Abstract
Objective
The mainstream media tend to rely on news content that will increase risk perceptions of pandemic outbreaks to stimulate public response and persuade people to comply with preventive behaviours. The objective of this study was to examine associations between exposure to coronavirus disease (COVID‐19) news, risk perceptions, and depressive symptoms.
Methods
Cross‐sectional data were collected from 501 participants who were ≥18 years. Exposure to COVID‐19 news was assessed as our exposure variable. We screened for depression (outcome variable) with the Patient Health Questionnaire and examined the roles of risk perceptions. Multiple linear regressions and mediation analysis with 1000 bootstrap resamples were conducted.
Results
Participants were 55.29% female, 67.86% White with mean age 32.44 ± 11.94 years. After controlling for sociodemographic and socio‐economic factors, news exposure was positively associated with depressive symptoms β = .11; 95% confidence interval (95%CI) = 0.02–0.20. Mediation analysis showed that perceived vulnerability to COVID‐19 mediated 34.4% of this relationship (β = .04; 95%CI = 0.01–0.06).
Conclusion
Perceived vulnerability to COVID‐19 can serve as a pathway through which exposure to COVID‐19 news on mainstream media may be associated with depressive symptoms. Based on our findings, we offered recommendations for media–health partnership, practice, and research.
Keywords: COVID‐19, depression, mainstream media, risk perception
Statement of contribution.
What is already known on this subject?
Mainstream media use the elements of elevated risk perception to steer public response during pandemic outbreaks.
Frequent exposure to risk‐framed news is positively associated with risk perception.
Risk perception is positively associated with psychosocial distress.
What does this study add?
Frequent exposure to coronavirus disease (COVID‐19) news on mainstream media is positively associated with depressive symptoms.
Perceived vulnerability to COVID‐19 mediates the relationship between exposure to COVID‐19 news and depressive symptoms.
Perceived self‐efficacy to practice protective behaviour is positively associated with news exposure and negatively associated with depressive symptoms.
Since the onset of the first reported coronavirus disease (COVID‐19) patient on 1 December 2019 (Huang et al., 2020), the disease has rapidly spread worldwide to over 100 countries with more than 937,000 cases, 47,256 deaths (World Health Organization, 2020). As of 3 April 2020, the United States has recorded 239,279 cases and 5,443 deaths, making it the leading nation in the world for the number of cases (CDC, 2020). These alarming estimations have triggered emergency preparedness efforts and public awareness through the swift dissemination of risk‐framed information in the mainstream media (Cowper, 2020; Dyer, 2020; Laupacis, 2020; Oxford Analytica, 2020). Understandably, it is important to glean up‐to‐date information regularly to stay in compliance with local and state authorities, as well as to mind the well‐being of family and loved ones in different parts of the world. The purpose of this current study was to assess the psychosocial outcomes of exposure to COVID‐19 news on the mainstream media.
American mainstream media is known to shape public perceptions through its widely available news conglomerates (e.g., digital, electronic, and print media) (Atton, 2002; Nair, Janenova, & Serikbayeva, 2020), giving it a significant influence on the psychological outcomes of rapidly shared information during pandemics (Leo & Lacasse, 2008; Meadows & Foxwell, 2011). However, managing the COVID‐19 pandemic requires a balanced and prompt approach which informs the public on what they can do, without causing a mental health burden (Cowper, 2020; Keles, McCrae, & Grealish, 2020; Seabrook, Kern, & Rickard, 2016). In an attempt to stimulate public response, threat perception, and persuade people to comply with the preventive policies and regulations, the mainstream media rely on producing news contents that will increase the perceived self‐efficacy to protect, vulnerability to the disease, and severity of the pandemic outbreaks (Bish & Michie, 2010; Park, Boatwright, & Avery, 2019; Pieri, 2019). For instance, in a recent video coverage, CNN interviewed recovering COVID‐19 patients who described their perceived vulnerability, severity, and experiences with the disease (CNN, 2020). However, frequent exposure to risk‐framed news may negatively impact the viewers' mental health (Keles et al., 2020; Seabrook et al., 2016). Therefore, it is important to investigate the mental health consequence of exposure to pandemic news on mainstream media. The objective of this study was to examine the association between exposure to COVID‐19‐related news on mainstream media, risk perceptions, and depressive symptoms.
