Abstract
The COVID‐19 epidemic has resulted in many hospitals and practices to cancel in‐person outpatient clinic visits, where head and neck patients receive their critical longitudinal care. Out of necessity, most practices have been encouraged to use telemedicine as a method to maintain a continuum of care with their patients. As a result, the prevalence of telemedicine has grown rapidly during this pandemic, without allowing the physicians and patients to be adequately educated on how best to utilize the services. There is a steep learning curve as we have learned, and our goal is to provide guidelines for both patients and physicians, as well as a valuable patient handout in preparation for their visit.
Keywords: cancer, COVID‐19, patient care, telehealth, telemedicine
1. INTRODUCTION
The 2019 novel coronavirus disease (COVID‐19) was initially identified in December 2019 in Wuhan, China. Following its spread across the globe within a matter of months, the World Health Organization classified COVID‐19 as a pandemic. 1 Its rapid transmission and high hospitalization rate have forced health professionals to drastically alter their practices in order to slow its proliferation. The rapid influx of COVID‐19 related admissions in hospitals around the United States has led to a widespread shortage of crucial health care resources, particularly personal protective equipment (PPE), ventilators, and free ICU beds. Surgical procedures further deplete such resources in a time of acutely high need. Additionally, evidence has shown that health care workers may be particularly susceptible to infection from the causative pathogen, SARS‐CoV‐2, with roughly 20% of exposed professionals becoming infected in Italy. 2 Following these developments, the Centers for Disease Control and Prevention (CDC) recommended that all inpatient facilities postpone or cancel any elective surgeries. 3 In the ensuing weeks, the American College of Surgeons and the American Academy of Otolaryngology‐Head and Neck Surgery followed suit with this recommendation.4, 5
Furthermore, many hospitals and practices have opted to cancel in‐person outpatient clinic visits, where patients oftentimes receive critical longitudinal care. Like other surgeons, otolaryngologists, and specifically head and neck surgical oncologists, have been deeply affected by these drastic measures. It is evident, however, that physicians must find ways to continue to monitor such patients’ conditions or treat them in some aspect. The popularity and prevalence of telemedicine have grown rapidly during this pandemic as many physicians have sought ways to maintain a continuum of care with their patients. 6 Such initiatives have previously been shown to decrease costs, decrease visit time, and lead to high patient satisfaction in surgical fields.7, 8
Within otolaryngology specifically, certain telehealth assessments have been shown to allow for quicker examinations without compromising the communication of crucial information from the patient to the physician, or vice versa. 9 However, the rapid implementation of telehealth has been a relatively new phenomenon during the COVID‐19 pandemic, meaning that physicians oftentimes have to learn how to optimize their virtual visits to maximize their efficiency and effectiveness. In otolaryngology, telemedicine has not been routinely used to evaluate patients, despite estimates that 62% of otolaryngology patients would be amenable to virtual appointments. 10 Thus, it may be difficult for physicians to anticipate barriers to their care during a telehealth visit. Based on the authors’ experience, there exists a steep learning curve following the onset of such visits due to a variety of factors on both the patient's and physician's side.
To the best of our knowledge, there are no set guidelines or best practices for patients or head and neck cancer physicians conducting virtual visits. Drawing upon our experience, we aim to compile a set of guidelines for physicians and patients alike to navigate telehealth visits during the era of COVID‐19. We also created a handout that can be distributed to patients prior to the visit, such that patients can familiarize themselves with general expectations and key examination steps that they may be asked to perform during the visit.
2. GENERAL GUIDELINES
2.1. Physicians
Given the constraints of remote visits, physicians are inherently limited in the amount of information that can be conveyed to them through video or audio. Obtaining patient history and understanding subjective patient complaints should remain ascertainable following a comprehensive and detailed conversation between the two parties. Physical exam findings, however, are understandably more difficult to obtain in a remote visit. Physicians may often have patients perform rudimentary aspects of a physician exam on themselves and describe their observations in detail to the physician. Given the lack of expertise among the majority of patients, physicians should promptly convey their expectations for the visit and possible tasks they might have patients perform. Distribution of the graphic handouts prior to the virtual visit can allow patients to adequately prepare for the visits. This ensures that the visit is as fruitful as possible and that time is not spent having the physician explain a task without context during a visit. Recommendations and expectations for patients are further discussed below (Figure 1).
FIGURE 1.
