Editor
The 2019‐nCoV outbreak occurred in Wuhan, China in December 2019. 1 This unprecedented virus has caused global pandemic and over 2 300 000 cases worldwide in total number, 2 which has been bringing tremendous pressure and challenges to medical institutions and clinical staff around the world. 2019‐nCoV can be transmitted by droplets primarily, while it has been reported that surface contact transmission exists as well. 3 Keeping the integrity of skin barrier is a critical method to prevent the spread of 2019‐nCoV, since skin is the first line of defence of human body. 4 It is of prime importance to ensure and maintain the skin clean, sterilized and protected of clinical healthcare staff during the fight against the epidemic. Self‐protection of the medical staff is essential, however, utilizing protective equipment such as goggles, masks and protective clothing continuously impairs skin integrity and the skin damage caused by the respective protective measures must be taken seriously.
To investigate the skin conditions of the front‐line medical staff during the outbreak of 2019‐nCoV, and identify any correlations between skin injury and the protection. We created an online questionnaire survey on skin problems in 484 clinical front‐line medical staff in China during the period of 2019‐nCoV and the results are as follows.
Among the 484 participants, half of them was from Wuhan and half was from the other 11 provinces of China. Female workers accounted for more than three quarters of the total (75.8%), the rest were males. The age distribution of the medical staff divided into four groups (Fig. 1a). The department of the medical staff was shown in Fig. 1b. The protection level of the participants was divided into three levels. 18.2%, 64.1% and 17.2% of participants were equipped with biosafety level 1, 2 or 3, respectively (Fig. 1c). More than half of the participants wore the protective suit between 4 and 6 h at a time and 9.1% of them kept the suit on for longer than 6 h (Fig. 1d). 64.2% of the staff worked 3–5 days a week, 12.4% of the staff worked more than 5 days a week, and 11.8% worked 1–2 days a week (Fig. 1e). To determine the degree of itching, we let participants grade their symptom into three intensity levels. 61.8% of the participants have various degrees of pruritus, the proportion is 45.5% (mild), 15.1% (moderate) and 1.2% (severe; Fig. 1f, degree of itching is demonstrated in legend). Among the 484 participants, 73.1% suffered from various skin lesions. The lesions manifested as erythema (38.8%), prurigo (22.9%), blisters (13.8%), rhagades (13.6%), papule/oedema (12.8%), exudation/crust (6.8%) and lichenification (5.6%) (Fig. 1g). The distribution of the lesions was wide. Nearly, half of the lesions were located on the face (47.1%), followed by the hands (27.5%), limbs (15.7%), truncus (12.6%) and the whole body (2.3%) (Fig. 1h).
Figure 1.
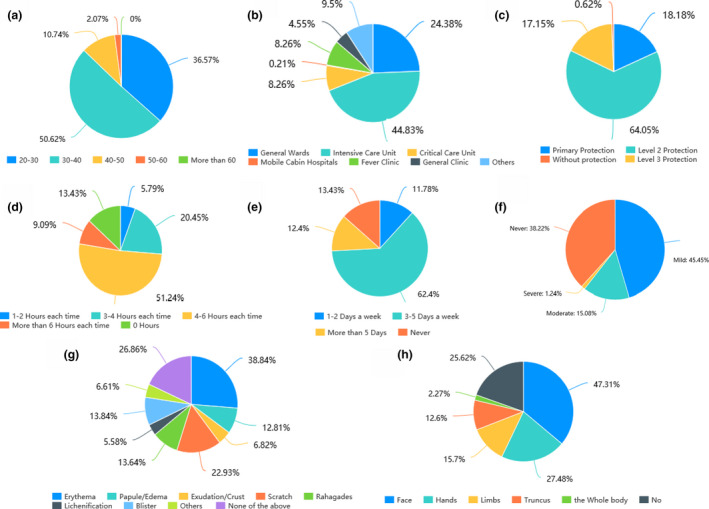
(a) Age distribution of the medical staff. Half of the staff were between 30 and 40 years old (50.6%), and followed by 20–30 years old (36.6%), 40–50 years old (10.7%) and 50–60 years old (2.1%). (b) Department of the medical staff. Nearly, half of the participants worked in the intensive care unit (44.8%), followed by general wards (24.4%), critical care unit and fever clinic (both 8.3%), general clinic (4.6%) and mobile cabin hospitals (0.2%). (c) Protection level of the participants. The proportion of the primary protection, level 2 protection