Methods
To satisfy this objective, we deployed a survey tool with validated screening techniques for rapid assessment of the mental health implications of the ongoing pandemic. The study was approved by the Institution Review Board of the University of Illinois at Chicago. All participants signed the online informed consent form before proceeding with the survey.
Study sample
Participants were recruited via Prolific, an online crowdsourcing platform for researchers (Peer, Brandimarte, Samat, & Acquisti, 2017). Recent studies have established the diversity of the participant pool and the high quality of the data collected from Prolific. For example, compared to other crowdsourcing platforms, participants from Prolific scored higher on attention‐checks, engaged in lesser dishonest behaviour, and were able to reproduce existing results (Palan & Schitter, 2018; Peer et al., 2017). Eligibility criteria for participants were (1) residence in the United States and (2) being 18 years or older. Cross‐sectional data were collected from 502 participants on 25 March 2020, through the Qualtrics online survey.
Media exposure
Exposure to COVID‐19 news on mainstream media was measured by asking participants four questions starting with the stem statement How frequently do you get information on coronavirus from any of the following sources? (1) Cable news channels (e.g., Fox News, CNN), (2) Local news channels, (3) New York Times, and (4) Washington post. Response options ranged from 1 = Never to 5 = Daily. Responses were summed and divided by 4 to provide a composite score ranging from 1 to 5 for each participant.
The most recent information source for COVID‐19 was assessed by adapting one question from the National Cancer Institute Health Information National Trends Survey (HINTS) (Nelson et al., 2004). Participants were asked The most recent time you looked for information about COVID‐19, where did you go first? Response options included television, friends, and government websites.
Depression screening
Patient Health Questionnaire (PHQ‐2) (Gelaye et al., 2016), an established screening tool (intraclass correlation of .92), was used to screen for depressive symptoms. The PHQ probed well‐being over the past 2 weeks (recommended time of self‐quarantine): Over the past 2 weeks, how often have you been bothered by any of the following problems? (1) Little interest or pleasure in doing things and (2) Feeling down, depressed, or hopeless. Response options were (1) nearly every day, (2) more than half the day, (3) several days, and (4) not at all. Responses were reversely coded and averaged to range from 1 to 4 with low numbers indicating low depressive symptoms.
Risk perceptions
Perceived vulnerability to COVID‐19 was assessed by adapting Gainforth's perceived vulnerability scale (α = .95) (Gainforth, Cao, & Latimer‐Cheung, 2012). Three items with 5‐point response options (1 = Strongly disagree and 5 = Strongly agree) were used to assess the participants’ anxiety, fear, and worry about being infected with COVID‐19. Items started with the statement Thinking about the possibility of being infected with coronavirus makes me feel: (a) Anxious, (b) Fearful, and (c) Worried.
Perceived severity of COVID‐19 was measured using a single item that asked respondents Coronavirus is a serious infection for me to contract. Response options ranged from 1 = Strongly disagree to 5 = Strongly agree.
Perceived self‐efficacy to practice protective behaviour was assessed using a 4‐item measure (Ajzen, 2002) (alpha = .83) about participant's perceived confidence and perceived control in protecting themselves against COVID‐19 infection. An example of an item was It is possible for me to protect myself against coronavirus infection. Response options ranged from 1 = Strongly disagree to 5 = Strongly agree.
Covariates
As COVID‐19 perceptions of risk and media consumption are likely to be influenced by key demographics (e.g., age, underlying conditions), we collected key demographic variables for statistical control (Liu, Huang, & Brown, 1998; Primack, Swanier, Georgiopoulos, Land, & Fine, 2009). More specifically, participants reported on the following important demographic characteristics: sociodemographic characteristics, for example, age (continuous variable), sex (female, male) race (White, African American, Asian, Hispanic, American Indian, Middle East and North Africa [MENA] and others), and marital status. For marital status, categories included married, divorced, separated, widowed, or single. Socio‐economic status (SES) characteristics included household income (<$20,000, $20,000–<$35,000, $35,000–<$50,000, $50,000–<$75,000, and $75,000 or more), employment status, and education (less than high school, high school graduate, some college, college graduate, or more). Race was self‐reported by participants based on the provided categories. It was considered to be an important confounder because both media exposure (Johnson, Adams, Hall, & Ashburn, 1997) and depressive symptoms (Morris et al., 2011) vary by race/ethnicity.
