Abstract
Background
COVID‐19 pandemic has led to a global shortage of personal protective equipment (PPE). This study aims to stratify face shield needs when performing head and neck cancer surgery.
Methods
Fifteen patients underwent surgery between March 1, 2020 and April 9, 2020. Operative diagnosis and procedure; droplet count and distribution on face shields were documented.
Results
Forty‐five surgical procedures were performed for neck nodal metastatic carcinoma of unknown origin (n = 3); carcinoma of tonsil (n = 2), tongue (n = 2), nasopharynx (n = 3), maxilla (n = 1), and laryngopharynx (n = 4). Droplet contamination was 57.8%, 59.5%, 8.0%, and 0% for operating, first and second assistant surgeons, and scrub nurse respectively. Droplet count was highest and most widespread during osteotomies. No droplet splash was noted for transoral robotic surgery.
Conclusion
Face shield is not a mandatory adjunctive PPE for all head and neck surgical procedures and health care providers. Judicious use helps to conserve resources during such difficult times.
Keywords: conservation, COVID‐19, face shield, head and neck cancer, PPE
1. INTRODUCTION
SARS‐CoV‐2 virus is the causative agent of the coronavirus disease 2019 (COVID‐19) pandemic. Since its outbreak, health care systems around the world are faced with unprecedented challenges with priorities of care and resources being shifted to combat COVID‐19.
With limited resources during the COVID‐19 pandemic, the major challenges that we head and neck cancer surgeons face are patient selection and timing of treatment, while preventing transmission of virus to health care providers and patients. 1 Majority of patients with head and neck cancer are elderly with multiple comorbidities and poor respiratory reserve from chronic tobacco use, predisposing them to SARS‐CoV‐2 contraction and COVID‐19 related mortality. However, if left untreated, tumors in the upper aerodigestive tract may impair essential functions such as breathing and swallowing, tumors may progress and metastasize, eventually leading to mortality.
SARS‐CoV‐2 is found in high abundance in the upper aerodigestive tract mucosa, particularly the nasopharynx. 2 Patients may be asymptomatic at the time of presentation. 3 There is currently no accurate way of diagnosis—polymerase chain reaction (PCR) testing for nucleic acid sequence homology in nasopharyngeal and throat swabs may be negative early in the course of disease. 4 The virus is known to be transmitted via close contact, droplet and aerosols from aerosol generating procedures (AGP) such as tracheotomy. 5 Hence as head and neck surgeons, we are at great risk of becoming infected when treating patients with head and neck cancer.
Ideally full barrier protection should be advocated when treating unknown, suspected, and confirmed COVID‐19 patients in order to avoid disease transmission to health care providers. Such personal protective equipment (PPE) includes gloves, goggles, face shield, and gowns, as well as items filtering facepiece respirators such as N95 or powered air‐purifying respirator (PAPR) hoods and aprons. 6
However, as the number of confirmed cases increases globally, resources including PPE become scarce. As of April 12, 2020, there are 1 695 096 confirmed cases spanning 215 countries of which Hong Kong accounts for 1005 patients.7, 8 In Queen Mary Hospital, The University of Hong Kong, the Division of Head and Neck Surgery has undergone a 50% reduction in head and neck cancer operations since March 2020 as a result of diminished supplies of PPE in particular N95 respirator and face shields.
In view of global PPE shortage, we look at strategies to optimize PPE availability, which includes minimizing the need for PPE in health care settings and ensuring rational and appropriate use of PPE.
This study aims to stratify face shield needs when performing head and neck cancer surgery with the aim of conserving PPE during the COVID‐19 pandemic.
2. MATERIALS AND METHODS
All patients who underwent surgery for head and neck cancer in the Division of Head and Neck Surgery of the Department of Surgery, The University of Hong Kong at Queen Mary Hospital and Gleneagles Hong Kong Hospital between March 1, 2020 and April 9, 2020 were included.