and level 3 protection was 18.2%, 64.1% and 17.2%, respectively. (Biosafety level 1 protection included wearing overalls, disposable hats, disposable surgical masks, disposable isolation clothing and disposable gloves. Level 2 protected personnel wore overalls, disposable hats, medical protective masks such as N95, goggles or protective masks, and as outer cover a medical protective suit with disposable gloves. Finally, level 3 protection was defined as the same combination as in level 2 but with addition of face mask, or a medical mask, goggles or face mask to a full set or with electric air filter respirator). (d) Duration of using the protective suits. More than half of the participants wearing the protective suit between 4 and 6 h per time and 9.1% of them wearing the suit over 6 h. (e) Working frequency. 64.2% of the staff worked 3–5 days a week, 12.4% of the staff worked more than 5 days a week, and 11.8% worked 1–2 days a week. (f) Degree of itching. 61.8% of the participants had various degrees of pruritus. 45.5% has mild, non‐irritating pruritus, 15.1% were irritated by moderate pruritus, which, however, did not affect them during off‐duty time. 1.2%, however, had severe itching, which negatively affected sleep and impaired their overall well‐being outside the hospital. (g) Type of the lesions. 73.1% of the participants suffered from different type of lesions. The lesions manifested as erythema (38.8%), scratch (22.9%), blister (13.8%), rahagades (13.6%), papule/oedema (12.8%), exudation/crust (6.8%) and lichenification (5.6%). (h) The distribution of the lesions. Nearly, half of the lesions performed on face (47.1%), followed by hands (27.5%), limbs (15.7%), truncus (12.6%) and the whole body (2.3%).
Our correlation analysis showed that medical staff with level 2&3 protection were more likely to experience itching than those using primary protection (P = 0.0121). More advanced protection (P = 0.0016), higher working frequency (P < 0.001) and longer wearing times of protective suits (P = 0.0016) were more correlated with the appearance of facial skin lesions (P = 0.0006). The occurrence of erythema is related to protection level (P = 0.0021), working frequency (P < 0.001) and the duration of wearing protective suit (P = 0.0006; Table 1).
Table 1.
(A) The correlation between the protection level and the degree of itching, site of the lesions and the type of the lesions, (B) The correlation between the working frequency and the degree of itching, site of the lesions and the type of the lesions. (C) The correlation between the duration of wearing protection suit and the degree of itching, site of the lesions and the type of the lesions
| (A) | ||||
|---|---|---|---|---|
| Characteristics | Total | The protection level | P value | |
| Primary protection | Level 2&3 protection | |||
| Itching or not | ||||
| Mild, moderate & severe n, (%) | 297 (100) | 44 (14.8) | 253 (85.2) | 0.0121 |
| Never | 184 (100) | 44 (23.9) | 140 (76.1) | |
| Site of the lesions | ||||
| Face, n, (%) | 229 (100) | 28 (12.2) | 201 (87.8) | 0.0016 |
| Hands, n, (%) | 131 (100) | 20 (15.3) | 111 (84.7) | 0.3584 |
| Type of the lesions | ||||
| Erythema, n, (%) | 187 (100) | 21 (11.2) | 166 (88.8) | 0.0021 |
| Papule/oedema, n, (%) | 62 (100) | 8 (12.9) | 54 (87.1) | 0.3170 |
| Exudation/crust, n, (%) | 33 (100) | 3 (9.1) | 30 (90.9) | 0.2365 |
| Scratch, n, (%), | 111 (100) | 13 (11.7) | 98 (88.3) | 0.0567 |
| Rahagades, n, (%) | 65 (100) | 8 (12.3) | 57 (87.7) | 0.2420 |
