Abstract
Because of the coronavirus disease 2019 (COVID‐19) emergency, on March 9, 2020 Italy went in lock‐down imposing the closure of non‐urgent outpatient clinics devoted to care of chronic, severe, inflammatory skin diseases that require periodic follow‐up. In this emergency situation, due to the lack of a teledermatology platform and in order not to leave our vulnerable high‐need patients without proper follow‐up, we started a teledermatologic service in smartworking using phone calls and emails. The total number of patients scheduled was 195; in 12 cases, we were not able to talk to the patients. Remote monitoring was performed in 183 patients (126 moderate to severe psoriasis, 10 severe acne, 11 severe atopic dermatitis, 11 hidradenitis suppurativa, 9 blistering autoimmune diseases, and 16 other autoimmune skin diseases). During remote‐visits, several interventions were conducted: triage for COVID‐19 suspected symptoms, email check of clinical pictures and of laboratory examinations, advices for topical and systemic therapy continuation or discontinuation/switch and reschedule of next appointment. Only five patients required personal office visit (2.7%), reducing consistently the number of face‐to face visits. Our real‐life experience shows that remote monitoring was effective in preventing unnecessary worsening of severe chronic skin diseases and poor outcomes due to withdrawal of current therapy.
Keywords: atopic dermatitis, COVID‐19, psoriasis, smartworking, teledermatology, telemonitoring
1. INTRODUCTION
Autoimmune skin diseases, moderate to severe psoriasis, severe atopic dermatitis (AD), hidradenitis suppurativa (HS) and severe acne are chronic and disabling cutaneous conditions that require regular care by a high‐trained specialist in order to avoid worsening of the disease itself, to prevent systemic involvement and necessitate monitoring of systemic therapies. 1 , 2
Because of the coronavirus disease 2019 (COVID‐19) emergency, on March 9, 2020 Italy went in lock‐down imposing the closure of non‐urgent outpatient clinics devoted to care of chronic, severe, inflammatory skin diseases that require periodic follow‐up. 1 , 2 , 3 , 4 , 5 Teledermatology and remote monitoring technologies (RMTs) may improve the quality of care, reduce barriers (as lock‐down) and allow to follow‐up patients. 6
In order not to leave our vulnerable high‐need patients without proper follow‐up, we started a teledermatologic service in smartworking. We present the data of 2 months of real‐life of remote monitoring.
2. METHODS
All patients scheduled in psoriasis outpatient clinic, atopic dermatitis outpatient clinic autoimmune skin diseases outpatient clinic and acne outpatient clinic received a telephonic visits and if required store and forward teledermatology (SAF‐TD). Access to personal health records from hospital in a remote fashion (smartworking) was allowed 2 days a week for the caring physician (A.M.G.B.) and most of the phone call‐work was done in a remote fashion.
Telephone‐numbers of all scheduled appointments were available and 2 days prior to the office‐visit all patients were contacted by telephone and the following information was asked and collected in a database:
Duration and number of phone calls per patient
Diagnosis
General status and symptoms of COVID‐19 and/or COVID‐19 diagnosis and/or admission to hospital
Current treatment: systemic and topical
Actual skin status: stable, worsening, in case of doubt patients were asked to send via email clinical photographs
Laboratory examinations, if necessary were asked to be send by email
After the first call the decision if a personal office visit was necessary according to the dermatological and general status was made and if not necessary, several interventions were conducted (Figure 1):
Advice to seek for help in the emergency system for COVID‐19 in case of suspected symptoms in order to perform swabs and testing for suspect patients
Email check of clinical pictures
Email check of laboratory examinations
Advice for topical therapy continuation or discontinuation
Advice for systemic therapy continuation or discontinuation
FIGURE 1.
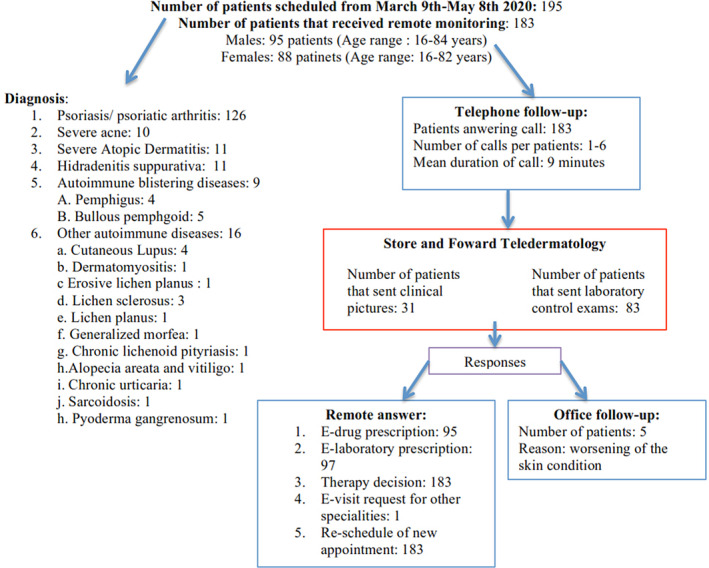
Flow‐chart of the remote monitoring process
Several registration‐actions were performed as:
Clinical chart registration of clinical status, of laboratory results and of therapy‐advice: continuation, modification, or withdrawal
E‐prescription of systemic or topical drugs
E‐laboratory prescription
Request for other specialties consultation: ie, Rheumatology, with e‐visit‐request.
