Abstract
Objective
To determine whether COVID‐19 may adversely affect outcome of myocardial infarction (MI) patients in Hong Kong, China.
Background
The COVID‐19 pandemic has infected thousands of people and placed enormous stress on healthcare system. Apart from being an infectious disease, it may affect human behavior and healthcare resource allocation which potentially cause treatment delay in MI.
Methods
This was a single center cross‐sectional observational study. From November 1, 2019 to March 31, 2020, we compared outcome of patients admitted for acute ST‐elevation MI (STEMI) and non‐ST elevation MI (NSTEMI) before (group 1) and after (group 2) January 25, 2020 which was the date when Hong Kong hospitals launched emergency response measures to combat COVID‐19.
Results
There was a reduction in daily emergency room attendance since January 25, 2020 (group 1,327/day vs. group 2,231/day) and 149 patients with diagnosis of MI were included into analysis (group 1 N = 85 vs. group 2 N = 64). For STEMI, patients in group 2 tended to have longer symptom‐to‐first medical contact time and more presented out of revascularization window (group 1 27.8 vs. group 2 33%). The primary composite outcome of in‐hospital death, cardiogenic shock, sustained ventricular tachycardia or fibrillation (VT/VF) and use of mechanical circulatory support (MCS) was significantly worse in group 2 (14.1 vs. 29.7%, p = .02).
Conclusions
More MI patients during COVID‐19 outbreak had complicated in‐hospital course and worse outcomes. Besides direct infectious complications, cardiology community has to acknowledge the indirect effect of communicable disease on our patients and system of care.
Keywords: acute myocardial infarction/STEMI, ACS/NSTEMI, health care outcomes
1. INTRODUCTION
Since December 2019, the emergence of coronavirus disease (COVID‐19) in Wuhan, China has been spreading quickly and evolved into a pandemic. 1 As of early April 2020, COVID‐19 has infected more than 1.5 million people and killed more than 90,000. COVID‐19 is a viral infection causing respiratory system involvement 2 and its highly infectious nature mandates healthcare system to implement strict infection control measures to limit its virulence. Unprecedentedly, COVID‐19 place huge burden on every part of healthcare system directly and indirectly. Hong Kong, as a city in southern part of China, started to have imported cases in January followed by community outbreak swiftly afterwards. As a result, hospitals in Hong Kong launched the emergency response measures on January 25, 2020 to combat the outbreak. Previously, our group demonstrated that COVID‐19 could affect human behavior and healthcare resource allocation which led to treatment delay in acute myocardial infarction (MI). 3 We sought to investigate the impact of current COVID‐19 outbreak on MI outcome in our patients in Hong Kong.
2. METHODS
This was a single center cross‐sectional observational study of a hospital‐based registry. We included all patients with a diagnosis of acute ST‐elevation MI (STEMI) or non‐ST elevation MI (NSTEMI) presented to Accident and Emergency Department (AED) from November 1, 2019 to March 31, 2020 into analysis. We compared the characteristics and outcome of MI patients before and after January 25, 2020. Hospitals in Hong Kong launched emergency response measures on January 25, 2020 which mandated frequent environmental disinfection, universal surgical masking, full personal protective equipment (N95 respirator, goggles/face shield, isolated gown, disposable gloves) for aerosol‐generating procedures and suspension of all non‐essential visits, volunteer work and clinical attachment. Patients transferred from other hospitals and type 2 MI (with evidence of ischemia) or myocardial injury (without evidence of ischemia) were excluded in final analysis. 4 Our hospital is a tertiary referral center, which serves a population of 530,000 in a region in Hong Kong. Since 2010, the hospital offers 24/7 primary percutaneous coronary intervention (PPCI) service to all eligible patients with acute STEMI according to international guidelines with fibrinolytics as backup for anticipated excessive delay. We continued to perform PPCI for acute STEMI patients after January 25, 2020. Management for delayed presentation of STEMI and acute NSTEMI includes guideline directed medical therapy and coronary revascularization as indicated. 5 , 6 , 7 The primary outcome was a composite of in‐hospital death, cardiogenic shock, sustained ventricular tachycardia or fibrillation (VT/VF) and use of mechanical circulatory support (MCS). Cardiogenic shock was defined by systolic blood pressure <90 mmHg for at least 30 min with evidence of poor tissue perfusion after correction of non‐myocardial factors.
