1. BACKGROUND
Coronavirus disease 2019 (COVID‐19), emerged only a few months ago in China, is now a global pandemic (see Figures 1 and 2). The significant medical complications, morbidity and the rapid international spread have led to the swift adoption of important public health and political measures across the world. Most countries have chosen to isolate positive cases and those they are in close contact with, and to limit social interactions to reduce transmission. The overall consequences of COVID‐19 on health, humanitarian and economic domains remain unknown. As of April 15, 2020, the World Health Organization (WHO) reported 1,914,916 confirmed cases of infection (with 123,010 deaths) extending to almost all countries across the globe (https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200415-sitrep-86-covid-19.pdf?sfvrsn=c615ea20_2).
Figure 1.

Distribution in Europe of number of cumulative infected cases due to COVID‐19. Source: https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide [Colour figure can be viewed at http://wileyonlinelibrary.com]
Figure 2.
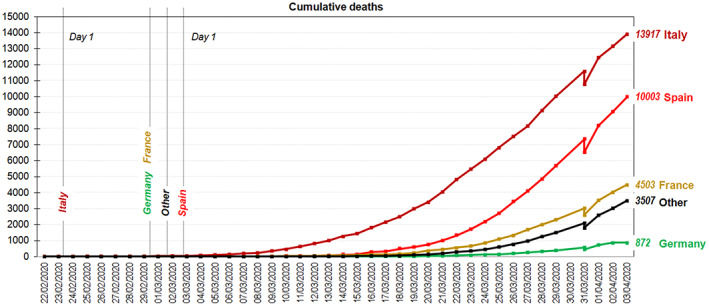
Distribution in Europe of number of cumulative deaths due to COVID‐19. Source: https://www.ecdc.europa.eu/en/publications-data/download-todays-data-geographic-distribution-covid-19-cases-worldwide [Colour figure can be viewed at http://wileyonlinelibrary.com]
Besides the consequences that this pandemic is having on public health (Onder, Rezza & Brusaferro, 2020), it stands to have an important impact on mental health (Fiorillo & Gorwood, 2020; Li, Wang, Xue, Zhao, & Zhu, 2020; Torales et al., 2020), including the mental state of patients who are suffering from the infection, family members who have lost loved ones due to this disease, health professionals, the general population and patients who had a mental health problem before the pandemic, who have seen their symptoms increase and/or have had their treatment disrupted (Duan & Zhu, 2020; Kang et al., 2020; Xiang et al., 2020; Wang et al., 2020). Several studies in Asia are reporting a higher prevalence of post‐traumatic stress disorders (PTSD) after COVID‐19 within the general population (Liu et al., 2020; Wang, Pan et al., 2020) and problems with anxiety and depression (Nguyen et al., 2020; Qiu et al., 2020; Cao et al., 2020; Wang, Di, Ye & Wei, 2020).
2. GENERAL IMPLICATIONS FOR EATING DISORDERS
The effect of COVID‐19 on eating disorder (ED) patients remains unknown. These patients are at high physical risk [for example, frailty in anorexia nervosa (AN), electrolyte disturbances on bulimia nervosa (BN), and cardiovascular risk in binge eating disorder (BED)], and psychological stress due to confinement and the distress caused by uncertainty and a decrease in usual treatment (Dalle Grave, 2020). We might anticipate that the severity of the ED symptomatology and carer burden will increase, as it may not be possible to readily implement treatment according to evidence‐based guidelines (Peckmezian & Paxton, 2020; van den Berg et al., 2019).
Concerns about health and fitness during confinement might serve as a precipitating factor for the development of an ED in vulnerable individuals. Further risk factors may also contribute to the likelihood of developing and ED, such as increased time spent using social‐media and the toxic influence of the objectification of the thin ideal. Isolation and loneliness are common consequences of AN and may be exaggerated by imposed quarantine. Problems with emotional regulation may trigger ED symptoms (binge eating episodes and consequent purging behaviors) (Manasse et al., 2018), while a consequence of increased external control may be reduced food intake (Masheb, Dorflinger, Rolls, Mitchell, & Grilo, 2016). Maladaptive emotional reactions from family members under the stress of confinement may lead to aggression and/or fragmentation and splitting.
