Abstract
During the ongoing COVID‐19 pandemic, healthcare professionals are at the forefront of managing the highly infectious coronavirus. As the most common route of transmission is via aerosols and droplet inhalation, it is critical for healthcare workers to have the correct personal protective equipment (PPE) including gowns, masks and goggles. Surgical masks are not effective in preventing the influenza and SARS, so they are unlikely to be able to resist contaminated aerosols from entering the respiratory system. Therefore, it is vital to use respirators which have been proven to offer better protection against droplets, aerosols and fluid penetration and which form a tight seal around the mouth and nose. Various types of respirators are used in healthcare settings, such as half‐mask filtering facepiece respirators (FFRs) and powered air‐purifying respirators (PAPRs). The most commonly used FFR is the N95 disposable respirator, which is tight fitting and has a 95% or above particle filtering efficiency for a median particle size of 0.3 µm. This review discusses respirators, their purpose, types, clinical efficiency and proper donning and doffing techniques.
Keywords: COVID‐19, masks, pandemic, respirators
Introduction
With the emerging outbreak of the coronavirus pandemic, millions of people throughout the world are staying at home to contain the spread of disease and contribute to flattening the curve associated with the rapid rise in the number of cases. However, healthcare professionals will not be staying home. Indeed, they belong to a group of individuals who will be particularly vulnerable to contracting the infection (Dave et al. 2020), which has been reported to be as high as 29% in Wuhan, China (Wang et al. 2020). In this context, the Occupational Safety and Health Administration (OSHA) within the Department of Labor, USA, has developed an occupational risk pyramid which defines the risk of healthcare providers based on exposure (https://www.osha.gov/Publications/OSHA3990.pdf; United States, Department of Labour). According to the OSHA, dental healthcare providers (DHCPs) are classified as ‘very high risk’. For this reason, the personal protective equipment (PPE) requirements for DHCPs have been modified to include the wearing of impermeable gowns, goggles or face shields and N95 or better respirators in addition to standard precautions (Meng et al. 2020).
The recommendation for a N95 respirator is unique for dentistry and requires a detailed discussion on, its types, alternatives, donning and doffing techniques and fit testing.
Why is a respirator required?
According to the information available, the most common transmission routes for severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) or COVID‐19 are through droplet transmission via direct face‐to‐face contact between patients and dental healthcare providers (DHCPs), coughing or sneezing and indirect transmission by touching surfaces that were contaminated by the virus and then touching face, nose or eyes and through coarse or small droplets of saliva whilst performing aerosol generating procedures such as laryngoscopy or dental treatments (Peng et al. 2020, Prati et al. 2020). The SARS‐CoV‐2 virus has an affinity for the angiotensin‐converting enzyme 2 (ACE‐2) receptor, which is in abundance in the respiratory tract and salivary gland duct epithelium, and therefore, the saliva is very likely to contain a high viral load (Liu et al. 2011). Micik and colleagues were the first to define aerosols in dentistry as particles of size less than 50 µm which were able to stay airborne for extended periods of time before eventually settling in the environment and or inhaled into the respiratory system (Micik et al. 1969). The particle size of 0.5–10 µm is of distinct importance as they are most likely to transmit infection (Micik et al. 1969). This has been validated by numerous studies, and there is strong evidence which indicates that severe acute respiratory distress syndrome virus (SARS) spreads through aerosol transmission. It would be completely logical to assume that COVID‐19, which is similar to SARS, can likewise spread through aerosols (Jones & Brosseau 2015, Centers for Disease Control and Prevention: https://www.cdc.gov/sars/guidance/i‐infection/healthcare.html (accessed 21 April 2020)).
Do surgical masks offer protection from COVID‐19?
Since the outbreak, there is a lack of data comparing the efficacy of surgical mask versus respirators in mitigating the spread of COVID‐19 virus; however, there is an abundance of published data comparing the two against the influenza virus and SARS (Seto et al. 2003, Teleman et al. 2004).
Wen and colleagues tested the performance of various respirators and surgical masks against viral aerosols and demonstrated that the protection factor of N95 was thirty times greater than normal surgical masks (Wen et al. 2013). Likewise, the superiority of N95 over surgical masks has also been demonstrated against SARS in a number of case–control studies (Seto et al. 2003, Teleman et al. 2004).
