals was growing, but the community health institutions had not reached the level of healthy development and self-sustaining. People still liked to go to large hospitals and find high-level doctors–even very small common diseases. There were two tendencies in large hospitals. One was that the investment in cardiovascular, tumor and other departments were very large, which was related to the rapid rise in the incidence of cardiovascular disease, diabetes and tumor after China’s rapid prosperity. The equipment of these departments were very advanced, while the development of respiratory and infectious diseases departments was slow, because the per capita medical cost of such patients was not high. Another trend was that doctors in hospitals need to undertake not only diagnosing and treating, but also scientific research work. A large number of doctors spent a lot of energy on research and statistics cases and publish medical papers for income and promotion. As commented by foreign organizations, the Chinese medical community were impatient with the continuous research on the virus. After the SARS in 2003, the research on the virus had no longer be carried out. Some Chinese doctors’ papers published in international academic journals had also been largely withdrawn due to the problem of academic integrity.
The efficiency of the health management system was worth discussing, too. After 2003, in order to solve the problem of the weak and low level of infectious diseases departments in hospitals, the Chinese government decided to expand disease control and prevention center, to manage the infectious diseases in a unified way, and required that the confirmation, information release, diagnosis and treatment specifications, scientific research of all infectious diseases should be undertaken by the center. In the Chinese Centers for Disease Control and Prevention and some Provinces’ Branch Centers, the research teams and research capabilities were very strong, but the medical strength was relatively weak in the cites and counties branch centers, they had not enough doctors and wards to treat patients, usually, they mainly focused on vaccine distribution, infectious disease quantity report, etc. This kind of system cannot achieve one-stop reception and treatment, which would definitely affect the efficiency of the rapid epidemic. The second problem came from hospitals management system. With the development of China’s health reform, some hospitals had been transformed into affiliated hospitals of universities, which were managed by universities instead of local health departments. This caused two predicament: Firstly, when patients increased, alternative options were to vacate wards or even changed the whole hospital into an isolation center, but this needed to be negotiated by the three parties of university, hospital and health department. Secondly, in the allocation of medical materials urgently needed for the infectious diseases, the health departments of local governments would first consider the needs of hospitals under their direct management, and then other types of hospitals. After the outbreak of the epidemic, some hospitals cannot apply for medical materials from their superiors in time, so they can only choose social and enterprise assistance. As a result, the public opinion criticized the emergency materials reserve of the government.
Conclusion
This study found that when Chinese government faced an unfamiliar and terrible epidemic, it was initial hesitation in decision-making, but quickly adopted unconventional measures, such as large-scale blockade of cities, cessation of economic and social activities, obliged residents staying at home, treated patients without regard to cost to reduce the epidemic. However, if the foundation of the public health system was not strong enough, this set of unconventional measures cannot be used for a long time. The optimal choice was that when similar epidemic came, instead of hasty decision-making, a clear legal framework should be established, more mature legal rules such as law on prevention of infectious diseases, law on food and drug safety, law on emergency state and law on promotion of public health should be established to solve the problem, transparency and technological level should be increased, too.
Acknowledgments
This research was sponsored by KC Wong Magna Fund in Ningbo University.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Chinese Center for Disease Control and Prevention. Epidemic update and risk assessment of 2019 Novel Coronavirus. Available from: http://www.chinacdc.cn/yyrdgz/202001/P020200128523354919292.pdf. Accessed February10, 2020.
- 2.Cheng ZJ, Shan J. 2019 Novel coronavirus: where we are and what we know. Infection. 2020;48:155–163. doi: 10.1007/s15010-020-01401-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed February1, 2020.
- 5.Chinese National Health Commission. Epidemic notification. Available from: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml. Accessed May5, 2020.
- 6.Tan WJ, Zhao X, Ma XJ, et al. A novel coronavirus genome identified in a cluster of pneumonia cases—Wuhan, China. 2019−2020. China CDC Weekly. 2020;2(4):61–62. [PMC free article] [PubMed] [Google Scholar]
- 7.Yang, M.Zhao J, Zhang, Z. More than pneumonia, the potential occurrence of multiple organ failure in 2019 novel coronavirus infection. SSRN Electronic Journal, January 2020. doi: 10.2139/ssrn.3532272 Available from: https://ssrn.com/abstract=3532272. Accessed February5, 2020. [DOI]
- 8.Wuhan Municipal Health Commission. Report of viral pneumonia of unknown cause. Available from: http://www.nhc.gov.cn/xcs/yqtb/202001/1beb46f061704372b7ca41ef3e682229.shtml. Accessed February1, 2020.