Continuous variables were reported as mean ± standard deviation (SD) or median and interquartile range (IQR) as appropriate. Categorical values were presented as absolute values or percentages. Comparison of continuous variables was performed by one‐way ANOVA, the Mann–Whitney U test, or the independent samples Kruskal–Wallis test, depending on data distribution. The Chi‐square and Fisher's exact tests were used for comparison of categorical values. A two‐sided p value of <.05 was considered statistically significant. All statistical analyses were performed using SPSS for Windows (version 19.0, SPSS Inc., Chicago, Illinois).
3. RESULTS
From November 1, 2019 to March 31, 2020, there was a marked decrease in AED attendance (Table 1) since January 25, 2020. In total, 225 patients were diagnosed to have acute MI. 23 transferred from other hospitals and 53 with type 2 MI/myocardial injury were excluded from final analysis (N = 149). Concerning STEMI, group 2 tended to have longer symptom‐to‐first medical contact (FMC) time and more presented out of revascularization window (Figure 1 and Table 1). For clinical outcome, more patients in group 2 seemed in‐hospital complicated course or worse outcome as shown by more in‐hospital death, cardiogenic shock, sustained VT/VF and use of MCS (group 1:14.1% vs. group 2 29.7%, p = .02).
TABLE 1.
Outcome of myocardial infarction patients before and after COVID‐19 response activation on January 25, 2020
| Group 1 01/11/2019–24/1/2020 (85 days) | Group 2 25/1/2020–31/3/2020 (66 days) | p Value | |
|---|---|---|---|
| AED attendance (per day) | 327 | 231 | |
| Acute myocardial infarction |
N = 85 |
N = 64 | |
| Age mean ± SD | 69.0 ± 15.1 | 69.4 ± 16.6 | .872 |
| Gender/male (%) | 56 (65.9%) | 45 (70.3%) | .599 |
| Smoker (%) | 17 (20.0%) | 12 (18.7%) | .531 |
| Hypertension (%) | 56 (65.9%) | 43 (67.2%) | 1.000 |
| Diabetes mellitus (%) | 30 (35.3%) | 24 (37.5%) | .864 |
| Previous MI (%) | 12 (14.1%) | 13 (20.3%) | .378 |
| Previous PCI (%) | 7 (8.2%) | 10 (15.6%) | .197 |
| Previous CABG (%) | 2 (2.4%) | 3 (4.7%) | .652 |
| Cerebrovascular disease or peripheral vascular disease (%) | 20 (23.5%) | 19 (29.7%) | .453 |
| STEMI | 36 | 27 | |
| 0.424/day | 0.409/day | ||
| NSTEMI | 49 | 37 | |
| 0.576/day | 0.561/day | ||
| Delayed STEMI | 10 | 9 | |
| 27.8% out of all STEMI | 33.3% out of all STEMI | ||
| Outcome | |||
| Cardiogenic shock (%) | 7 (8.2%) | 8 (12.5%) | .421 |
| Mechanical circulatory support (%) | 6 (7.1%) | 7 (10.9%) | .559 |
| VT/VF (%) | 2 (2.4%) | 5 (7.8%) | .140 |
| In‐hospital death (%) | 5 (5.9%) | 8 (12.5%) | .240 |
| Composite of in‐hospital death, cardiogenic shock, mechanical circulatory support and VT/VF (%) | 12 (14.1%) | 19 (29.7%) | .020 |
Abbreviations: AED, Accident and Emergency Department; CABG, Coronary artery bypass graft; ECG, Electrocardiogram; MI, Myocardial infarction; NSTEMI, Non‐ST elevation myocardial infarction; PCI, Percutaneous coronary intervention; STEMI, ST elevation myocardial infarction; VT/VF, Ventricular tachycardia/fibrillation.
FIGURE 1.