Conversely, a recent systematic review and meta‐analysis failed to demonstrate the superiority of N95 respirators over surgical masks during influenza pandemics (Long et al. 2020). The reasons suggested by the authors for the conflicting results were the high risk of bias in the randomized control trials, low compliance of wearing the N95 respirator and frequent doffing as the respirator was uncomfortable to wear for longer periods of time (Long et al. 2020). To sum up, faced with the emergence of a virulent disease such as COVID‐19 it would be logical to use a respirator as it offers resistance to fluid penetration and forms a seal around the mouth and nose in contrast to surgical masks that provide barrier protection only against droplets including large respiratory particles. Most surgical masks lack an adequate face seal and do not effectively filter small particles from the air or aerosols, allowing for leakage around the mask and subsequent exposure (Wen et al. 2013). Furthermore, the American Dental Association (ADA) recommends an isolation of 14 days for both the DHCP and the patient if an aerosol generating procedure was performed using only a surgical mask and/or a COVID test be performed on the patient (https://www.ada.org/en/member‐center/coronavirus‐resource‐toolkit‐for‐ada‐members).
What are the different types of respirators?
There is a range of respirators including full‐ and half‐mask types. The common types of respirators that are used in healthcare settings include half‐mask filtering facepiece respirators (FFRs) and powered air‐purifying respirators (PAPRs). Since all dental guidelines recommend using FFRs, they are discussed in greater detail (Chughtai et al. 2020). The most widely used FFRs are the N95 respirators, which are disposable filtering facepiece respirators (FFRs) that tightly fit to provide optimum face seal and have a 95% or above particle filtering efficiency for a median particle size of 0.3 µm (Bergman et al. 2015).
The prefix N is a description of the filter material (N = oil nonresistant, R = some resistance to oil and P = oil proof) and suffix 95 describes its protective properties (95 would filter 95% particles whilst 99 filters 99% particles) (Bollinger 2004).
They come in a variety of shapes, for example cup‐shaped 1860 (3M™, St. Paul, MN, United States), flat‐fold 1870 (3M™) and duckbill PFR95‐270 (Kimberly Clark Corp., Dallas, TX, United States). These variations allow for better fit and comfort for different face types. Some masks have exhalation valves that tend to keep the face cooler and prevent moisture build‐up. The masks with an exhalation valve should not be used when working under sterile conditions (Bollinger 2004).
The respirators mentioned below according to 3M™ are equivalent in performance to N95 (United States NIOSH‐42CFR84) and may be considered as viable alternatives to N95 (https://multimedia.3m.com/mws/media/957730O/respirators‐and‐surgical‐masks‐contrast technical‐bulletin.pdf).
FFP2 (Europe EN 149‐2001)
KN95 (China GB2626‐2006)
P2 Particulate respirator (1716:2012; 3M ™ Australia/New Zealand)
Korea 1st class (Korea KMOEL‐2017‐64)
DS (Japan JMHLW‐Notification 214, 2018)
Which model should i choose?
Fit testing is needed to determine whether a particular size and model of respirator provide an acceptable fit. The benefit of the FFR will be negated if it does not form a tight seal around the face and nose; therefore, a process of individual fit testing is required (OSHA Respiratory Protection standard 29 CFR 1910.134) and this should be repeated periodically (Bergman et al. 2015). There are two types of fit tests available, which include qualitative and quantitative tests.
The qualitative test is graded as adequate if the test subject does not detect the sweet or bitter taste of saccharin or Bitrex (a solution containing 95% water, 5% sodium chloride and < 0.1% denatonium benzoate), respectively, whilst performing a series of test exercises. Whilst the quantitative fit test is done by using ambient aerosols to numerically estimate how well the N95 fits the user by measuring the aerosol particle ratio outside (C o) and inside (C i) the device. Nonetheless, studies demonstrate that fit testing with either method provides the expected levels of protection (Shaffer & Janssen 2015). Studies have shown that varying pass rates for fit tests range from 10% to 80% indicating that one size does not fit all (McMahon et al. 2008, Winter et al. 2010, Huh et al. 2018).
To date, there have been hundreds of approved N95 models that are available and it is difficult to predict which type of respirator will be the best fit in a given population. A fit testing programme is recommended for dental healthcare providers, in which the selection of the most suitable model should be made by an experienced fit tester who would determine the best fit based on facial dimensions, ethnicity and appearance of fit. These recommendations have proven to be useful in the past (McMahon et al. 2008, Wilkinson et al. 2010, Danyluk & Hon 2011).
Donning and doffing of FFRs
Correct donning and doffing procedures are the key to use of PPE, and all efforts should be made to prevent contamination during wearing and removal of respirators. Therefore, stringent surveillance on proper PPE use is critical for preventing disease transmission to healthcare workers. Previous studies show poor adherence with donning and doffing protocols lead to self‐contamination (Beam et al. 2011, Casanova et al. 2016). There are no universally accepted donning and doffing sequences but having a check list or instructions (Figs 1 and 2) are useful. Having full body mirrors for self‐assessment and external observers have also proven to be helpful in preventing self‐contamination (Aguilar & Linsuwanont 2011).
Figure 1.