Data analysis
Participants’ characteristics were analyzed using descriptive statistics such as frequencies, proportions, means, and standard deviations. The one‐way analysis of variance (ANOVA) was performed to investigate the mean differences in depressive symptoms by participants’ characteristics. Pearson correlations were calculated to test bivariate associations between continuous variables. To further investigate the relationship between exposure to COVID‐19 news on mainstream media and depressive symptoms, multivariable analysis was calculated to test the relationship between the exposure and depressive symptoms. Model 1 tested the unadjusted relationships. In Model 2, we adjusted for sociodemographic factors, and in Model 3, we included the SES variables. Finally, mediation analysis was conducted to test the possible mediating role of perceptions in the relationship between news exposure and depressive symptoms. Alternative pathways were also tested to address the concern of causal ordering (i.e., the mediating role of news exposure in the relationship between perceptions and depressive symptoms). Regression models were fitted in four steps according to the procedures outlined by Sobel (1982) to assess whether the association between the independent variable and depressive symptoms was mediated by risk perceptions. Statistical tests were two‐sided, and a p< .05 was considered statistically significant. Effect sizes and their confidence intervals (bootstrapping methods were used to estimate 95% confidence intervals for the indirect effects) were reported to interpret findings (Cumming, 2014). Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
After the exclusion of one participant who failed the attention check (Table 1), the remaining participants (N = 501) reported a mean age of 32.44 ± 11.94 years, being females (55.29%), White (67.86%), single/never married (68.46%), college graduate or more (53.71%), and employed (54.89%).
Table 1.
Mean (SD) of occurrences of depressive symptoms by participants’ characteristics (N = 501) a
| Variables | Depressive symptoms | ||
|---|---|---|---|
| No. (%) of participants | Means (SD) | p‐Value | |
| Sex | |||
| Female | 277 (55.29) | 1.96 (0.92) | .29 |
| Male | 224 (44.71) | 1.87 (0.94) | |
| Race b | |||
| White | 340 (67.86) | 1.93 (0.94) | .98 |
| African American | 30 (5.99) | 1.92 (1.05) | |
| Asian | 72 (14.37) | 1.85 (0.86) | |
| Hispanic | 41 (8.18) | 1.94 (0.87) | |
| American Indian/MENA/others | 18 (3.59) | 1.94 (0.97) | |
| Marital status b | |||
| Single/Never married | 343 (68.46) | 2.05 (0.93) | <.001 |
| Married | 128 (25.55) | 1.61 (0.83) | |
| Widowed/Divorced/Separated | 30 (5.99) | 1.98 (1.03) | |
| Highest education b | |||
| Less than high school/high school | 70 (14.03) | 2.20 (1.06) | <.001 |
| Some college | 161 (32.26) | 2.05 (0.97) | |
| College or more | 268 (53.71) | 1.77 (0.83) | |
| Household income b | |||
| <$15,000 | 50 (10.02) | 2.10 (0.81) | .005 |
| $15,000–$34,999 | 80 (16.03) | 2.2 (0.97) | |
| $35,000–$49,999 | 82 (16.43) | 1.99 (0.99) | |
| $50,000–$74,999 | 109 (21.84) | 1.80 (0.90) | |
| Over $75,000 | 178 (35.67) | 1.79 (0.90) | |
| Employment status | |||
| Employed | 275 (54.89) | 1.80 (0.87) | .01 |
| Student | 102 (20.36) | 2.10 (0.95) | |
| Unemployed/retired/disabled/others | 110 (22.59) | 1.98 (0.98) | |
| Most recent information source b | |||
| Government website | 131 (29.05) | 1.90 (0.91) | .59 |
| Medical websites | 105 (23.28) | 1.88 (0.87) | |
| Social media | 78 (17.29) | 2.08 (0.95) | |
| Scientific publication | 53 (11.75) | 2.02 (1.03) | |
| Television | 50 (11.09) | 1.82 (1.01) | |
| Relatives/employer/doctor's office/print | 34 (7.54) | 1.90 (0.85) | |
| Perceived risk of unemployment | |||
| Yes | 190 (38) | 2.20 (0.80) | <.001 |
| No | 310 (62) | 1.91 (0.87) | |
MENA = Middle East and North Africa.
n may vary due to missing responses.
Results from this group should be interpreted with caution due to the small n.
