Dear Editor,
In the city of Wuhan (Hubei province) in China, during the month of December 2019, an inexplicable increase in number of atypical pneumonia cases arose. 1 The cause of these pneumonias has been related to a zoonotic‐transmitted virus named severe acute respiratory syndrome coronavirus 2 (SARS‐Cov‐2), which leads to the resultant disease named as coronavirus disease 2019 (COVID‐19). 1 , 2
The main initial clinical manifestations of SARS‐Cov‐2 infection are: fever, dry cough, rhinorrhea, fatigue, arthralgias, myalgias, and headache. The onset of a dyspnea associated with an underlying bilateral interstitial pneumonia is a complication of this infection, causing a respiratory failure that in some cases requires invasive or noninvasive mechanical ventilation. In addition, a large number of recent cases characterized by viral‐related thrombophilic vasculitis are increasingly observed. A mild leukopenia and an elevation of lactate dehydrogenase (LDH) can be present in COVID‐19 patients. 1 Finally, neurological symptoms (such as ageusia and anosmia) also highlight a neurological tropism of SARS‐Cov‐2. In most cases, the disease passes asymptomatically or with only mild symptoms without requiring any hospitalization with only a period of quarantine at home. 4
As with all other viral diseases, the skin can also be affected in COVID‐19 patients. A 37‐year‐old Caucasian woman, in her 7th postpartum day, developed fever (up to 39 °C), dry cough, myalgia, and arthralgia; her husband developed the same symptoms. Her personal medical history was negative for cutaneous and internal diseases, she denied any allergies, the childbirth had no complications, and routine laboratory investigations did not show abnormalities. Five days before the onset of these symptoms, the patient had direct contact with an asymptomatic COVID‐19 patient, confirmed with a nasopharyngeal and oropharyngeal swab. There were no signs of dyspnea, and the vital signs (including saturation) were all in normal range. A diagnosis of COVID‐19 was made. The patient was obligated to quarantine at home and was advised to come to the hospital only in the event of clinical worsening. A symptomatic treatment with only acetaminophen was prescribed. Breastfeeding has not been suspended.
After 3 days from the onset of the symptoms and in her 10th postpartum day, the patient developed a craniocaudal cutaneous manifestation characterized by erythematous maculopapular lesions on the trunk, neck, and face (Fig. 1a–c). Additionally, there were cutaneous lesions characterized by nummular erythematous lesions with a peripheral slight white halo, assuming an urticaria‐like feature in the lower limbs (Fig. 2). She denied itching. The patient emailed us a photo of the cutaneous lesions, and a medical call was also performed. After 8 days, the cutaneous lesions clearly improved along with improvement of the general symptoms and absence of fever and dry cough. The newborn did not show any symptom of the disease and did not develop any cutaneous lesion. Her husband also showed a clear general improvement without having developed any cutaneous lesion.
Figure 1.
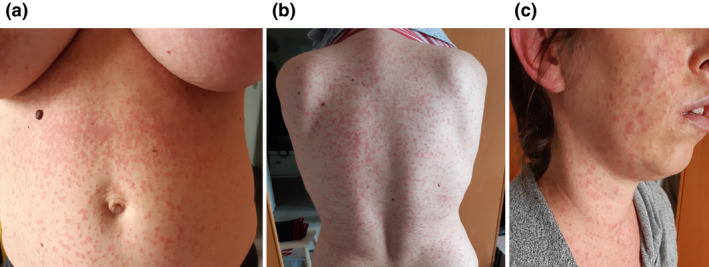
(a) Erythematous maculopapular lesions on the trunk in the absence of itching. (b) Erythematous maculopapular lesions on the trunk, with more erythema in the back. (c) Involvement of the head‐neck region. The lesions showed a craniocaudal development
Figure 2.

Nummular erythematous lesions with a peripheral slight white halo, assuming urticaria‐like features, specifically resembling an adrenergic urticaria
Currently, there are only two articles that described a total of 19 cases of cutaneous manifestations in COVID‐19 patients, mainly characterized by erythematous rash, widespread urticaria, chickenpox‐like vesicles, with a predilection for the trunk 1 and one case presenting with a skin rash with petechiae resembling dengue. 5 However, in both articles, the authors did not report any picture of the described cutaneous lesions. 1 , 2 , 3 , 4 , 5 While there are two recent reports that highlight the presence of acro‐ischemia due to an existence of hypercoagulation status associated with COVID‐19, this was not observed in our patient. 5 , 6
Our case shows a cutaneous manifestation in a new mother with COVID‐19 characterized by the simultaneous presence of erythematous, maculopapular lesions and urticaria‐like skin lesions, further highlighting the variety of the clinical features which are associated with this new disease, still little known. Again, our case highlights that newborns and children in 97% of cases do not develop severe respiratory symptoms, without showing clear clinical manifestations, although they can be an important viral reservoir. 7 Women with COVID‐19 can breastfeed. Moreover, our case also highlights how telemedicine plays a very important role in supporting patients confined at home during the coronavirus pandemic emergency.
Acknowledgment
We thank Matteo Riccardo Di Nicola for the technical support.
Conflict of interest: None.
Funding source: None.
References
- 1. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16387. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2. Koo JR, Cook AR, Park M, et al. Interventions to mitigate early spread of SARS‐CoV‐2 in Singapore: a modeling study. Lancet Infect Dis 2020. pii: S1473‐3099(20)30162‐6. 10.1016/S1473-3099(20)30162-6. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model‐based analysis. Lancet Infect Dis 2020. pii: S1473‐3099(20)30243‐7. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Joob B. Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for Dengue. J Am Acad Dermatol 2020. pii: S0190‐9622(20)30454‐0. 10.1016/j.jaad.2020.03.036. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhang Y, Cao W, Xiao M, et al. Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi 2020; 41: E006. [DOI] [PubMed] [Google Scholar]
- 6. Mazzotta F, Troccoli T. Acute acro‐ischemia in the child at the time of COVID19. Eur J Pediatr Dermatol 2020. [Epub ahead of print]. [Google Scholar]
- 7. Dong Y, Mo X, Hu Y, Qi X, Jiang F, Jiang Z, Tong S. Epidemiological Characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics 2020. pii: e20200702. [Epub ahead of print]. [Google Scholar]