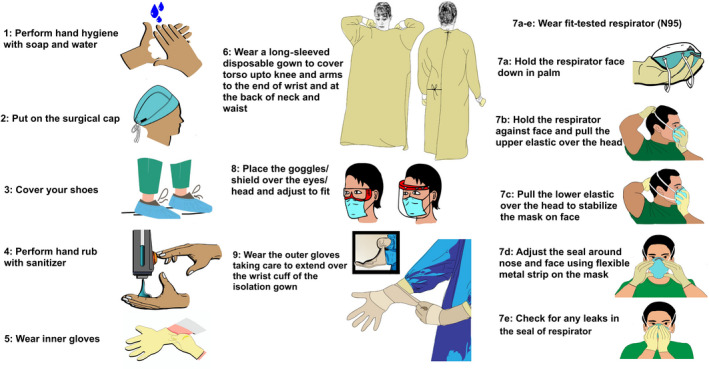
Donning of PPE.
Figure 2.
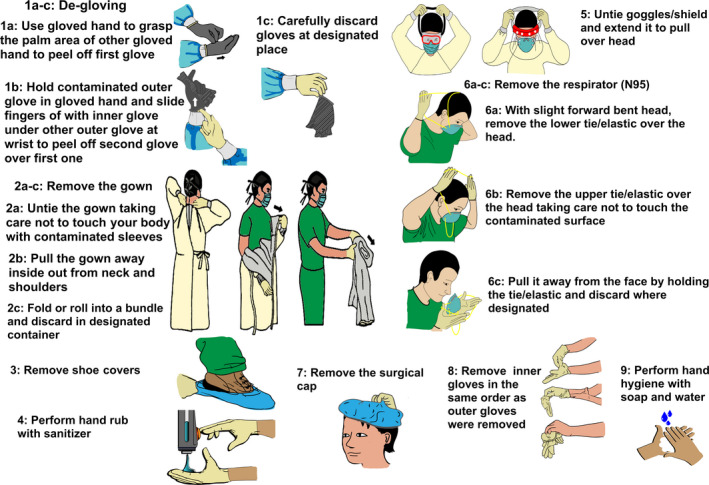
Doffing of PPE.
Reuse and decontamination of FFRs
Respirators are meant for single use only; however, reuse may be allowed in a crisis situation to conserve resources. The COVID‐19 virus is able to survive on plastic, stainless steel and cardboard for up to 72 h (van Doremalen et al. 2020). Therefore, there is a chance that the outer surface of respirators could become contaminated with aerosol, which can later be transferred to the user during donning and doffing procedures. Ultraviolet germicidal irradiation (UVGI), vaporous hydrogen peroxide (VHP) and moist heat are the most promising decontamination procedures, but there are is no literature which supports their efficacy against COVID‐19. Nevertheless, caution is advised as decontamination procedures can have negative impact on the respirator performance as well as the fit of the respirator. It is also recommended to contact the vendor for best decontamination practices (Bergman et al. 2010, Aguilar & Linsuwanont 2011, van Straten et al. 2020).
Conclusion
It is essential to use FFRs during the pandemic of COVID‐19 to prevent aerosol and droplet transmission as they are proven to offer resistance against fluid penetration and forms a seal around the mouth and nose better than surgical masks. The success of any FFR in preventing the inhalation of contaminant particles is also subject to an acceptable fit test and proper donning and doffing. The most commonly used FFR is the N95 respirator to prevent the transmission of disease.
Conflict of interest
The authors have stated explicitly that there are no conflicts of interest in connection with this article.
Umer F, Haji Z, Zafar K. Role of respirators in controlling the spread of novel coronavirus (COVID‐19) amongst dental healthcare providers: a review. International Endodontic Journal, 53, 1062–1067, 2020.