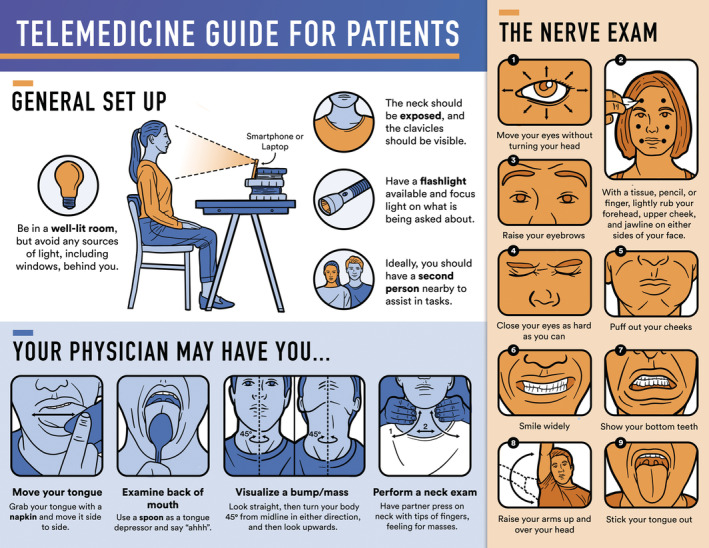
Patient handout in preparation for telemedicine visit
Professionalism should be maintained throughout the virtual visits. Physicians should use a high‐resolution camera, such as one from a laptop or an external webcam, and dress professionally. Furthermore, physicians should ensure their face is clearly seen in their video and that there is ample lighting. It may be advisable for physicians to have the materials recommended for patients easily available, such as a flashlight and napkins, in order to demonstrate aspects of the exam on themselves if patients are having difficulty. Having access to a high‐quality Wi‐Fi or network signal is also critical.
2.2. Patients
It is imperative for physicians to obtain a clear and unobscured view of their patient's head and neck during a virtual examination. To help ensure this, physicians can communicate certain baseline expectations to patients using the handout in Figure 1 and have the nursing/administrative staff discuss this with the patient prior to the visit.
General setup
Patient positioning: Ideally, patients should be sitting on a dining room chair or equivalent. This allows them to sit erect and permits a second person to stand behind the patient to perform a neck exam. Patients should also choose a room in the house that has ample lighting and avoid having light sources, including windows, positioned behind their back, as this can cause underexposure of the subject and a silhouette effect.
Equipment: If patients have access to a laptop or a computer with a large screen, they should be encouraged to use that over their cellphone. Additionally, a high‐resolution camera and Wi‐Fi signal is important.
Camera positioning: The camera positioned at eye‐level helps provide physicians with a clear, properly angled view of the patient's face and neck. Ideally, the camera, whether it is on the laptop or phone, should be propped up, such that patients have both hands free and unoccupied in order to perform basic physical exam tasks.
Second person present during the visit: If possible, patients should be encouraged to have a family member or friend present during the visit, so that they can assist with certain tasks if needed. This is preferable for many aspects of the virtual physical exam; for example, it allows patients to maintain an optimal camera angle for the physician while a third person carries out the basic examination.
Patient clothing: Patients should avoid clothing that obscures or covers the neck in order to reduce obstruction of the physician's view.
Extra light source: Patients should have a flashlight or another light source to enhance visualization during the physical exam. In such situations, light should be focused as much as possible on the target of interest, while minimizing illumination of surrounding structures. As stated previously, having an additional person aid in this task can help maximize the physician's view through the camera and reduce multitasking required by the patient.
- Physical exam
- Vital signs: If able, patients should be asked to take their blood pressure, temperature and weight before the visit with self‐purchased BP cuffs, thermometer, and weighing scale.
- Exam: Since physicians cannot perform the physical exams, they will need to rely on the patient's own ability to perform their own physical exam. These are highlighted in Figure 1.
- Subsite exam: highlighted in section below.
- Neck exam: If a second person is present during the visit and able to do the exam, they should be encouraged to participate. Ideally, they should be asked to stand behind the patient to perform the exam. As highlighted in Figure 1, it is ideal if they palpate the patient's neck in a directional manner (from superior to inferior, then medial to lateral).
- Cranial nerve exam: most frequently tested cranial nerves are highlighted in Figure 1
3. SUBSITE‐SPECIFIC GUIDELINES
These subsite‐specific guidelines and tips are provided as a guide to optimize the telemedicine visit. It is by no means intended to serve as an all‐inclusive list of questions and physical examination maneuvers for each subsite. Rather, the purpose is to provide some structure and thoughts on how to best navigate surveillance and examination of these subsites.
3.1. Oral cavity
Subjective: In addition to the routine questions, physicians can ask patients if they note the following symptoms: new sore in the mouth, unresolving pain in the mouth, trismus, dysphagia, odynophagia, ear pain, difficulty with tongue mobility, tongue numbness, pain or difficulty with mastication, loosening of teeth, any new lumps, weight loss, and constant bad breath.
Physical exam: Patient history of these symptoms are of particular importance during the virtual oral cavity examination. Upon first glance, a self‐performed, abbreviated oral cavity physical exam may seem straightforward due to the ease of access to the oral cavity. However, this exam may be quite challenging for patients based on their level of expertise in being able to properly position their camera or external light source (flashlight). As discussed in the general guidelines, the presence of an additional individual to properly angle the light source for the patient can be extremely beneficial and make a critical difference. Additionally, in order to ensure patients do not obstruct the physician's view of the oral cavity subsite, physicians may find it useful to demonstrate optimal examination technique on themselves. For example, this could involve grasping the tip of the tongue with a napkin using the fingertips in order to maximize its view (Figure 1).
