The COVID‐19 epidemic necessitates the application of strict isolation strategies to curb virus spreading. Isolation of individuals in combination with fear of contagion, quarantine, and stigma, as well as with potential (mis) information overload (“infodemic”), 1 however, causes chronic stress and is associated with a burden on mental health, posing risk factors for anxiety and depression. It is well understood that chronic stress is a major modulator of immunity 2 and thus directly influences probability of infection. In addition, chronic stress induces structural and functional consequences on the brain resulting in altered social behaviors and limiting in turn individuals’ capacities to cope with the stressful conditions 3 during the epidemic. The circular interaction of stressful COVID‐19‐related conditions with chronic stress triggered impairment of coping strategies, and immune system capacity establishes a first vicious circle.
Isolation strategies like confinement furthermore restrict access to physical activity (PA), in particular if usually practiced outdoors or in groups. Trends of dramatically reduced general non‐residential mobility following measures to contain the epidemic can currently be observed all over the world (https://www.google.com/covid19/mobility/) and likely reflect an overall reduction of PA. PA, however, on one hand is known to have robust beneficial effects on anxiety and depression, 4 very likely accentuated if performed outdoors or in groups. On the other hand, chronic stress may also reduce the readiness to practice PA, 4 thus constituting another vicious circle.
We argue that not enough public emphasis is yet put on the importance of regular PA during confinement. Beside the well‐known advantageous effects of regular PA on all‐cause mortality, 5 and in particular morbidities considered as risk factors for severe COVID‐19 disease outcome, as well as immunological benefits of PA, 6 its immediate mood‐enhancing, stress‐alleviating and long‐term mental health improving effects 7 are of highest relevance for the current social situation.
While the importance of maintaining PA during the epidemic is largely acknowledged, provided the adherence to physical distance recommendations, there is a risk that especially vulnerable parts of the population fall short of staying active. It can be assumed that the implementation of home training activities especially for the elderly, in particular in combination with motivation‐enhancing video conferencing tools, but also communication (eg, by social media) of the necessity of PA during physical distancing, is more difficult. Personalized advise of general practitioners could be integral to fill such communication gaps.
Whereas group activities requiring physical proximity clearly should be avoided during the epidemic (but are recommended, if the possibility exists to perform them remotely, for example using video conferencing tools), performing PA outdoors produces distinct synergistic benefits with regard to viral infection. 8 Fear of infection as well as political measures to promote physical distancing may for example reduce frequentation of public parks, an activity commonly associated with higher PA levels, and potentially to an even higher degree in older people. 9 We interrogated Google`s recently released COVID‐19 Community Mobility Reports and found highly divergent activity patterns in terms of frequentation of parks during the epidemic across European countries, with particular differences between Nordic and South‐European countries (Figure 1). This may be attributable to the regional severity of the COVID‐19 outbreak, to nation‐specific political measures, or to meteorological or geographical peculiarities but will certainly have modulating effects on COVID‐19 infection incidence. The directionality of such effects—(a) increased virus spreading caused by insufficient physical distance or (b) mitigation of disease progression and stress due to PA, fresh air, sunshine, and associated vitamin D production 10 —will have to be assessed in post‐epidemic analyses. Provision of more complete data sets, for example, by Google is of great interest to assess the associations of mobility and activity with COVID‐19 spreading, severity of infections, and secondary physical and mental health consequences.
FIGURE 1.
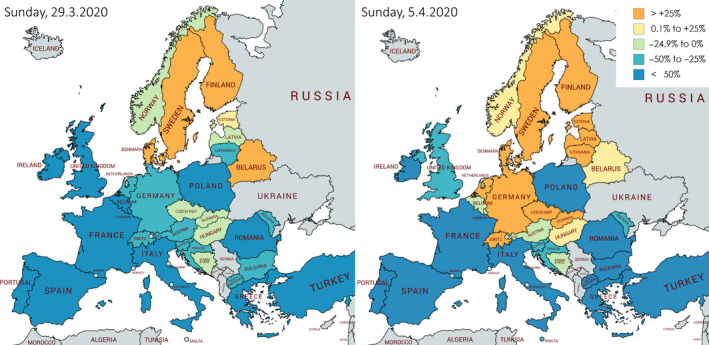
Frequentation of parks on two sundays during the COVID‐19 epidemic. Mobility (visits and length of stay) related to parks according to Google`s COVID‐19 Community Mobility Reports (https://www.google.com/covid19/mobility/) for European countries, for which data were available. Data reflect daily snapshots as of 29.3.2020 and of 5.4.2020, accessed 4.4.2020, 11.00 am and 10.4.2020, 12 am, respectively (percentages as compared to a baseline for the country and the corresponding day of the week (median value across the 5‐week period 3.1. to 6.2.2020). Map created with https://mapchart.net
The uncertainty of the length of confinement strategies in either case adds to the necessity to interrupt the described vicious circles in order to prevent both overlapping additional burden on the health system capacities and long‐lasting mental health deterioration in the society subsequent to the COVID‐19 epidemic. We urge the rapid issuing and appropriate dispensing of public PA recommendations adapted to isolation conditions and tailored to specific risk groups, including relevant patient groups and the elderly.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
REFERENCES
- 1. Gao J, Zheng P, Jia Y, et al. Mental Health Problems and Social Media Exposure During COVID‐19 Outbreak. SSRN Electronic Journal. 2020. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Morey JN, Boggero IA, Scott AB, Segerstrom SC. Current directions in stress and human immune function. Curr Opin Psychol. 2015;5:13‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sandi C, Haller J. Stress and the social brain: behavioural effects and neurobiological mechanisms. Nat Rev Neurosci. 2015;16(5):290‐304. [DOI] [PubMed] [Google Scholar]
- 4. Stults‐Kolehmainen MA, Sinha R. The effects of stress on physical activity and exercise. Sports Med. 2014;44(1):81‐121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Burtscher J, Burtscher M. Run for your life: tweaking the weekly physical activity volume for longevity. Br J Sports Med. 2019. 10.1136/bjsports-2019-101350. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 6. Nieman DC, Wentz LM. The compelling link between physical activity and the body's defense system. J Sport Health Sci. 2019;8(3):201‐217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mikkelsen K, Stojanovska L, Polenakovic M, Bosevski M, Apostolopoulos V. Exercise and mental health. Maturitas. 2017;106:48‐56. [DOI] [PubMed] [Google Scholar]
- 8. Hobday RA, Cason JW. The open‐air treatment of pandemic influenza. American journal of public health. Am J Public Health. 2009;99(Suppl 2):S236‐S242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kaczynski AT, Potwarka LR, Smale BJ, Havitz ME. Association of parkland proximity with neighborhood and park‐based physical activity: variations by gender and age. Leis Sci. 2009;31(2):174‐191. [Google Scholar]
- 10. Grant WB, Lahore H, McDonnell SL, et al. Evidence that vitamin D supplementation could reduce risk of influenza and COVID‐19 infections and deaths. Nutrients. 2020;12(4):988. [DOI] [PMC free article] [PubMed] [Google Scholar]


