Dear Editor,
We read with great interest the recent study of Volpicelli et al. [1], in which the authors propose objective ultrasonographic criteria to evaluate pulmonary alterations in COVID-19. Indeed, ultrasound (US) has been successfully used in the ICU setting and, in a pandemic situation, can represent a valuable option for reducing pressure on computed tomography systems in times of imbalance between demand and the existing imaging structure [2].
In our pathology service, US is routinely used to guide minimally invasive autopsies (MIA/US) of COVID-19 deceased patients [3, 4]. MIA/US was chosen because it is an inexpensive procedure for obtaining tissue samples from several organs and, at the same time, reduces the risks of the autopsy procedure in a highly contagious situation. The first case was studied on March 18, 2020; to date, we have evaluated 30 cases and the series increases daily, encompassing different stages of the disease.
During MIA-US, we observed aspects similar to those described by Volpicelli et al. [1], which oriented the extensive pulmonary tissue sampling in these patients (48 samples in each case, obtained with a 14 G Tru-cut, from four predefined pulmonary areas in each lung).
Three distinct histological patterns were identified in severe COVID-19 affected lungs: A. Acute pulmonary injury: defined as exudative inflammatory changes that include exudative diffuse alveolar damage (DAD), alveolar edema, neutrophilic pneumonia and hemorrhage; B. early fibroproliferative changes: defined as a mixed pattern of acute and fibroproliferative changes, with organization of the exudative process and deposition of loose extracellular matrix; C. predominant pattern of fibroproliferation (fibroproliferative DAD).
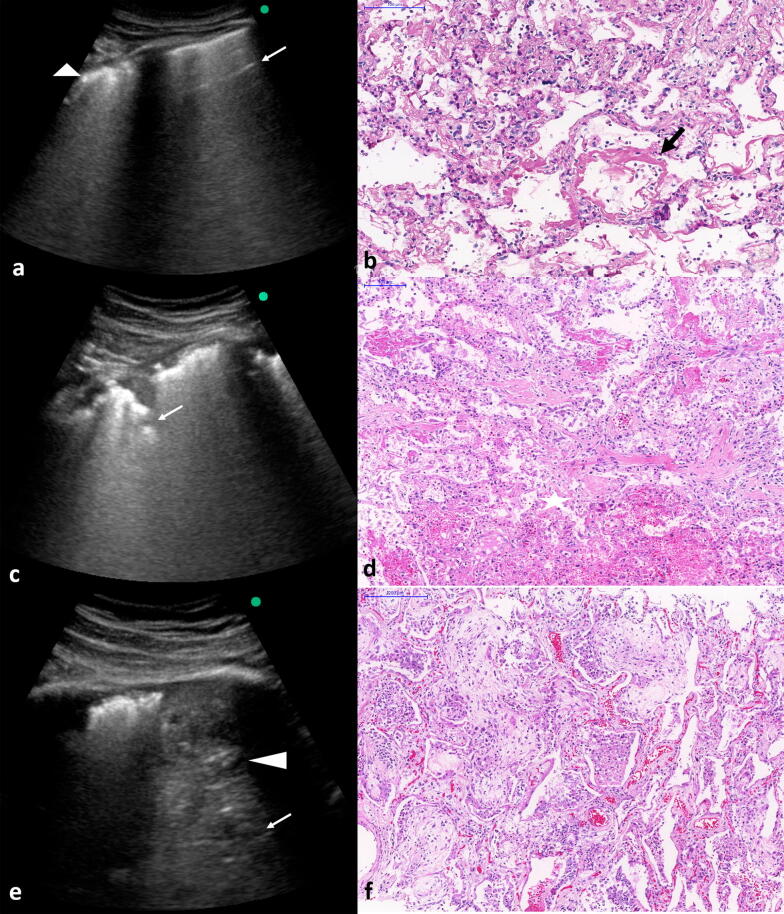
We tested the agreement between US image patterns and histological alterations in 10 COVID-19 fatal cases by blindly comparing the diagnosis made by ultrasound and those obtained by histopathological analysis. A full agreement was obtained, fulfilling some criteria of category D of probability (“High probability”) of COVID-19 based on patterns of lung ultrasound findings proposed by Volpicelli et al. [1] (Figure 1).