Reschedule of next appointment
We analyzed the collected data from the ninth of March to the eighth of May 2020.
3. RESULTS
The total number of patients scheduled for control in that period was 195; in 12 cases we were not able to talk to the patients (never answered the phone‐calls or called‐back) and they did not show‐up for control. In 183 cases remote monitoring was performed; 126 patients had moderate to severe psoriasis, 10 had severe acne, 11 had severe AD, 11 had HS, 9 had blistering autoimmune diseases (4 pemphigus, 5 bullous pemphigoid), 16 with other autoimmune skin diseases (4 cutaneous lupus, 3 lichen sclerosus, 1 oral erosive lichen, 1 lichen planus, 1 generalized morfea, 1 pytiriasis lichenoides, 1 pyoderma gangrenosum, 1 alopecia areata and vitiligo, 1 sarcoidosis, 1 dermatomyositis and 1 chronic urticaria). Details are shown in Table 1.
TABLE 1.
Demographic data, diagnosis, and therapies of the 183 patients
| Diagnosis (No. of pts) | Psoriasis (126) | Acne (10) | AD (11) | HS (11) | Autoimmune blistering disease (9) | Other autoimmune skin disease (16) |
|---|---|---|---|---|---|---|
| Sex: M/F (% M) | 76/50 (60.3%) | 6/4 (60%) | 5/6 (40%) | 3/8 (27.3%) | 2/7 (28.6%) | 3/13 (18.7%) |
| Age: range (mean years) | 23‐84 y (60) | 16‐23 y (18.5) | 24‐72 y (49.7) | 16‐49 y (38.2) | 60‐83 y (71.1) | 26‐78 y (52.1) |
| Current systemic treatment (No. of pts) | MTX (45), CSA (1), ACI (9), DMF (3), APR (3), UVB/topical (9), ADA (25), ETA (1), UST (6), SEC (7), IXE (1), BRO (4), GUS (9), TIL (1), RIS (1), GOL (1) |
Isotretinoin (10) Prednisone (1) |
CSA (2) DUPI (4) MTX (4) Topical and UVB (1) |
ADA (7) DOXI (2) RIF/CLIN (2) |
RITU (1) PRED (9) |
HCQ (3) PRED (3) MTX (3) OMA (1) TOFA (1) ADA (1) |
| Topical therapy (No. of pts) |
Emollients (126) Betamethasone/Calcipotriol (48) |
Emollients (10) |
Emollients (11) TCS (8) Tacrolimus (5) |
Antiseptics (11) | TCS (6) |
CSA (1) TCS (7) |
| Actual skin status |
Stable: 122 pts Worsening: 4 pts |
Stable: 10 pts |
Stable: 10 pts Worsening: 1 patient |
Stable: 11 pts | Stable: 9 | Stable: 16 |
| Lab exams sent by pts | 55 | 10 | 6 | 3 | 4 | 5 |
| General status (No. of pts)/COVID‐19 (No. of pts) | Good (123)/COVID‐19 (2)/death (2) | Good (10)/COVID‐19 (0) | Good (11)/0 COVID‐19 (0) | Good (11)/0 COVID‐19 (0) | Good (8)/COVID‐19 (1) | Good (16)/COVID‐19 (0) |
| Office required visits | 4 pts | 0 | 1 pt | 0 | 0 | 0 |
Abbreviations: ACI, acitretin; AD, atopic dermatitis; ADA, adalimumab; APR, apremilast; BRO, brodalumab; CSA, ciclosporine; DMF, dimetil fumarate; DUPI, dupilumab; DOXI, doxicycline; ETA, etanercept; F, female; GOL, golimumab; GUS, guselkumab; HS, hidradenitis suppurativa; HCQ, hydroxychloroquine; IXE, ixekizumab; Lab, laboratory; M, male; MTX, methotrexate; No., number; OMA, omalizumab; pts, patients; RIS, risankizumab; RIF/CLIN, rinfamycin/clindamycin; RITU, rituximab; SEC, secukinumab; TIL, tildrakiyumab; TOFA, tofacitinib; TCS, topical corticosteroids; UST, ustekinumab; UVB, ultraviolet B.