- 9.Ji W, Wang W, Zhao X, et al. Cross species transmission of the newly identified coronavirus 2019-nCoV. J Med Virol. 2020;92:433–440. doi: 10.1002/jmv.25682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhu N, Zhang DY, Wang WL, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hubei Province Health Commission. Novel coronavirus infection pneumonia knowledge of health science. Available from: http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/jkkp/202001/t20200121_2013874.shtml. Accessed February1, 2020.
- 12.Chinese National Health Commission. Announcement. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml. Accessed February1, 2020.
- 13.Information Office of the Chinese State Council. First level response to public health emergencies in 31 provinces of mainland China. Available from: http://china.caixin.com/2020-01-29/101509411.html. Accessed February1, 2020.
- 14.Wuhan Municipal Government. Announcement of novel coronavirus infection prevention command headquarters in Wuhan. Available from: http://jyh.wuhan.gov.cn/pub/whs_70/zwgk/tzgg/202003/t20200316_972434.shtml. Accessed February1, 2020.
- 15.Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11209&gecstype=1. Accessed February1, 2020.
- 16.Chen SM, Zhang ZJ, Yang JT, et al. Fangcang shelter hospitals: a novel concept for responding to public health emergencies. Lancet. 2020;395(10232):1305–1314. doi: 10.1016/S0140-6736(20)30744-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11234&gecstype=1. Accessed February18, 2020.
- 18.Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11211&gecstype=1. Accessed February1, 2020.
- 19.Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11295&gecstype=1. Accessed April13, 2020.
- 20.Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11266&gecstype=1. Accessed March20, 2020.
- 21.Cai G. Bulk and single-cell transcriptomics identify tobacco-use disparity in lung gene expression of ACE2, the receptor of 2019-nCov. medRxiv. 2020. doi: 10.20944/preprints202002.0051.v3 Available from: https://www.medrxiv.org/content/medrxiv/early/2020/02/17/2020.02.05.20020107.full.pdf. Accessed February10, 2020. [DOI]
- 22.Zhao Y, Zhao Z, Wang Y, et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv. 2020. doi: 10.1101/2020.02.11.20022228 Available from: https://www.biorxiv.org/content/10.1101/2020.01.26.919985v2.full.pdf. Accessed February10, 2020. [DOI]
- 23.Richardson P, Griffin I, Tucker C, et al. Baricitinib as potential treatment for 2019-nCoV acute respiratory disease. Lancet. 2020;395(10223):30–31. doi: 10.1016/S0140-6736(20)30304-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.HuiDS IAE, Madani TA, Ntoumi F, et al. The continuing 2019-nCoV epidemic threat of novel coronavirus to global health: the latest 2019 novel coronavirus outbreak in Wuhan, China. Int J Infect Dis. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li L, Jiao H. Fully guarantee the supply and quality safety of drugs and medical devices for epidemic prevention and control. Qiushi. 2020;7:40–43. [Google Scholar]
- 26.Chinese National Medical Products Administration. Press conference record. Available from: http://www.nmpa.gov.cn/WS04/CL2578/376293.html. Accessed April5, 2020.
- 27.Chinese National Health Commission. Diagnosis and treatment plan for pneumonia with COVID-19. Available from: http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_2275/index_1.html. Accessed February20, 2020.
- 28.China Center for Disease Control and Prevention. Public prevention guidelines for COVID-19 pneumonia. Available from: http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/W020200128207842237479.pdf. Accessed February20, 2020.
- 29.China Center for Disease Control and Prevention. Plan for prevention and control of pneumonia caused by new coronavirus. Available from: http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/t20200123_211379.html. Accessed February20, 2020.
- 30.Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11235&gecstype=1. Accessed February18, 2020.
- 31.Wuhan Municipal Bureau of statistics. 2018 Wuhan statistical yearbook. Available from: http://tjj.wuhan.gov.cn/tjfw/tjnj/202004/t20200426_1124257.shtml. Accessed February10, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Chinese Center for Disease Control and Prevention. Epidemic update and risk assessment of 2019 Novel Coronavirus. Available from: http://www.chinacdc.cn/yyrdgz/202001/P020200128523354919292.pdf. Accessed February10, 2020.