All patients underwent comprehensive work‐up for tumor staging including clinical and endoscopic examination of the upper aerodigestive tract, and ultrasonography of the neck +/− fine needle aspiration for cytology of suspected neck nodal metastasis with full barrier protection. Magnetic resonance imaging +/− whole‐body positron emission tomography scans was also performed for tumor staging.
Admission to head and neck surgical ward was only allowed (a) on declaring absence of travel history 14 days prior to surgery, (b) absence of close contact with confirmed cases, and (c) tympanic body temperature <37.5°C taken at ward entrance. On admission, routine bloods including white cell count and chest X‐ray were checked. As recommended by Centre for Health Protection in Hong Kong (CHP) and Queen Mary Hospital Infection Control Unit, PCR would only be tested for febrile and symptomatic patients +/− radiological changes on chest X‐ray.
All operations were performed by a consultant surgeon and two assistants who have completed their fellowship in head and neck surgery. Skin incisions and tracheotomies were performed using scalpel knife. Reciprocating and oscillating saws were used for maxillary swing and manubrial resection respectively. Monopolar and bipolar diathermy was used for tissue dissection and hemostasis.
Full barrier protection was adopted by all three surgeons and one scrub nurse. The face shield (A R Medicom Inc (Asia) Ltd.) used was a piece of optically clear, latex free plastic film measuring 32 cm in length and 22 cm in width with foam forehead cushion and elastic strap. It covered a full face length from forehead to neck, with outer edges of the face shield reaching bilateral ears. It had antifog and antiglare properties with no hearing restrictions.
The face shield of each surgeon and scrub nurse was removed after each procedure. Each face shield was put against a white background with 12 grids measuring 7 cm × 7 cm each to facilitate counting at maximal magnification (Figure 1). The number and size of droplets splashed was counted for each face shield using the surgical microscope Leica M720 0H5 (Leica Microsystems GmbH, Germany; Figure 2). Droplet distribution per face shield was plot on a separate sheet with the same grid as that used in Figure 1 (Figure 3). Each of the 12 grids was labeled 1 to 12 (Figure 4). Counting and plotting of droplets splashed were performed by a surgeon who did not participate in the operation. The face shields were discarded once counting was complete.
FIGURE 1.

Face shield placed on white background with grid prior to droplet count with surgical microscope [Color figure can be viewed at http://wileyonlinelibrary.com]
FIGURE 2.
Two bloodstained droplets viewed under surgical microscope at 7.8× magnification [Color figure can be viewed at http://wileyonlinelibrary.com]
FIGURE 3.
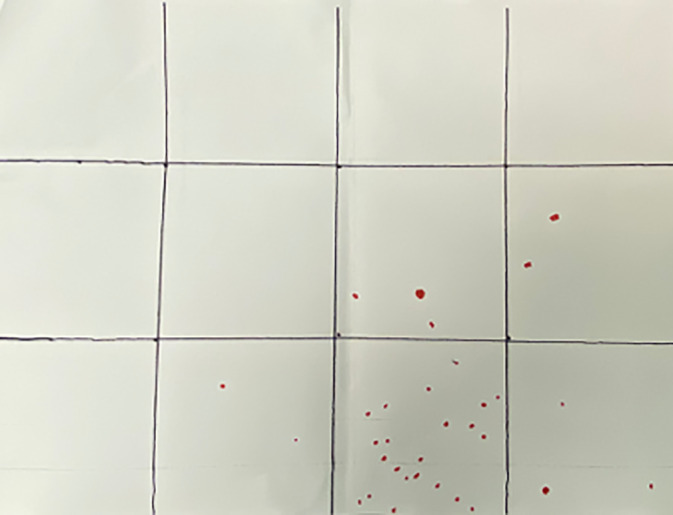
Plots of droplet splash and distribution with red marker based on face shield of operating surgeon during manubrial resection [Color figure can be viewed at http://wileyonlinelibrary.com]
FIGURE 4.
Labeling of grids from 1 to 12
Operative diagnosis and procedure; size, average number, and distribution of droplets on face shield for each party were documented.