Mean phone‐call duration was 9 minutes; the number of phone‐calls per patient made ranged from 1 to 6 (mean: 1.6); the number of e‐mails per patient range from 0 to 4, mean: 0.9. During remote monitoring, 178 patients referred a stable skin condition/remission while in five cases (2.7%; 4 affected by psoriasis and one by atopic dermatitis) was reported a worsening of the skin disease that required personal office visit. We received reports of laboratory exams from 83 patients, 97 patients received by e‐mail an e‐prescription for laboratory exams and 95 an e‐drug prescription. Seventy‐one patients were under biological therapy/small molecules. Three patients referred diagnosis of COVID‐19, one died and two recovered completely.
One‐hundred and ten patients affected by psoriasis continued therapy as before; in three cases dose reduction of methotrexate (MTX) was advised; one patient started a new therapy (Tildrakizumab) and in one case switch of drug was required (Brodalumab to Risankizumab). In 10 cases withdrawal of therapy was recorded due to: (a) death (2 cases, only one due to COVID‐19; both patients were under Guselkumab for severe psoriasis, both were older than 78 years‐old and with comorbidities); (b) lymphopenia (1 case) under MTX; (c) increase of transaminases (1 case) under MTX; (d) fear of COVID‐19 (2 cases) under MTX; (e) new diagnosis of cancer (1 case) under Adalimumab biosimilar; (f) worsening of psoriasis (2 cases) under MTX; (g) lack of drug (1 case) under acitretin (details in Tables 1 and 2).
TABLE 2.
Outcome, measures, and advices for the 183 patients
| Diagnosis (No. of pts) | Psoriasis/PsA (126) | Acne (10) | AD (11) | HS (11) | Autoimmune blistering disease (9) | Other autoimmune skin diseases (16) |
|---|---|---|---|---|---|---|
| Mean call duration of the first call | 9 minutes | 8 minutes | 10 minutes | 7 minutes | 7 minutes | 8 minutes |
| No. of calls per patient range (mean) | 1‐6 (1.5) | 1‐4 (2.3) | 1‐4 (2.7) | 1‐3 (1.2) | 1‐4 (1.2) | 1‐3 (1.2) |
| No. of e‐mails per patient range (mean) | 0‐4 (0.8) | 1‐4 (1.6) | 1‐4 (1.2) | 1–2 (1.1) | 1‐3 (1.2) | 0‐2 (0.8) |
| Systemic therapy |
Continue: 110 Dose reduction: 3 MTX Switch: 1 BRO to RIS Start therapy: 1 TIL Withdrawal: 11 pts, 6 MTX, 1 ACI, 1 ADA, 2 GUS, 1 CSA |
Continue: 10 pts, Dose‐change isotretinoin: 2 pts |
Continue: 9 Start therapy: 1 (DUPI) |
Continue: 11 | Continue: 9 | Continue: 16 |
| Advice for COVID‐19 | 2 pts confirmed (MTX, GUS), 1 death (GUS) | None | None | None | None | None |
| No. of e‐lab prescriptions | 65 | 10 | 7 | 4 | 5 | 6 |
| No. of e‐drug prescriptions | 50 | 10 | 6 | 4 | 9 | 16 |
| E‐visit‐request for other specialties | 2 (Rheumatology) | 0 | 1 | 0 | 0 | 0 |
| Reschedule of next appointment | 126 | 10 | 11 | 11 | 9 | 16 |
All the acne patients (10) continued therapy; in two patients dose increase of isotretinoin was advised. Nine patients affected by atopic dermatitis continued therapy and in one case introduction of Dupilumab was necessary. The rest of the patients with HS and autoimmune blistering disease were stable and were advised to continue therapy as before (details in Tables 1 and 2).
The modality of remote monitoring required different steps: (a) calling the patients with a mean time per call of 9 minutes; (b) an email‐check (patient sent 1‐4 emails with laboratory results and/or clinical pictures, mean: 0.9 emails); (c) email an answer with different strategies: e‐drug prescription (97), e‐lab prescription (95), e‐request for consultant (1); (d) new phone call for therapy advice; and (e) reschedule of appointments (183). We were not able to record exactly the whole time required per patient but approximately it was around 20 minutes.
