Dear Editor,
Coronavirus disease 2019 (COVID‐19) has become a pandemic condition, yet little is known about its dermatologic manifestations. 1 , 2 We report here on peculiar (perniosis‐like) skin lesions, unreported in the previous years, observed in young outpatients visited in our dermatologic unit in the last 4 weeks of COVID‐19 pandemic (March–April 2020). Similar cases were referred to us in the same period by paediatricians and dermatologists from Italy and European countries.
We directly observed 14 cases including 11 children (average age 14.4 years, range 13–18) and three young adults (average age 29 years, range 23–39). In this series, three couples were siblings and the ratio female–male was 8 : 6. The cutaneous manifestations consisted of an acral eruption of erythemato‐violaceous papules and macules, with possible bullous evolution, or digital swelling (Fig. 1a–c). Lesions were localized on the feet in eight cases, on the hands in four cases and on both sites in 2. Two children developed erythemato‐papular targetoid lesions on the hands and elbows after few days (Fig. 1c,d). No systemic symptoms were reported, except mild itch in three cases. In three cases, cough and fever preceded the onset of the lesions 3 weeks before. Lesions resolved after 2–4 weeks without treatment. No association with cold exposure, comorbidities or drug intake was recorded. No familial history of COVID‐19‐related symptoms was elicited.
Figure 1.

Clinical images. (a) Violaceous papules and digital swelling on the feet of a 14‐year‐old girl. A small overlying blister is visible on the big toe. (b) Purple macules on the right foot of a 18‐year‐old girl. (c) Erythematous macules on the right hand of a 14‐year‐old girl. Targetoid lesions are present. (d) Targetoid lesions on the elbows of a 11‐year‐old boy.
Routine laboratory findings were normal, including complete blood count, C‐reactive protein, lactic dehydrogenase and D‐dimer; serology ruled out Epstein–Barr virus, cytomegalovirus, Coxsackie and parvovirus B19 infection. Skin biopsies were performed from lesions on the fingers (n = 2) and from targetoid lesions on the elbows (n = 2). Histology of the acral lesions showed a diffuse dense lymphoid infiltrate of the superficial and deep dermis, as well as hypodermis, with a prevalent perivascular pattern, and signs of endothelial activation (Fig. 2). Histology of the targetoid lesions of the elbows showed a mild superficial perivascular dermatitis. Both nasopharyngeal (three patients) and rectal swabs (two patients) for COVID‐19 yielded negative results. Rectal swabs were performed considering that gastrointestinal tract involvement induces a prolonged virus RNA shedding in feces. 3 , 4 Nevertheless, in the hypothesis that these skin lesions were linked to COVID‐19 infection, we checked accurately for acral perniotic signs 107 COVID‐19‐positive patients (average age 72.2 years, 58 males, 49 females) hospitalized in our hospital for acute respiratory illness. We found only two patients with acrocyanosis due to respiratory failure and one patient with left foot thrombosis. None showed perniotic lesions.
Figure 2.
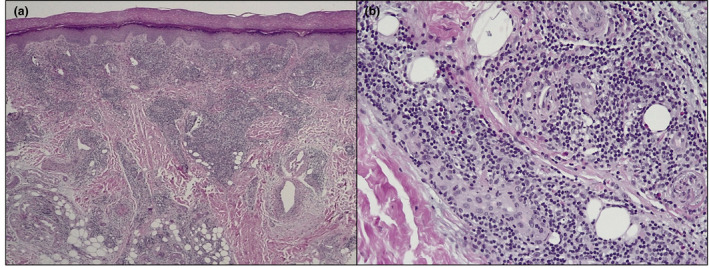
Histologic findings. (a) Diffuse perivascular involvement of the dermis and hypodermis by a dense lymphoid infiltrate, with saving of the epidermis (H&E, 2.5×). (b) Thickening of the vessel wall and activation of the endothelium with nuclear enlargement (H&E, 20×).
We suspect that these cutaneous manifestations could be COVID‐19 related. The temporal relationship with the COVID‐19 pandemia, the rapid outbreak and clustering of unusual skin lesions, the occurrence of familial cases in a situation of home restriction and the multiple reporting of similar cases from other affected areas in parallel with pandemic diffusion strongly support this hypothesis. Young age, swab negativity and the absence of other symptoms appear to be common features of these subjects. The swab negativity could be explained with the disappearance of detectable viral presence after a brief asymptomatic course: according to this hypothesis, the observed skin lesions would represent late manifestations of the COVID‐19 infection in young healthy subjects, possibly due to an immunologic response targeting the cutaneous vessels. The absence of similar signs in acute COVID‐19‐positive patients of older age would corroborate this assumption. Thus, children could be facilitators of viral transmission in the early stage, before skin involvement. 5 Only serology, showing antibody response to COVID‐19 virus, could validate this hypothesis, and we are waiting for such an answer from reliable serological tests.
Acknowledgement
The patients in this manuscript have given written informed consent to publication of their case details.
References
- 1. Ng OT, Marimuthu K, Chia PY et al. SARS‐CoV‐2 Infection among travelers returning from Wuhan, China. N Engl J Med 2020; 382: 1476–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Recalcati S. Cutaneous manifestations in COVID‐19: a first perspective. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16387. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 3. Cai J, Xu J, Lin D et al. A Case Series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis 2020. 10.1093/cid/ciaa198. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Abdelmaksoud A, Kroumpouzos G, Jafferany M, Lotti T, Sadoughifar R, Goldust M. COVID‐19 in the pediatric population. Dermatol Ther 2020: e13339. 10.1111/dth.13339. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5. Kelvin AA, Halperin S. COVID‐19 in children: the link in the transmission chain. Lancet Infect Dis 2020; 1473–3099. 10.1016/S1473-3099(20)30236-X. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]