3. RESULTS
Fifteen patients with no clinical evidence of COVID‐19 underwent operations for head and neck cancer: 3 patients with metastatic squamous cell carcinoma of unknown primary underwent examination under anesthesia, transoral robotic (TORS) tonsillectomy and tongue base mucosectomy and modified radical neck dissection; 2 patients underwent radical tonsillectomy, modified radical neck dissection, free anterolateral thigh flap reconstruction and tracheostomy for tonsillar carcinoma; 2 patients with carcinoma of the tongue underwent glossectomy and selective neck dissection followed by free anterolateral thigh flap reconstruction and tracheostomy; 1 patient underwent total laryngectomy for recurrent carcinoma of larynx; 3 patients with recurrent pharyngoesophageal carcinoma underwent total laryngectomy (n = 3), circumferential pharyngectomy (n = 3) and cervico‐esophagectomy after manubrial resection (n = 1), followed by reconstruction with free jejunal flap (n = 3); 3 patients with recurrent nasopharyngeal carcinoma underwent tracheostomy followed by maxillary swing nasopharyngectomy, 1 patient required selective neck dissection and free vastus lateralis flap coverage of exposed internal carotid artery; and 1 patient with carcinoma of maxilla underwent tracheostomy, total maxillectomy, selective neck dissection and free anterolateral thigh flap reconstruction (Table 1).
TABLE 1.
Operating procedures, droplet count and distribution by zone for operating surgeon, first and second assistant surgeon, and scrub nurse
| Operating procedure | Operating surgeon average number of droplets (zones affected) | First assistant average number of droplets (zones affected) | Second assistant average number of droplets (zones affected) | Scrub nurse average number of droplets (zones affected) |
|---|---|---|---|---|
| TORS tonsillectomy + tongue base mucosectomy (n = 3) | 0.0 | 0.0 | NA | 0.0 |
| Radical tonsillectomy (n = 2) | 2.0 (6) | 5.0 (9,10,11) | 0.0 | 0.0 |
| Glossectomy (n = 2) | 2.5 (10,11) | 6.0 (6,7,10,11) | 0.0 | 0.0 |
| Nasopharyngectomy (n = 3) | 2.0 (10,11) | 0.7 (2,11) | 0.0 | 0.0 |
| PLCE (n = 4) | 5.0 (6,10) | 7.0 (6,7,8,10,11) | 0.0 | 0.0 |
| Tracheostomy (n = 8) | 0.6 (10,11) | NA | NA | 0.0 |
| Maxillectomy a (n = 4) | 40.0 (2,3,4,6,7,8,9,10,11,12) | 21.3 (2,3,4,6,7,8,9,10,11,12) | 1.0 (2,3,6) | 0.0 |
| Manubrial resection (n = 1) | 32.0 (7,8,10,11,12) | 1.0 (6,7,8,10,11,12) | 0.0 | 0.0 |
| Neck dissection (n = 9) | 1.2 (10,11) | 2.8 (6,10,11) | 0.1 (6) | 0.0 |
| Free anterolateral thigh flap (n = 5) | 1.2 (7,10) | 0.4 (10,11) | NA | 0.0 |
| Free vastus lateralis flap (n = 1) | 2.0 (7,10) | 0.0 | NA | 0.0 |
| Free jejunal flap (n = 3) | 1.0 (10) | 0.0 (11) | NA | 0.0 |
Abbreviations: PLCE, pharyngo‐laryngo‐cervico‐esophagectomy; TORS, transoral robotic surgery.
Maxillectomy includes maxillary swing operations (n = 3).
There were a total of 45 procedures of which 26 involved mucosa along the upper aerodigestive tract. There were 12 procedures which involved manipulation of the airway including temporary tracheostomy (n = 8) and laryngectomy (n = 4). Operating surgeon and scrub nurse were involved in all surgical procedures (n = 45). First assistant was involved in all but tracheostomy operations (n = 37). Second assistant was not involved in TORS, tracheostomy and free flap harvest procedures (n = 25). Overall droplet size ranged from 0.3 mm to 3.0 mm. Percentage of procedures with droplet contamination was 57.8% for the operating surgeon (n = 26), 59.5% for the first assistant (n = 22), and 8.0% for the second assistant (n = 2). No droplets were noted on all face shields of the scrub nurse (n = 45).