References
- Aguilar P, Linsuwanont P (2020) Vital pulp therapy in vital permanent teeth with cariously exposed pulp: a systematic review. Journal of Endodontics 37, 581–7. [DOI] [PubMed] [Google Scholar]
- Beam EL, Gibbs SG, Boulter KC, Beckerdite ME, Smith PW (2011) A method for evaluating health care workers’ personal protective equipment technique. American Journal of Infection Control 39, 415–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman MS, Viscusi DJ, Heimbuch BK, Wander JD, Sambol AR, Shaffer RE (2010) Evaluation of multiple (3‐cycle) decontamination processing for filtering facepiece respirators. Journal of Engineered Fibers and Fabrics 5, 155892501000500405. [Google Scholar]
- Bergman M, Zhuang Z, Brochu E, Palmiero A (2015) Fit assessment of N95 filtering‐facepiece respirators in the US Centers for Disease Control and Prevention Strategic National Stockpile. Journal of the International Society for Respiratory Protection 32, 50. [PMC free article] [PubMed] [Google Scholar]
- Bollinger NJ (2004) NIOSH respirator selection logic: US Department of Health and Human Services, Public Health Service,Centers. [Google Scholar]
- Casanova LM, Teal LJ, Sickbert‐Bennett EE et al. (2016) Assessment of self‐contamination during removal of personal protective equipment for Ebola patient care. Infection Control & Hospital Epidemiology 37, 1156–61. [DOI] [PubMed] [Google Scholar]
- Chughtai AA, Seale H, Rawlinson WD, Kunasekaran M, Macintyre CR (2020) Selection and use of respiratory protection by healthcare workers to protect from infectious diseases in hospital settings. Annals of Work Exposures and Health 64, 1–10. [DOI] [PubMed] [Google Scholar]
- Danyluk Q, Hon C‐Y (2011) Strengthening N95 filtering facepiece respirator protection programs by evaluating the contribution of each of the program elements. Richmond, British Columbia, Canada: Workers’ Compensation Board of British Columbia. [Google Scholar]
- Dave M, Seoudi N, Coulthard P (2020) Urgent dental care for patients during the COVID‐19 pandemic. The Lancet 395, 1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huh YJ, Jeong HM, Lim J et al. (2018) Fit characteristics of N95 filtering facepiece respirators and the accuracy of the user seal check among Koreans. Infection Control and Hospital Epidemiology 39, 104–7. [DOI] [PubMed] [Google Scholar]
- Jones RM, Brosseau LM (2015) Aerosol transmission of infectious disease. Journal of Occupational and Environmental Medicine 57, 501–8. [DOI] [PubMed] [Google Scholar]
- Liu L, Wei Q, Alvarez X et al. (2011) Epithelial cells lining salivary gland ducts are early target cells of severe acute respiratory syndrome coronavirus infection in the upper respiratory tracts of rhesus macaques. Journal of Virology 85, 4025–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long Y, Hu T, Liu L et al. (2020) Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta‐analysis. Journal of Evidence‐Based Medicine 13, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon E, Wada K, Dufresne A (2008) Implementing fit testing for N95 filtering facepiece respirators: practical information from a large cohort of hospital workers. American Journal of Infection Control 36, 298–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng L, Hua F, Bian Z (2020) Coronavirus disease 2019 (COVID‐19): emerging and future challenges for dental and oral medicine. Journal of Dental Research 99, 481–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Micik RE, Miller RL, Mazzarella MA, Ryge G (1969) Studies on dental aerobiology: I. Bacterial aerosols generated during dental procedures. Journal of Dental Research 48, 49–56. [DOI] [PubMed] [Google Scholar]
- Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B (2020) Transmission routes of 2019‐nCoV and controls in dental practice. International Journal of Oral Science 12, 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prati C, Pelliccioni GA, Sambri V, Chersoni S, Gandolfi MG (2020) COVID‐19: its impact on dental schools in Italy, clinical problems in endodontic therapy and general considerations. International Endodontic Journal 53, 723–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto W, Tsang D, Yung R et al. (2003) Effectiveness of precautions against droplets and contact in prevention of nosocomial transmission of severe acute respiratory syndrome (SARS). The Lancet 361, 1519–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaffer RE, Janssen LL (2015) Selecting models for a respiratory protection program: what can we learn from the scientific literature? American Journal of Infection Control 43, 127–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teleman M, Boudville I, Heng B, Zhu D, Leo Y (2004) Factors associated with transmission of severe acute respiratory syndrome among health‐care workers in Singapore. Epidemiology and Infection 132, 797–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Doremalen N, Bushmaker T, Morris DH et al. (2020) Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. New England Journal of Medicine 382, 1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Straten B, de Man P, van den Dobbelsteen J, Koeleman H, van der Eijk A, Horeman T (2020) Sterilization of disposable face masks by means of standardized dry and steam sterilization processes; an alternative in the fight against mask shortages due to COVID‐19. Journal of Hospital Infection.https://doi:10.1016/j.jhin.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang D, Hu B, Hu C et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 323, 1061–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen Z, Yu L, Yang W et al. (2013) Assessment the protection performance of different level personal respiratory protection masks against viral aerosol. Aerobiologia 29, 365–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson IJ, Pisaniello D, Ahmad J, Edwards S (2010) Evaluation of a large‐scale quantitative respirator‐fit testing program for healthcare workers: survey results. Infection Control and Hospital Epidemiology 31, 918–25. [DOI] [PubMed] [Google Scholar]
- Winter S, Thomas JH, Stephens DP, Davis JS (2010) Particulate face masks for protection against airborne pathogens‐one size does not fit all: an observational study. Critical Care and Resuscitation 12, 24. [PubMed] [Google Scholar]