Fig. 1.
Correlation between lung ultrasound (LUS) postmortem images with histology findings in fatal cases of COVID-19. a, b COVID-19 pneumonia in the early phase with irregular and thickened pleural line (arrowhead) and spared areas with A line (arrow) at LUS examination. The histology shows acute pulmonary injury with hyaline membranes (arrow). c, d intermediary phase with pleural thickening and subpleural consolidations at LUS examination. The histology shows early fibroproliferative changes (in the center) associated with acute diffuse alveolar damage (DAD). e, f LUS examination shows thickened pleural line and consolidation (arrowhead) with air bronchograms (arrow) in the base of left lung. The histology shows fibroproliferative DAD
This analysis produced a series of paired histology-ultrasound images that can complement the information presented by Volpicelli et al. [1], contributing to reinforce the usefulness of US imaging in screening for suspected cases and to monitor the severity of affected patients. Here, we prepared a panel of combined US/histopathological images from the same pulmonary areas, using as reference the parameters proposed by Volpicelli et al. [1] Our results support the idea that US imaging can characterize the progressive changes in the pulmonary structure caused by SARS-CoV-2.
Acknowledgements
The authors wish to thank to all involved in the care for the patients with COVID-19 and to all hospital workers who take part in the HC-FMUSP-Coronavirus Crisis Committee during the epidemic season. To all relatives and legal representatives who agreed with the postmortem examination of COVID-19 victims.
Collaborator members of BIAS - Brazilian Image Autopsy Study Group: Luiz Fernando Ferraz da Silva, Thais Mauad, Glaucia Aparecida Bento dos Santos, Thábata Larissa Luciano Ferreira Leite, Catia Sales de Moura, Jair Theodoro Filho, Kely Cristina Soares Bispo, Angela B. G. dos Santos, Sandra de Moraes Fernezlian and Reginaldo Silva do Nascimento.
Funding
Fundação de Amparo à Pesquisa do Estado de São Paulo 2013/17159-2. Funder 10.13039/501100001807; Bill and Melinda Gates Foundation INV-002396. Funder 10.13039/100000865.
Compliance with ethical standards
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
This study has been approved by the HC-FMUSP Ethical Committee (Protocol #3951.904).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Amaro Nunes Duarte-Neto, Email: amaro.ndneto@hc.fm.usp.br.
BIAS - Brazilian Image Autopsy Study Group:
Luiz Fernando Ferraz da Silva, Thais Mauad, Glaucia Aparecida Bento dos Santos, Thábata Larissa Luciano Ferreira Leite, Catia Sales de Moura, Jair Theodoro Filho, Kely Cristina Soares Bispo, Angela B. G. dos Santos, Sandra de Moraes Fernezlian, and Reginaldo Silva do Nascimento
References
- 1.Volpicelli G, Lamorte A, Villén T. What’s new in lung ultrasound during the COVID-19 pandemic. Intensive Care Med. 2020 doi: 10.1007/s00134-020-06048-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Enghard P, Rademacher S, Nee J, et al. Simplified lung ultrasound protocol shows excellent prediction of extravascular lung water in ventilated intensive care patients. Crit Care. 2015;19:36. doi: 10.1186/s13054-015-0756-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dolhnikoff M, Duarte-Neto AN, de Almeida Monteiro RA, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020 doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duarte-Neto AN, Monteiro RAA, Johnsson J, et al. Ultrasound-guided minimally invasive autopsy as a tool for rapid post-mortem diagnosis in the 2018 Sao Paulo yellow fever epidemic: correlation with conventional autopsy. PLoS Negl Trop Dis. 2019;13(7):e0007625. doi: 10.1371/journal.pntd.0007625. [DOI] [PMC free article] [PubMed] [Google Scholar]