Average droplet count was highest for procedures involving osteotomies such as maxillectomy (n = 1), maxillary swing (n = 3) and manubrial resection (n = 1). Droplet spread was more widespread (zones 2‐12) for maxillectomy procedures (n = 4), involving face shields of the operating, first and second assistant surgeons.
Nonosteotomy surgical procedures involving mucosa of the nasopharynx (n = 3), oropharynx (n = 5), oral cavity (n = 2), laryngo‐pharyngeal apparatus (n = 4), and trachea (n = 8) yielded minimal droplet count on face shields of the operating surgeon and first assistant, affecting zones 6 to 11 which were over the lower half of the face. There was one droplet splash at zone 2 of the first assistant during nasopharyngectomy, corresponding to upper half of the face. No droplet splash was noted on the second assistant's face shield. No droplet splash was documented on face shields of the operating surgeon and first assistant for TORS.
Average droplet count from nonmucosal, nonosteotomy related surgical procedures such as neck dissection (n = 9) and free flap harvest (n = 9) was minimal on both the operating surgeon's and first assistant's face shields, mainly affecting zones 6, 7, 10, and 11 which were concentrated on the lower half of the face. One drop was noted in zone 6 of the second assistant's face shield during modified radical neck dissection.
4. DISUCSSION
The current global stockpile of PPE is insufficient due to the rapidly increasing number of infected patients worldwide. In view of global PPE shortage, strategies have been formulated to optimize PPE availability include minimizing the need for PPE in health care settings, and ensuring rational and appropriate use of PPE. 9
In Queen Mary Hospital, attempts at minimizing PPE need include reducing the volume of head and neck patients undergoing outpatient clinic and endoscopy service by 60%, and operations by 50% and the number of health care providers within endoscopy suites and operating theater.
Based on current evidence, SARS‐CoV‐2 is transmitted between people through close contact and droplets. Airborne transmission may occur during AGP and support treatments including tracheal intubation, noninvasive ventilation, tracheotomy, cardiopulmonary resuscitation, manual ventilation before intubation, and bronchoscopy. Despite concerns of aerosolization of blood using energy device, manipulation of upper aerodigestive tract mucosa and resection of tumors in the upper aerodigestive tract are not classified as AGP.9, 10, 11, 12 According to World Health Organization (WHO), droplet and contact precautions with the use of medical masks, eye protection, cap, gown, and gloves are sufficient for regular care of COVID‐19 patients. Respirators such as N95 or PAPR are advocated for AGP.9, 13
There is currently no universal standard for face and/or eye protection from biohazards. Face shield is usually in the form of an optically clear plastic film, which covers the forehead to neck and both sides of the face up to the ears. Due to the lack of a good facial seal peripherally, face shields are usually used as an adjunctive PPE, which acts to provide additional physical barrier against splashes, sprays, and spatter of body fluids. 14 However, the use of face shield hinders the use of a headlight when performing head and neck surgery. Prolonged use can give rise to fogging, carbon dioxide retention especially when combined with respirator, and impaired communication.
Centre for Disease Control and Prevention (CDC) Standard Precautions guidelines for prevention of transmission of infectious agents includes the use of face shields (with a medical/surgical face mask) when sprays, splashes, or splatter are anticipated. 15 The effectiveness of face shields in preventing the transmission of viral respiratory diseases is unknown. 16 With the use of goggles and appropriate respiratory protection device, we reevaluate the need for face shield in performing head and neck cancer surgical procedures.
In an attempt to conserve face shield and other PPE consumption, we minimized the number of health care providers during operation: all tracheostomy (n = 8) was performed by the operating surgeon alone. Furthermore, a second assistant was not involved in TORS and free flap harvest procedures. Only the operating surgeon and scrub nurse was involved in all 45 surgical procedures.
From our study, the percentage of procedures with droplet contamination was 57.8% for the operating surgeon, 59.5% for the first assistant, and 8.0% for the second assistant. No droplets were noted on all face shields of the scrub nurse. In view of 0% contamination rate, face shield is not necessary for the scrub nurse for all non‐AGP.