| Lichenification, n, (%) | 27 (100) | 8 (29.6) | 19 (70.4) | 0.1896 |
| Blister, n, (%) | 67 (100) | 11 (16.4) | 56 (83.6) | 0.7963 |
| (B) | ||||
|---|---|---|---|---|
| Characteristics | Total | The working frequency | P value | |
| 0–2 days | More than 3 days | |||
| Itching or not | ||||
| Mild, moderate & severe n, (%) | 299 (100) | 63 (21.1) | 236 (78.9) | 0.0899 |
| Never | 150 (100) | 24 (16) | 126 (84) | |
| Site of the lesions | ||||
| Face, n, (%) | 229 (100) | 37 (14.8) | 192 (85.2) | <0.001 |
| Hands, n, (%) | 133 (100) | 30 (22.6) | 103 (77.4) | 0.4781 |
| Type of the lesions | ||||
| Erythema, n, (%) | 188 (100) | 27 (14.4) | 161 (85.6) | <0.001 |
| Papule/oedema, n, (%) | 62 (100) | 9 (14.5) | 53 (85.5) | 0.0549 |
| Exudation/crust, n, (%) | 33 (100) | 3 (9.1) | 30 (90.9) | 0.0454 |
| Scratch, n, (%) | 111 (100) | 17 (15.3) | 94 (84.7) | 0.0091 |
| Rahagades, n, (%) | 66 (100) | 17 (25.8) | 49 (74.2) | 1 |
| Lichenification, n, (%) | 27 (100) | 8 (29.6) | 19 (70.4) | 0.7515 |
| Blister, n, (%) | 67 (100) | 15 (22.4) | 52 (77.6) | 0.6738 |
| (C) | ||||
|---|---|---|---|---|
| Characteristics | Total | The duration of wearing protection suit | P value | |
| 0–4 h | More than 4 h | |||
| Itching or not | ||||
| Mild, moderate & severe, n, (%) | 299 (100) | 111 (37.1) | 188 (62.9) | 0.6474 |
| Never | 185 (100) | 81 (43.8) | 104 (56.2) | |
| Site of the lesions | ||||
| Face, n, (%) | 229 (100) | 72 (31.4) | 157 (68.6) | 0.0006 |
| Hands, n, (%) | 133 (100) | 50 (37.6) | 83 (62.4) | 0.6380 |
| Type of the lesions | ||||
| Erythema, n, (%) | 188 (100) | 54 (28.7) | 134 (71.3) | 0.0001 |
| Papule/oedema, n, (%) | 62 (100) | 22 (35.5) | 40 (64.5) | 0.5603 |
| Exudation/crust, n, (%) | 33 (100) | 8 (24.2) | 25 (75.8) | 0.0906 |
| Scratch, n, (%) | 111 (100) | 33 (29.7) | 78 (70.3) | 0.0199 |
| Rahagades, n, (%) | 66 (100) | 27 (40.9) | 39 (59.1) | 0.9313 |
| Lichenification, n, (%) | 27 (100) | 13 (48.1) | 14 (51.2) | 0.4688 |
| Blister, n, (%) | 67 (100) | 22 (32.8) | 45 (67.2) | 0.2725 |
Based on the above findings, the occurrence of skin lesions of front‐line medical staff is closely related to the level of protection, working frequency and duration of wearing protective suits. Therefore, to avoid decimation of the active workforce due to irritated skin, we recommend the implementation of effective measures to ensure the integrity of skin barrier of the front‐line medical staff, what is more the dermatologist's intervention is necessary.
Contributor Information
X. Chen, Email: chenxiangck@126.com.
M. Yin, Email: yinmingzhu2008@126.com.
References
- 1. Chen N, Zhou M, Dong X et al. Zhang L Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet (London, England) 2020; 395: 507–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. WHO . Coronavirus disease (COVID‐2019) situation reports, 2020. URL https://www.who.int/emergencies/diseases/novel‐coronavirus2019/situation‐reports/ (last accessed: 21 April 2020).
- 3. Chan JF, Yuan S, Kok KH et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person‐to‐person transmission: a study of a family cluster. Lancet (London, England) 2020; 395: 514–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Toncic RJ, Jakasa I, Hadzavdic SL et al. Altered levels of sphingosine, sphinganine and their ceramides in atopic dermatitis are related to skin barrier function, disease severity and local cytokine milieu. Int J Mol Sci 2020; 21: 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]