Participants reported exposure to COVID‐19 news on mainstream media as 2.73 ± 0.91, depressive symptoms (1.92 ± 0.93), perceived severity (3.73 ± 1.19), perceived vulnerability (3.67 ± 1.07) and, self‐efficacy (4.01 ± 0.67). Mean occurrences of depressive symptoms by participants’ characteristics (Table 1) showed that participants who were single/never married (2.05 ± 0.93), with less than high school/high school diploma (2.20 ± 1.06), household income $15,000–$34,999 (2.2 ± 0.97), students (2.10 ± 0.95), and perceived risk of losing their jobs (2.20 ± 0.80) reported higher depressive symptoms. Pearson's correlation analysis showed that the occurrence of depressive symptoms was negatively associated with age (r = −.22, p < .001), self‐efficacy to protect self (r = −.13, p < .01), and positively associated with perceived vulnerability (r = .23, p < .001).
Model 1 showed a non‐significant positive association between exposure to COVID‐19 news and depressive symptoms (β = .06; 95% confidence interval [CI] = −0.03 to 0.14). This relationship remained non‐significant in Model 2 (β = .07; 95%CI = −0.01 to 0.16). However, after including SES in Model 3, there was a significantly positive association between the news exposure and the depressive symptoms (β = .11; 95%CI = 0.02–0.20). We also found a significantly positive relationships between news exposure and perceived severity (β = .08; 95%CI = 0.01–0.15); perceived vulnerability (β = .21; 95%CI = 0.13–0.28); and a negatively significant relationship with perceived self‐efficacy to practice protective behaviour (β = −.16; 95%CI = −0.27 to −0.04). Standardized mediation tests showed perceived vulnerability as mediating 34.4% (bias‐corrected 95%CI = 7.79–149.35) of the relationship between exposure to COVID‐19 news on mainstream media and depressive symptoms (Figure 1) with an indirect effect of β = .04; 95%CI = 0.01–0.06. We recorded non‐significant indirect effects through perceived severity (β = .00; 95%CI = −0.01 to 0.02) and perceived self‐efficacy (β = .01; 95%CI = −0.03 to 0.00). In the analysis of the alternative pathway where news exposure mediated the relationship between perceived vulnerability and depressive symptoms, we found a non‐significant indirect effect (β = .01; 95%CI = −0.00 to 0.02), a partial mediation of 2.18% (bias‐corrected 95%CI = −0.63 to 7.65) of the total effect.
Figure 1.
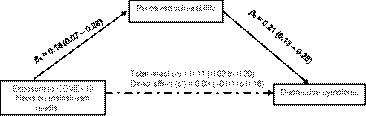
Mediation analysis: Perceived vulnerability mediates 34.4% of the total effect of exposure to COVID‐19 news on mainstream media on depressive symptoms with 1,000 bootstrap resamples β = .04, SE = .01. Bias‐corrected 95%CI = 0.01–0.06.
Discussion
In this analysis, the relationship between exposure to COVID‐19 news on mainstream media and depressive symptoms was partially mediated by perceived vulnerability to COVID‐19. Our findings suggest that perceived vulnerability to COVID‐19 can serve as a pathway through which exposure to COVID‐19 news on mainstream media may be associated with depressive symptoms. The non‐significance of the alternative pathway model further addresses concerns of causal ordering, which supports our premise. The spread of COVID‐19 news on mainstream media has been dominated by the proliferation of negatively framed information (Cowper, 2020; Dyer, 2020) such as uncertainties concerning the virus–host interaction, the evolution of the pandemic (Wang, Wang, Chen, & Qin, 2020), increased magnitude of the disease (e.g., the number of cases and fatalities both nationally and globally) (CDC, 2020), momentous government policies (Lazzerini & Putoto, 2020), and increasing health care demand (Ferguson, Laydon, & Nedjati‐Gilani, 2020) which has psychological implications.
We, therefore, offer the following recommendations: First, in addition to disseminating information on vulnerability to COVID‐19, public health workers should work with mainstream media to provide teletherapy and mental health resource contents to their viewers. Second, considering the mediating role of perceived vulnerability, and its negative correlation with perceived self‐efficacy to practice preventive measures, mainstream media should consider offering balanced information that will increase the viewer's confidence to practice protective measures in addition to the information on vulnerability. Third, primary care providers should screen for depressive symptoms while following up with their patients either in person or via telemedicine.
Limitations
Our study is not without its limitations: first, our sample consists largely of young, educated adults and is therefore not representative; hence, our results may not be generalizable across the United States and should be interpreted with caution. Second, the use of a cross‐sectional study design makes it challenging to establish causality and warrants a careful interpretation of our result. Third, our measure of exposure to mainstream media was developed by the researchers and not validated. Nevertheless, the correlation with other items is consistent with previous studies on media exposure (Keles et al., 2020; Seabrook et al., 2016). Future studies should therefore consider testing these relationships longitudinally and with more valid measures to improve our understanding of these associations.
