Abstract
During the COVID‐19 pandemic, chilblain‐like lesions have been reported in mildly symptomatic children and adolescents. We present four children investigated for suspected COVID‐19 infection who presented with acral skin findings and mild systemic symptoms. Histology from one case showed signs of vasculitis with evident fibrin thrombus.
Keywords: infection‐viral, skin signs of systemic disease, vasculitis
1. INTRODUCTION
Since the first reports of cases from Wuhan (Hubei Province, China) at the end of 2019, a pandemic of COVID‐19 (novel severe acute respiratory syndrome coronavirus 2 or SARS‐CoV‐2) has spread worldwide. The clinical spectrum of infection ranges from mild to critical but many cases are asymptomatic or minimally symptomatic, the so‐called “invisible” patient. 1 Joob et al. 2 and Recalcati 3 have reported several non‐specific cutaneous manifestations, ranging from maculopapular rash to urticaria, in adults affected by COVID‐19 with no recent history of drug intake, excluding possible adverse drug reaction. Acro‐ ischemic lesions have been reported in hospitalized adult COVID‐19 patients. 4 Mazzotta et al. 5 reported a pediatric patient with similar findings and summarized that the lesions often occur in asymptomatic or mildly symptomatic children and adolescents and mainly affect the feet and hands, especially toes and fingers and also the plantar region and the heel. The number of reports is increasing in Italy and across many European countries and seems to overlap with the spread of the COVID‐19 pandemic.
2. PATIENT 1
On April 10, 2020, an 11‐year‐old girl from Milan (Lombardy region, Italy) was referred to Pediatric Dermatology Department by her pediatrician for a 14‐day history of lesions on the feet. Skin examination demonstrated several dusky erythematous macules with blurred edges , 5‐10 mm in diameter, located on the lateral margin of the feet and the dorsal surface of the right first, second, and third toes. On the plantar surface of the left first and fourth toes, the lesions appeared erythematous to cyanotic and slightly atrophic. The dorsal surface of the third and fourth toes was affected with an erythematous plaque (Figure 1). The upper limbs, face, trunk, genitals, and mucous membranes were spared. The lesions, initially faint, had become edematous and darker over a few days. They were associated with a feeling of coldness and mild pain. Her medical history revealed that the patient was in good health except for mild flu‐like symptoms with headache and rhinitis over the preceding weeks that did not require any treatment. During the same time, both parents had a cough. Based on the clinical findings and literature reports, an acro‐ischemia due to COVID‐19 infection was suspected. The girl and her father were tested for COVID‐19 with nasopharyngeal swab and aspirate. Both were negative. Antibody tesing for COVID‐19 was not available. No biopsy was performed. Laboratory testing, including complete blood count (CBC), liver and kidney function tests, C‐reactive protein (CRP), coagulation profile, ferritin, and fibrinogen, showed no abnormalities (D‐dimer test was not available because of in vitro hemolysis). Antiphospholipid antibodies (anti‐cardiolipin IgG and IgM), interleukin‐6 (IL‐6), and antinuclear antibody (ANA) were in the normal range. Cytomegalovirus (CMV), Epstein‐Barr virus (EBV), parvovirus B19 testing, and serology for Mycoplasma pneumoniae did not show recent infection. The skin lesions subsided without treatment within 5 days, leaving no sequelae.
FIGURE 1.

Patient 1, chilblains‐like lesions on the toes in an 11‐y‐old girl
3. PATIENT 2
On the same day as Patient 1, a 6‐year‐old girl from Monza (Lombardy region, Italy) was admitted to our Pediatric Emergency Department with a 2‐day history of vascular lesions on the feet. Erythematous, edematous 8‐10 mm rounded macules with blurred edges and a central erythematous‐cyanotic area were located on the bilateral plantar surfaces only (Figure 2). The lesions were itchy and moderately painful. Symptoms had begun 10 days prior and included mild intermittent fever and localized pain on soles. Her mother also reported fever during the previous month; her father had worked closely with a COVID‐19 positive individual but had remained asymptomatic. Both the girl and her mother were negative for COVID‐19 by nasopharyngeal swab and aspirate. Blood tests including CBC, CRP, coagulation panel, fibrinogen, ferritin, IL‐6, lupus anticoagulant, antinuclear antibody, and viral titers for CMV, EBV, and parvovirus B19 showed no abnormalities except for an elevated D‐dimer at 723 µg/L (<500 µg/L normal range). Due to the isolation restrictions, no biopsy was performed. Symptoms subsided without any therapy within 3 days, leaving no sequelae.