- World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Available from: https://www.who.int/news-room/detail/30-01-2020-statement-on-the-second-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-outbreak-of-novel-coronavirus-(2019-ncov). Accessed February1, 2020.
- Chinese National Health Commission. Epidemic notification. Available from: http://www.nhc.gov.cn/xcs/yqtb/list_gzbd.shtml. Accessed May5, 2020.
- Yang, M.Zhao J, Zhang, Z. More than pneumonia, the potential occurrence of multiple organ failure in 2019 novel coronavirus infection. SSRN Electronic Journal, January 2020. doi: 10.2139/ssrn.3532272 Available from: https://ssrn.com/abstract=3532272. Accessed February5, 2020. [DOI]
- Wuhan Municipal Health Commission. Report of viral pneumonia of unknown cause. Available from: http://www.nhc.gov.cn/xcs/yqtb/202001/1beb46f061704372b7ca41ef3e682229.shtml. Accessed February1, 2020.
- Hubei Province Health Commission. Novel coronavirus infection pneumonia knowledge of health science. Available from: http://wjw.hubei.gov.cn/bmdt/ztzl/fkxxgzbdgrfyyq/jkkp/202001/t20200121_2013874.shtml. Accessed February1, 2020.
- Chinese National Health Commission. Announcement. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202001/44a3b8245e8049d2837a4f27529cd386.shtml. Accessed February1, 2020.
- Information Office of the Chinese State Council. First level response to public health emergencies in 31 provinces of mainland China. Available from: http://china.caixin.com/2020-01-29/101509411.html. Accessed February1, 2020.
- Wuhan Municipal Government. Announcement of novel coronavirus infection prevention command headquarters in Wuhan. Available from: http://jyh.wuhan.gov.cn/pub/whs_70/zwgk/tzgg/202003/t20200316_972434.shtml. Accessed February1, 2020.
- Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11209&gecstype=1. Accessed February1, 2020.
- Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11234&gecstype=1. Accessed February18, 2020.
- Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11211&gecstype=1. Accessed February1, 2020.
- Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11295&gecstype=1. Accessed April13, 2020.
- Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11266&gecstype=1. Accessed March20, 2020.
- Cai G. Bulk and single-cell transcriptomics identify tobacco-use disparity in lung gene expression of ACE2, the receptor of 2019-nCov. medRxiv. 2020. doi: 10.20944/preprints202002.0051.v3 Available from: https://www.medrxiv.org/content/medrxiv/early/2020/02/17/2020.02.05.20020107.full.pdf. Accessed February10, 2020. [DOI]
- Zhao Y, Zhao Z, Wang Y, et al. Single-cell RNA expression profiling of ACE2, the putative receptor of Wuhan 2019-nCov. BioRxiv. 2020. doi: 10.1101/2020.02.11.20022228 Available from: https://www.biorxiv.org/content/10.1101/2020.01.26.919985v2.full.pdf. Accessed February10, 2020. [DOI]
- Chinese National Medical Products Administration. Press conference record. Available from: http://www.nmpa.gov.cn/WS04/CL2578/376293.html. Accessed April5, 2020.
- Chinese National Health Commission. Diagnosis and treatment plan for pneumonia with COVID-19. Available from: http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_2275/index_1.html. Accessed February20, 2020.
- China Center for Disease Control and Prevention. Public prevention guidelines for COVID-19 pneumonia. Available from: http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/W020200128207842237479.pdf. Accessed February20, 2020.
- China Center for Disease Control and Prevention. Plan for prevention and control of pneumonia caused by new coronavirus. Available from: http://www.chinacdc.cn/jkzt/crb/zl/szkb_11803/jszl_11815/202001/t20200123_211379.html. Accessed February20, 2020.
- Chinese National Health Commission. Press conference record. Available from: http://www.nhc.gov.cn/xwzb/webcontroller.do?titleSeq=11235&gecstype=1. Accessed February18, 2020.
- Wuhan Municipal Bureau of statistics. 2018 Wuhan statistical yearbook. Available from: http://tjj.wuhan.gov.cn/tjfw/tjnj/202004/t20200426_1124257.shtml. Accessed February10, 2020.