Droplet count was highest and most widespread with procedures involving osteotomies such as maxillectomy, maxillary swing, and manubrial resection. Other than blood, irrigation fluid also contributed to the number of droplets. Vibrations of saw blade caused droplets to be dispersed over a large area during osteotomy, as reflected by the distribution on the surgeon and two assistants' face shields (Figure 3; Table 1). This can be minimized by controlled irrigation and vigilant suction to minimize the amount of irrigation fluid and blood accumulating around the saw blade. Operation by an experienced surgeon would also help to reduce blood loss and shorten procedure time. Face shield should be provided for the operation, first and second assistant surgeons during osteotomy‐related procedures.
Nonosteotomy surgical procedures involving mucosa of the upper aerodigestive tract yielded minimal droplet count on face shields of the operating surgeon and first assistant, affecting zones 6 to 11, which were centered over the lower half of the face. There was one droplet splash at zone 2 of the first assistant during nasopharyngectomy, corresponding to the first assistant's eye level. No droplet splash was noted on the second assistant's face shield. Abiding by CDC, WHO, and CHP guidelines, face shield should be used by all surgeon(s) for AGP including tracheostomy and laryngectomy. For non‐AGP, face shield for second assistant may not be warranted. Given the low droplet count on face shields of the operating surgeon and first assistant, one could argue against the need for face shield as an adjunctive PPE to goggles and adequate respiratory device for the aforementioned procedures, which are non‐aerosol generation.
For TORS, docking was performed by the operating surgeon prior to commencement of surgery. In order to prevent droplet splash the following steps have been taken: (a) ensure that the cuff of the endotracheal tube was inflated with no evidence of air leak and (b) Fr 16 Nelaton suction catheter was placed through the remaining nostril down to the level of the oropharynx for suctioning of saliva prior to docking and also of blood and diathermy smoke and aerosols during the operation. There were no droplets noted on the operating surgeon's face shield during docking and none noted on the first assistant's face shield after the operation. Hence, face shield is not necessary for the operating and assistant surgeons when performing TORS.
Average droplet count from nonmucosal, nonosteotomy‐related surgical procedures such as neck dissection and free flap harvest was minimal on both the operating surgeon's and first assistant's face shields, mainly affecting the lower half of the face. One drop was noted in the lower half of the second assistant's face shield during modified radical neck dissection. Given the low droplet count and low risk of aerosol generation of such procedures, one could argue against the routine use of a face shield as an adjunctive PPE for all surgeons when resources are low during the COVID‐19 pandemic.
Given proper eye protection and adequate respiratory device, results from our preliminary study suggested that face shield, as an adjunctive PPE was not mandatory for all head and neck surgical procedures. The following recommendations can be made when performing head and neck cancer surgery in an attempt to conserve PPE during the COVID‐19 pandemic: (a) All operations are to be performed by an experienced surgeon assisted by specialists in the field of head and neck surgery in order to minimize operation time and droplet contamination. (b) Number of surgeons should be kept at a minimum for all procedures not limiting to AGP. (c) Face shield is advocated for operating and assistant surgeons for procedures involving osteotomies. (d) Conforming to CDC, WHO, and CHP guidelines, face shield should be worn by surgeon(s) performing AGP in unknown, suspected, and confirmed cases. (e) For non‐AGP involving mucosa of the upper aerodigestive tract, face shield can be provided to the operating and first assistant surgeon if resources allow. (f) Routine use of a face shield as adjunctive PPE is not necessary for all parties when performing TORS and all non‐AGP, nonmucosal, and nonosteotomy‐related procedures. (g) Scrub nurse could be spared of using a face shield for all non‐AGP. (h) If resources allow, all patients to be operated on can be quarantined in hospital 14 days prior to surgery, followed by two sets of PCR tests performed 24 hours apart. This would further ensure that patients are COVID‐19 free prior to operation whereby we can revert to standard droplet precautions. Larger scale studies with more patients, procedures, and operating surgeons is warranted to justify such recommendations. Other means to conserve PPE for instance the role and efficacy of N95 respiratory vs medical masks in preventing viral transmission is beyond the scope of this study.