3.2. Oropharynx
Subjective: Since the virtual physical examination of the oropharynx is limited, the physician is more reliant on the patient's reported symptoms. Symptoms are similar to those highlighted for the oral cavity examination.
Physical examination: Attempts can be made to have the patients use a spoon as a tongue depressor to evaluate and view the soft palate and tonsils.
3.3. Larynx
Subjective: Once again, due to limitations of a virtual physical examination, physicians must largely rely on patient reports of salient symptoms, including dysphagia, odynophagia, hoarseness or voice changes, ear pain, breathing difficulty, constant sore throat, or new neck mass.
Physical exam: Patients can phonate a few different sounds, and attempts can be made to hear breaks in voice or changes in voice quality. Physicians can have patients feel for laryngeal crepitus to obtain clinical signs of mass in the retrolaryngeal space or hypopharynx. 11 If there are concerns with airway patency, patients can be asked to breath with an open mouth, which could reveal concerns for an obstructive mass or stenosis.
3.4. Salivary glands
Subjective: Symptoms to ascertain from patients include the presence of a new mass or swelling, facial nerve weakness, pain in the region of a salivary gland, numbness in a part of the face, pain with mastication, and trismus.
Physical exam: Attempts can be made to determine subtle changes or asymmetry in the salivary glands. To facilitate this, patients can be asked to first look straight at the camera, then turn their body 45° from the midline in either direction and then look upwards. If there are concerns for changes in skin morphology in the area overlying the lesion, patients can be asked to gently run their fingers over the lesion and to assess for skin mobility. The cranial nerve exam and neck exam are of particular importance for clinical assessment of salivary gland pathology.
4. CONCLUSION
The rapid spread of COVID‐19 across the United States has led to overburdening of the health care system and a cancellation of many in‐person patient visits. As a result, many practices have been turning to telemedicine as an avenue for continued care for patients while minimizing mutual risk of exposure to SARS‐CoV‐2. This approach, while extremely useful, can be challenging for both the physician and patient, particularly as this is a new mode of clinical evaluation for both parties. Head and neck cancer surveillance is often challenging to perform in person, and doing this virtually without being able to educate patients on expectations can make the task even more difficult. In order to mitigate many of these issues, we have provided a set of guidelines for implementation of telehealth visits. We additionally provide an easy‐to‐read handout that can be widely distributed to patients to assist them in preparing for a virtual visit. Our hope is that this can maximize the utility gained from telehealth visits for both the physician and patient in the era of COVID‐19 and beyond.
Prasad A, Brewster R, Newman JG, Rajasekaran K. Optimizing your telemedicine visit during the COVID‐19 pandemic: Practice guidelines for patients with head and neck cancer. Head & Neck. 2020;42:1317–1321. 10.1002/hed.26197
REFERENCES
- 1.WHO Director‐General's opening remarks at the media briefing on COVID‐19‐11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed March 11, 2020.
- 2. Remuzzi A, Remuzzi G. COVID‐19 and Italy: what next? Lancet. 2020;395:1225‐1228. 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Interim guidance for healthcare facilities: preparing for community transmission of COVID‐19 in the United States. https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fhealthcare-facilities%2Fguidance-hcf.html. Accessed February 29, 2020.
- 4.COVID‐19: guidance for triage of non‐emergent surgical procedures. https://www.facs.org/about-acs/covid-19/information-for-surgeons/triage. Accessed March 17, 2020.
- 5.New recommendations regarding urgent and nonurgent patient care. https://www.entnet.org/content/new-recommendations-regarding-urgent-and-nonurgent-patient-care-0. Accessed March 20, 2020.
- 6. Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID‐19. N Engl J Med. 2020. 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 7. Russo JE, McCool RR, Davies L. VA telemedicine: an analysis of cost and time savings. Telemed J E Health. 2016;22:209‐215. 10.1089/tmj.2015.0055. [DOI] [PubMed] [Google Scholar]
- 8. Cain SM, Moore R, Sturm L, et al. Clinical assessment and management of general surgery patients via synchronous telehealth. J Telemed Telecare. 2017;23:371‐375. 10.1177/1357633X16636245. [DOI] [PubMed] [Google Scholar]
- 9. Alemi AS, Seth R, Heaton C, Wang SJ, Knott PD. Comparison of video and in‐person free flap assessment following head and neck free tissue transfer. Otolaryngol Head Neck Surg. 2017;156:1035‐1040. 10.1177/0194599816688620. [DOI] [PubMed] [Google Scholar]
- 10. McCool RR, Davies L. Where does telemedicine fit into otolaryngology? An assessment of telemedicine eligibility among otolaryngology diagnoses. Otolaryngol Head Neck Surg. 2018;158:641‐644. 10.1177/0194599818757724. [DOI] [PubMed] [Google Scholar]
- 11. Hansen SH. Laryngeal crepitus: an aid to diagnosis in non‐fatal strangulation. Med Sci Law. 2001;41:284‐286. 10.1177/002580240104100402. [DOI] [PubMed] [Google Scholar]