4. DISCUSSION
Social distancing measures recommended to prevent the widespread of COVID‐19 and the lock‐down imposed in Italy since the ninth of March determined the reduction of dermatological consultations approximately of 80% to 90%. 1 Telemedicine and teledermatology are an opportunity to continue to deliver health care system. 1 , 3
In this emergency situation, a prompt solution was needed in order to respect the legislation, the desire of patients to remain home avoiding coming to hospital and the need not to interrupt the care of high need dermatological patients. Teledermatology systems are not yet implemented in routine Health Care System in Italy. Moreover, web conferencing software allowing video‐conferences are not diffusely known by our patients; therefore, an hybrid teledermatology system of telephone calls and e‐mail seemed to us the most widely, immediate and diffuse mode of communication in order to answer this task.
We were able to conduct the remote monitoring in 94% (183/195) of the scheduled patients, only 5 patients required personal office visit (2.7%), reducing consistently the number of face‐to face visits. Only for 6% of patients we lost contact ignoring the reason. All the 183 patients received a reschedule of appointments.
Our real‐life experience shows that remote monitoring was effective in preventing unnecessary worsening of severe chronic skin diseases and poor outcomes due to withdrawal of current therapy that might occur for different reasons as spontaneous withdrawal due to fear of COVID‐19, lack of prescription, uncontrolled side‐effects of treatments, and so forth. We were also able to switch or initiate new therapies in those patients requiring them avoiding important impairment of quality of life.
Another important aspect is that this experience was performed in smart working, being this an important advantage for the female caring physicians that during lockdown also took care of their children, being the schools closed.
Other models of remote monitoring of patients with chronic severe cutaneous diseases as psoriasis and acne have been tested in the past, as online, collaborative‐health model (asynchronous telemedicine) and mobile phone based teledermatology systems with successful results. 7 , 8 , 9 , 10 Such systems have the disadvantage that require access to new technologies (smart‐phones, computers, etc) by patients. As stated above, in order to maximize promptly patient care and support we organized in an urgent manner the remote monitoring system using telephone and emails in order to reach the maximum possible number of patients.
In conclusion, due to the lack of a teledermatology platform we were forced to use the telephone and email as RMTs; in the future it will be ideal to have a teledermatology service platform that fulfills all the privacy, quality checks and legal regulations allowing also reimbursement of the activity performed.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
Brunasso AMG, Massone C. Teledermatologic monitoring for chronic cutaneous autoimmune diseases with smartworking during COVID‐19 emergency in a tertiary center in Italy. Dermatologic Therapy. 2020;33:e13495. 10.1111/dth.13695
REFERENCES
- 1. Gisondi P, Piaserico S, Conti A, Naldi L. Dermatologists and SARS‐CoV‐2: the impact of the pandemic on daily practice. J Eur Acad Dermatol Venereol. 2020. 10.1111/jdv.16515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Omboni S. Telemedicine during the COVID‐19 in Italy: a missed opportunity? Telemed J E Health. 2020. 10.1089/tmj.2020.0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Villani A, Scalvenzi M, Fabbrocini G. Teledermatology: a useful tool to fight COVID‐19. J Dermatol Treat. 2020;31(4):325. [DOI] [PubMed] [Google Scholar]
- 4. Perkins S, Cohen JM, Nelson CA, Bunick CG. Teledermatology in the era of COVID‐19: experience of an Academic Department of Dermatology. J Am Acad Dermatol. 2020. 10.1016/j.jaad.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jakhar D, Kaul S, Kaur I. WhatsApp messenger as a teledermatology tool during coronavirus disease (COVID‐19): from bedside to phone‐side. Clin Exp Dermatol. 2020. 10.1111/ced.14227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID‐19. N Engl J Med. 2020;382:1679‐1681. [DOI] [PubMed] [Google Scholar]
- 7. Bashi N, Karunanithi M, Fatehi F, Ding H, Walters D. Remote monitoring of patients with heart failure: an overview of systematic reviews. J Med Internet Res. 2017;19:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Armstrong AW, Chambers CJ, Maverakis E, et al. Effectiveness of online vs in‐person care for adults with psoriasis: a randomized clinical trial. JAMA Netw Open. 2018;1:e183062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Armstrong AW, Ford AR, Chambers CJ, et al. Online care versus in‐person care for improving quality of life in psoriasis: a randomized controlled equivalency trial. J Invest Dermatol. 2019;139:1037‐1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Koller S, Hofmann‐Wellenhof R, Hayn D, et al. Teledermatological monitoring of psoriasis patients on biologic therapy. Acta Derm Venereol. 2011;91:680‐685. [DOI] [PubMed] [Google Scholar]