5. CONCLUSION
During the COVID‐19 pandemic, it is our collective responsibility to conserve PPE when treating patients with head and neck cancer while preventing viral transmission to health care providers. Reduction in patient volume, limiting the number of health care providers, and judicious use of PPE are ways to minimize wastage. Practices and recommendations made in this document are intended to support safe clinical practice and efficient use of resources during this challenging time.
6. CONFLICT OF INTEREST
The authors declared no potential conflict of interest.
Chow VLY, Chan JYW, Ho VWY, et al. Conservation of personal protective equipment for head and neck cancer surgery during COVID‐19 pandemic. Head & Neck. 2020;42:1187–1193. 10.1002/hed.26215
REFERENCES
- 1. Vukkadala N, Qian ZJ, Holsinger FC, Patel ZM, Rosenthal E. COVID‐19 and the otolaryngologist ‐ preliminary evidence‐based review. Laryngoscope. 2020;1‐7. 10.1002/lary.28672. [DOI] [PubMed] [Google Scholar]
- 2. Zou L, Ruan F, Huang M, et al. SARS‐CoV‐2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177‐1179. 10.1056/NEJMc2001737. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lai C‐C, Liu YH, Wang C‐Y, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARSCoV‐2): facts and myths. J Microbiol Immunol Infect. 2020;2:1‐36. 10.1016/j.jmii.2020.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ai T, Yang Z, Hou H, et al. Correlation of chest CT and RT‐PCR testing in coronavirus disease 2019 (COVID‐19) in China: a report of 1014 cases. Radiology. 2020;200642 10.1148/radiol.2020200642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. US Centers for Disease Control and Prevention . Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease (COVID‐19) in healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html
- 6. Bann DV, Patel VA, Saadi R, et al. Impact of coronavirus (COVID‐19) on otolaryngologic surgery: a brief commentary. Head Neck. 2020;1‐8. 10.1002/hed.26162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. World Health Organization (WHO) . Novel coronavirus (COVID‐19) situation dashboard. https://who.sprinklr.com
- 8. Centre for Health Protection . Latest situation of coronavirus disease (COVID‐19) in Hong Kong. https://chp-dashboard.geodata.gov.hk/covid-19/en.html
- 9. World Health Organization (WHO) . Rational use of personal protective equipment for coronavirus disease (COVID‐19) and considerations during severe shortages. Interim guidance 2020. https://apps.who.int/iris/bitstream/handle/10665/331695/WHO-2019-nCov-IPC_PPE_use-2020.3-eng.pdf
- 10. Givi B, Schiff BA, Chinn SB, et al. Safety recommendations for evaluation and surgery of the head and neck during the COVID‐19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020. 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 11. Seto WH. Airborne transmission and precautions: facts and myths. J Hosp Infect. 2015;89(4):225‐228. 10.1016/j.jhin.2014.11.005. Epub 2014 Dec 13 Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tran K, Cimon K, Severn M, Pessoa‐Silva CL, Conly J. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012;7(4):e35797 10.1371/journal.pone.0035797. Epub 2012 Apr 26 Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wei WI, Tuen HH, Ng RW, Lam LK. Safe tracheostomy for patients with severe acute respiratory syndrome. Laryngoscope. 2003;113(10):1777‐1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Roberge RJ. Face shields for infection control: a review. J Occup Environ Hyg. 2016;13(4):235‐242. 10.1080/15459624.2015.1095302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention (CDC) . Healthcare Infection Control Practices Advisory Committee (HICPAC). Part III. Precautions to prevent transmission of infectious agents. http://ww.cdc.gov/hicpac/2007IP/2007ip_part3.html
- 16. Institute of Medicine (IOM) Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases . Personal Protective Equipment for Healthcare Workers: Update 2010. Washington, DC: National Academics Press; 2010:10. [PubMed] [Google Scholar]