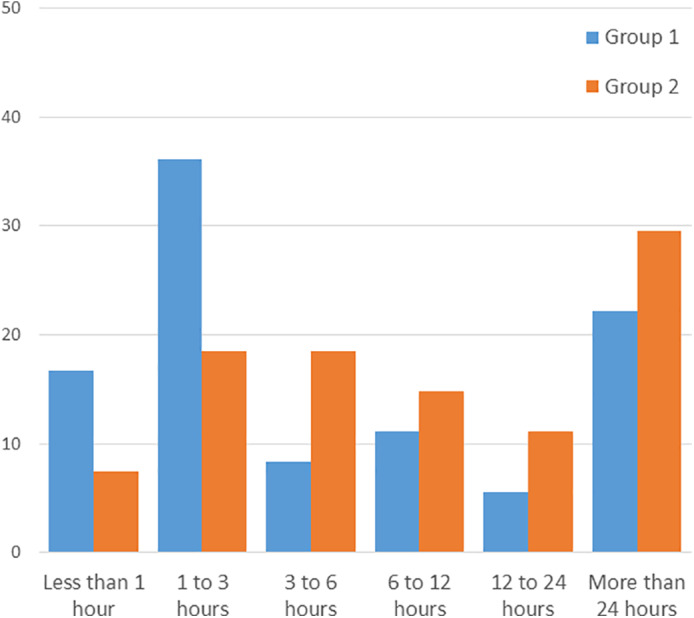
Symptom‐to‐first medical contact (FMC) time in group 1 and two patients with ST‐elevation myocardial infarction. Group 2 patients tended to have longer symptom‐to‐FMC time. The prolonged ischemic time in STEMI may translate into worse clinical outcomes
4. DISCUSSION
Despite severe direct cardiac damage is not dominant in COVID‐19, our preliminary report showed infectious disease outbreak can indirectly affect MI care and potentially lead to worse outcomes. It is well established that prompt diagnosis and treatment are important for MI and treatment delay is a predictor of adverse outcome. On January 25, 2020, Hong Kong hospitals implemented emergency response measures which are necessary and important for infection control. However, at the same time it may discourage people to promptly seek medical care which is crucial in the context of MI. We observed a reduction in AED attendance which is understandable. Nevertheless, MI patients tried to endure their symptoms until intolerant and eventually when they reached the hospital, many of them had prolonged ischemic time or out of window for revascularization. Besides, additional time may be required for potential infection containing measures such as detailed travel history taking, temperature measurement, chest X ray and staff protective gear changing etc. 3 All these will increase treatment delay and might have immediately translated into increase in mortality, incidence of cardiogenic shock and malignant arrhythmia. While in long run, more MI survivors may have heart failure which is debilitating and deadly.
Our data are preliminary and needed to be interpreted with cautions. This was a single center experience with limited patient number and human behavior may be different in different societies. Besides, patients and staff behavior may also change with time. Hopefully when people gain more experience, MI care system and outcome will improve with time in the midst of COVID‐19 outbreak. Moreover, we cannot evaluate whether some AMI patients did not seek any care at all or they may have died before any medical contact.
5. CONCLUSION
COVID‐19 outbreak may cause treatment delay in MI and potentially lead to worse clinical outcome. All hospitals not only have to prepare to fight against immediate infections and various healthcare professionals need to anticipate how different systems of care would be affected and act accordingly.
6. CONFLICT OF INTEREST
The authors declare no conflict of interest in relationship with manuscript content.
ACKNOWLEDGMENTS
The authors would like to thank Catherine SHEA, Timonthy UN, Chun Ka WONG, Will CHAN, Carmen CHAN, Yui Ming LAM, Tat Chi TSANG, Matthew TSUI and all healthcare workers sacrifice themselves in current COVID‐19 outbreak. This study received no specific grant from any funding agency in the public, commercial or not‐for‐profit sectors.
Tam C‐CF, Cheung K‐S, Lam S, et al. Impact of coronavirus disease 2019 (COVID‐19) outbreak on outcome of myocardial infarction in Hong Kong, China. Catheter Cardiovasc Interv. 2021;97:E194–E197. 10.1002/ccd.28943
REFERENCES
- 1. Cucinotta D, Vanelli M. WHO declares COVID‐19 a pandemic. Acta Biomed. 2020;91(1):157‐160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guan WJ, Ni ZY, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. 10.1056/NEJMoa2002032. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tam CF, Cheung KS, Lam S, et al. Impact of coronavirus disease 2019 (COVID‐19) outbreak on ST‐segment‐elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Circulation. 2018;138(20):e618‐e651. [DOI] [PubMed] [Google Scholar]
- 5. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non‐ST‐elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;130(25):e344‐e426. [DOI] [PubMed] [Google Scholar]
- 6. Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119‐177. [DOI] [PubMed] [Google Scholar]
- 7. Roffi M, Patrono C, Collet JP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST‐segment elevation: task force for the Management of Acute Coronary Syndromes in patients presenting without persistent ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267‐315. [DOI] [PubMed] [Google Scholar]