FIGURE 2.

Patient 2, moderately painful chilblains‐like lesions localized on the plantar surface of the first metatarsus in a 6‐y‐old girl
4. PATIENT 3
Four days later, on April 14, 2020, a 5‐year‐old boy from Milan (Lombardy region, Italy) was examined for similar vascular lesions on the feet and right hand, preceded by edema. On February 10, 2020, the child experienced fever and cough with radiographic evidence of pneumonia and was treated with systemic antibiotics. Five days later, the boy's grandfather developed the same symptoms. No hospitalizations were required, nor were they tested for COVID‐19. On March 20, 2020, the boy developed fever, and in a few days, edema and localized pain of the right hand and feet were noted, leading to difficulty walking. Four days later, chilblains‐like lesions appeared. On examination, there were several rounded macules with blurred edges, 5‐20 mm in diameter, on the plantar surface of both feet, as well as the right hand (Figure 3). The child's parents also reported having had cough for the last 20 days. The boy and his mother were tested for COVID‐19 with nasopharyngeal swab and aspirate, and the results were negative. Blood tests showed no abnormalities except for mild thrombocytosis and monocytosis. No treatment or biopsy was performed, and within 3 days, the lesions subsided without sequelae.
FIGURE 3.

Patient 3, diffuse chilblains‐like lesions on the plantar surface of the left foot in a 5‐y‐old boy
5. PATIENT 4
On April 18, 2020, an 11‐year‐old girl from Milan (Lombardy region, Italy) was referred to our department by her pediatrician for a 20‐day history of foot lesions, swelling, and difficulty walking. Skin examination demonstrated erythematous and dusky 5‐15 mm plaques on the lateral margin of the left foot and the dorsal surface of the left second, third, and fifth toes (Figure 4). The patient also reported intermittent fever and localized pain during the previous ten days. The girl and her mother were tested for COVID‐19 with nasopharyngeal swab and aspirate; the results were negative. Blood tests showed no abnormalities. A skin biopsy was performed. Histology revealed dense lymphocytic perivascular cuffing and periadnexal infiltration. Signs of vasculitis were evident in small‐ to medium‐sized vessels with endothelial cell swelling and red blood cell extravasation. Fibrin thrombus was evident in superficial capillary vessels (Figure 5). No treatment was initated.
FIGURE 4.

Patient 4, chilblains‐like lesion on the lateral surface of the left foot in an 11‐y‐old girl
FIGURE 5.
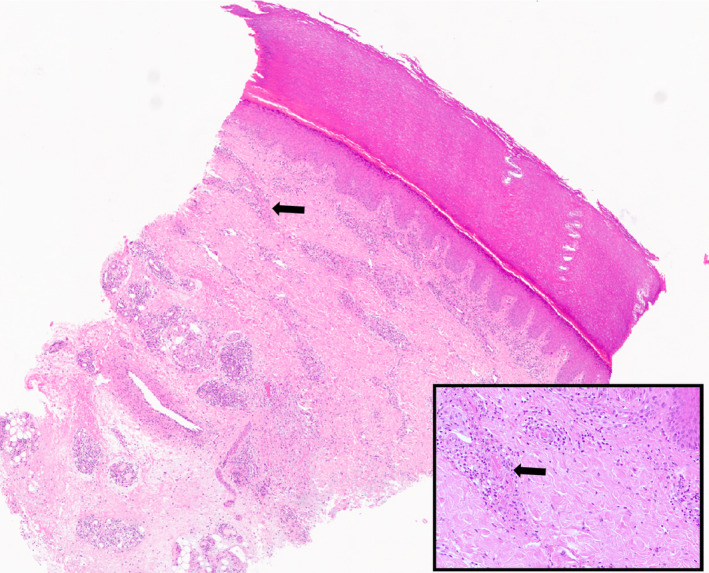
Patient 4, punch biopsy from the lateral surface of the left foot of Patient 4. Dense lymphocytic perivascular and periadnexal infiltrates extending to the subcutis. Inset: higher magnification of a small thrombus in a capillary vessel in the upper part of the dermis (arrow)
6. DISCUSSION
Herein, we describe chilblains‐like lesions in four children to further explore its correlation with COVID‐19. In our patients, the cutaneous manifestation appeared several days after systemic symptoms and all tests for active COVID‐19 infection were negative at the time of first clinical evaluation. However, the accuracy and predictive values of COVID‐19 testing have not been systematically evaluated. Serologic antibody testing might be able to identify a previous COVID‐19 infection linked to the cutaneous manifestations but reliable testing was not available at the time these cases were evaluated. 6
The clinical finding of acro‐ischemia may not be an unusual manifestation of COVID‐19 infection 4 ; however very little has been published describing the histological features of this finding. 7 It is known that chilblains‐like lesions can occur secondarily in other circumstances (e.g. infectious diseases, interferon disorders, adverse drug reaction). For example, the parvovirus B19 atypical acrosyndrome is an eruption that differs from the classic "gloves and socks syndrome" because of the presence of plantar painful erythrocyanosis. 8 In our cases, infection with several common viruses was ruled out. The nature of the phenomenon in relation to COVID‐19 infection is still under evaluation. Autopsy findings from COVID‐19 infected patients showed IL‐6 is significantly elevated and associated with adverse clinical outcomes, suggesting a relationship between degree of inflammation and severity of disease.