Conclusion
In this study of 501 participants, perceived vulnerability mediated the relationship between exposure to COVID‐19 news on the mainstream media and depressive symptoms. In addition to providing information about the vulnerability to COVID‐19, mainstream media outlets should offer contents that will reduce their viewers’ mental health burden at this critical time.
Conflicts of interest
All authors declare no conflict of interest.
Author contributions
Ayokunle Olagoke (Conceptualization; Data curation; Formal analysis; Methodology; Writing – original draft) Olakanmi Ojo Olagoke (Writing – original draft; Writing – review & editing) Ashley Hughes (Methodology; Supervision; Writing – review & editing).
Acknowledgement
We are grateful to Professor David DuBois for his helpful advice.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
References
- Ajzen, I. (2002). Constructing a TPB questionnaire: Conceptual and methodological considerations. Retrieved from http://www.people.umass.edu/aizen/pdf/tpb.measurement.pdf [Google Scholar]
- Atton, C. (2002). News cultures and new social movements: Radical journalism and the mainstream media. Journalism Studies, 3, 491–505. 10.1080/1461670022000019209 [DOI] [Google Scholar]
- Bish, A. , & Michie, S. (2010). Demographic and attitudinal determinants of protective behaviours during a pandemic: A review. British Journal of Health Psychology, 15, 797–824. 10.1348/135910710X485826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . (2020). Coronavirus Disease 2019 (COVID‐19) in the U.S. Centers for Disease Control and Prevention. Retrieved from https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html [Google Scholar]
- CNN . (2020). Recovering patients describe what it's like to contract coronavirus – CNN video. Retrieved from https://www.cnn.com/videos/world/2020/02/13/china-coronavirus-survivors-culver-pkg-ctw-intl-hnk-vpx.cnn [Google Scholar]
- Cowper, A. (2020). Covid‐19: Are we getting the communications right? BMJ, 368, m919. 10.1136/bmj.m919 [DOI] [PubMed] [Google Scholar]
- Cumming, G. (2014). The new statistics. Psychological Science, 25(1), 7–29. 10.1177/0956797613504966 [DOI] [PubMed] [Google Scholar]
- Dyer, O. (2020). Trump claims public health warnings on covid‐19 are a conspiracy against him. BMJ, 368, m941. 10.1136/bmj.m941 [DOI] [PubMed] [Google Scholar]
- Ferguson, N. M. , Laydon, D. , Nedjati‐Gilani, G. , Imai, N. , Ainslie, K. , Baguelin, M. , … Ghani, A. C. (2020). Impact of non‐pharmaceutical interventions (NPIs) to reduce COVID‐19 mortality and healthcare demand. London, UK: Imperial College. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gainforth, H. L. , Cao, W. , & Latimer‐Cheung, A. E. (2012). Determinants of human papillomavirus (HPV) vaccination intent among three Canadian target groups. Journal of Cancer Education, 27, 717–724. 10.1007/s13187-012-0389-1 [DOI] [PubMed] [Google Scholar]
- Gelaye, B. , Wilson, I. , Berhane, H. Y. , Deyessa, N. , Bahretibeb, Y. , Wondimagegn, D. , … Williams, M. A. (2016). Diagnostic validity of the Patient Health Questionnaire‐2 (PHQ‐2) among Ethiopian adults. Comprehensive Psychiatry, 70, 216–221. 10.1016/j.comppsych.2016.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, C. , Wang, Y. , Li, X. , Ren, L. , Zhao, J. , Hu, Y. , … Cao, B. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet, 395, 497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, J. D. , Adams, M. S. , Hall, W. , & Ashburn, L. (1997). Race, media, and violence: Differential racial effects of exposure to violent news stories. Basic and Applied Social Psychology, 19(1), 81–90. 10.1207/s15324834basp1901_6 [DOI] [Google Scholar]
- Keles, B. , McCrae, N. , & Grealish, A. (2020). A systematic review: The influence of social media on depression, anxiety and psychological distress in adolescents. International Journal of Adolescence and Youth, 25(1), 79–93. 10.1080/02673843.2019.1590851 [DOI] [Google Scholar]
- Laupacis, A. (2020). Working together to contain and manage COVID‐19. Canadian Medical Association Journal, 192(13), E340–E341. 10.1503/cmaj.200428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazzerini, M. , & Putoto, G. (2020). COVID‐19 in Italy: Momentous decisions and many uncertainties. The Lancet Global Health, 8, e641–e642. 10.1016/S2214-109X(20)30110-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leo, J. , & Lacasse, J. R. (2008). The media and the chemical imbalance theory of depression. Society, 45(1), 35–45. 10.1007/s12115-007-9047-3 [DOI] [Google Scholar]
- Liu, S. , Huang, J.‐C. , & Brown, G. L. (1998). Information and risk perception: A dynamic adjustment process. Risk Analysis, 18, 689–699. 10.1111/j.1539-6924.1998.tb01113.x [DOI] [PubMed] [Google Scholar]
- Meadows, M. , & Foxwell, K. (2011). Community broadcasting and mental health: The role of local radio and television in enhancing emotional and social well‐being. Radio Journal: International Studies in Broadcast & Audio Media, 9(2), 89–106. 10.1386/rjao.9.2.89_1 [DOI] [Google Scholar]
- Morris, A. , Zhao, L. , Ahmed, Y. , Stoyanova, N. , De Staercke, C. , Hooper, W. C. , … Vaccarino, V. (2011). Association between depression and inflammation–differences by race and sex: The META‐Health study. Psychosomatic Medicine, 73, 462–468. 10.1097/PSY.0b013e318222379c [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nair, B. , Janenova, S. , & Serikbayeva, B. (2020). Social and mainstream media relations. In A primer on policy communication in Kazakhstan (pp. 35–48). Singapore: Palgrave Pivot. [Google Scholar]
- Nelson, D. , Kreps, G. , Hesse, B. , Croyle, R. , Willis, G. , Arora, N. , … Alden, S. (2004). The Health Information National Trends Survey (HINTS): Development, design, and dissemination. Journal of Health Communication, 9, 443–460. 10.1080/10810730490504233 [DOI] [PubMed] [Google Scholar]
- Oxford Analytica . (2020). Misinformation will undermine coronavirus responses. Melbourne, Australia: Emerald Expert Briefings; (oxan‐db). [Google Scholar]
- Palan, S. , & Schitter, C. (2018). Prolific.ac—A subject pool for online experiments. Journal of Behavioral and Experimental Finance, 17, 22–27. 10.1016/j.jbef.2017.12.004 [DOI] [Google Scholar]
- Park, S. , Boatwright, B. , & Avery, E. J. (2019). Information channel preference in health crisis: Exploring the roles of perceived risk, preparedness, knowledge, and intent to follow directives. Public Relations Review, 45, 101794. 10.1016/j.pubrev.2019.05.015 [DOI] [Google Scholar]
- Peer, E. , Brandimarte, L. , Samat, S. , & Acquisti, A. (2017). Beyond the Turk: Alternative platforms for crowdsourcing behavioral research. Journal of Experimental Social Psychology, 70, 153–163. 10.1016/j.jesp.2017.01.006 [DOI] [Google Scholar]
- Pieri, E. (2019). Media framing and the threat of global pandemics: The Ebola crisis in UK Media and policy response. Sociological Research Online, 24(1), 73–92. 10.1177/1360780418811966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack, B. A. , Swanier, B. , Georgiopoulos, A. M. , Land, S. R. , & Fine, M. J. (2009). Association between media use in adolescence and depression in young adulthood: A longitudinal study. Archives of General Psychiatry, 66, 181–188. 10.1001/archgenpsychiatry.2008.532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seabrook, E. M. , Kern, M. L. , & Rickard, N. S. (2016). Social networking sites, depression, and anxiety: A systematic review. JMIR Mental Health, 3(4), e50. 10.2196/mental.5842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobel, M. E. (1982). Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology, 13, 290–312. 10.2307/270723 [DOI] [Google Scholar]
- Wang, Y. , Wang, Y. , Chen, Y. , & Qin, Q. (2020). Unique epidemiological and clinical features of the emerging 2019 novel coronavirus pneumonia (COVID‐19) implicate special control measures. Journal of Medical Virology, 92(6), 568–576. 10.1002/jmv.25748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2020). Novel Coronavirus Disease 2019 (COVID‐19) Situation Report – 68. Retrieved from https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200328-sitrep-68-covid-19.pdf?sfvrsn=384bc74c_2 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