As reported by Zhang et al., 4 COVID‐19 could be responsible for coagulation disorders, increasing the D‐dimer and fibrinogen degradation products, leading to acro‐ischemia. The finding of an elevated D‐dimer in one of our patients, along with the clinical features suggestive of a vaso‐occlusive phenomenon, supports laboratory evaluation for coagulation defects in asymptomatic or mildly symptomatic children with chilblains‐like findings. In small autopsy series, thrombosis associated with COVID‐19 was described mainly in the lungs and kidneys. 9 , 10 , 11
Given the fact that the sensitivity and specificity of both nasopharyngeal swabs and antibody tests for COVID‐19 (when available) are not 100% reliable, the question of the origin of these strange chilblain‐like lesions is still elusive. 12 Until our observation can be further validated by larger studies, clinicians should be alert to the presentation of chilblains‐like findings in pauci‐symptomatic pediatric patients as a possible sign of COVID‐19 infection.
Colonna C, Monzani NA, Rocchi A, Gianotti R, Boggio F, Gelmetti C. Chilblain‐like lesions in children following suspected COVID‐19 infection. Pediatr Dermatol. 2020;37:437–440. 10.1111/pde.14210
REFERENCES
- 1. Huang C, Wang Y, Li X, et al. B Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497‐506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Joob B, Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for Dengue. J Am Acad Dermatol. 2020;82(5):e177. 10.1016/j.jaad.2020.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol. 2020. 10.1111/jdv.16387 [DOI] [PubMed] [Google Scholar]
- 4. Zhang Y, Cao W, Xiao M, et al. Clinical and coagulation characteristics of 7 patients with critical COVID‐2019 pneumonia and acro‐ischemia. Zhonghua Xue Ye Xue Za Zhi. 2020;41:E006. [DOI] [PubMed] [Google Scholar]
- 5. Mazzotta F, Troccoli T, Bonifazi E. Acute acro‐ischemia in the child at the time of covid‐19. Eur J Pediatr Dermatol. 2020;121(2):172‐175. [Google Scholar]
- 6. Xie X, Zhong Z, Zhao W et al. Chest CT for typical 2019‐nCoV pneumonia: relationship to negative RT‐PCR testing. Radiology. 2020; 200343. 10.1148/radiol.2020200343. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Magro C, Mulvey JJ, Berlin D, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID‐19 infection: a report of five cases. Transl Res. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Penouil MH, Estève E, Millotte B, et al. Parvovirus B19 atypical acrosyndrome. Ann Dermatol Venereol. 1997;124(3):254‐256. [PubMed] [Google Scholar]
- 9. Yao XH, Li TY, He ZC, et al. A pathological report of three COVID‐19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi. 2020;49:E009. [DOI] [PubMed] [Google Scholar]
- 10. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID‐19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wang HJ, Du SH, Yue X, Chen CX. Review and prospect of pathological features of corona virus disease. Fa Yi Xue Za Zhi. 2020;36(1):16‐20. [DOI] [PubMed] [Google Scholar]
- 12. Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507‐513. [DOI] [PMC free article] [PubMed] [Google Scholar]