In a pilot study at the ED Unit of the Department of Psychiatry, at the University Hospital of Bellvitge (Barcelona, Spain), we used a survey to monitor the impact of the first two weeks of confinement. A total of 32 patients [13 AN, 10 BN), 5 other specified feeding or ED (OSFED) and 4 BED], with a mean age of 29.2 years old (range 16–49), most of them females (N = 29; 90.6%), took part in this telephone survey. Most of the patients presented worries about increased uncertainties in their lives, such as the risk of COVID‐19 infection of themselves or their loved ones, the negative impact on their work, and their treatment. Almost 38% (12 out of 32) reported impairments in their ED symptomatology and 56.2% (18 out of 32) reported additional anxiety symptoms, of whom, four patients noted that stress made it difficult for them to control their grazing behavior and emotional eating.
In the context of COVID‐19, and in many health settings, only urgent visits and inpatient treatments settings for severe ED cases are provided and—where possible—online treatments (instead of face‐to‐face) have been recommended. Restrictions include the closure of day hospitals and outpatient facilities (e.g., Spain, Austria, USA and UK). However, in many countries, there has been a rapid implementation of technological interventions in order to provide telemedicine counseling and online treatments (including family psychoeducation), as it is known that delays in starting appropriate treatments for newly referred patients can lead to worsening of symptomatology. This can allow ED patients to be treated in outpatient settings during the COVID‐19 period. Also, communication between health care providers and their support system (families and friends) can be managed by individual or group methods of telecommunication. The latter overcomes problems in confidentiality, as general, rather than individual, matters are discussed. It allows for families to get support and reduces the stigma they may feel. Online‐ and e‐health measures for ED patients have been developed and tested for over 20 years worldwide and are available for implementation, but more research is necessary (Anastasiadou et al., 2018; Anderson et al., 2017; Barakat et al., 2019; Vollert et al., 2019; Zerwas et al., 2017). However, some aspects of the assessment can be challenging to monitor without face‐to‐face contact or some form of surrogate measure (Keshen et al., 2020; McLean et al., 20192019), especially in more extreme cases (e.g., severely underweight, non‐suicidal self‐injury, self‐destructive patients). In these cases, hospitalisation can be necessary, for safeguarding the patient, their families and professionals (Dalle Grave, 2020).
3. EDS AND FAMILY CONCERNS
In the following section, we describe some of the challenges and solutions to managing AN in the community in the context of COVID‐19. This information comes from an online multifamily chat group consisting of patients with a diagnosis of AN (n = 8) and their carers in the UK. The group was anonymous, although patient/carer usernames were labelled with P and C, respectively. The topic of the group focused on how they were coping with the rapidly changing environment. Isolation was recognised by patients and carers as being negatively associated with their mental health. The following themes emerged (see Table 1):
Table 1.
Results obtained from qualitative analysis around the different domains
| Themes | Example quotes from AN patients (P) and carers (C) |
|---|---|
| Connecting in isolation |
P1: “I don't like using the phone or video calling… I don't want to see myself, but I do want to see the person I'm talking to. The problem is that you don't get the same level of non‐verbal communication, which I really need. It's going to be tough!” P2 “Social media can be unhelpful with different adverts popping up or comments from others. Which makes the isolation feel worse […] For that reason, I won't use social media to try and protect my mental health.” P4: “…you can filter it so only people who have positive or helpful content can be seen. I have found it great to stay connected.” C5: “i think social media can trigger many negative thoughts, but i try to concentrate and only look at the positive and helpful things there are. As a carer, its also easy to feel isolated and generally whilst others are empathetic, it's hard to truly understand. When I'm finding things hard, I connect with pages or those who I know can really help.” |
| Helping others versus helping oneself |
P4 “I have also been offering support and listening ear to those who are feeling particularly anxious presently. This makes me feel a little more connected when able to talk through issues.” P5 “I feel like I've being very socially isolated for a long time […] and find it really fuels my depression. However, I've now joined a community project to help elderly people and those who are vulnerable” P6: “I know when I feel threatened (by C‐19 for example!), I go into 'drive' mode and try to take on the world and do everything for everyone. Eating is usually the first casualty of this behaviour.” P2: “…I agree about the challenge of C‐19 and feel that I may struggle a lot with the change and on these days won't push myself but try to be kind to myself by maybe watching a film.” |
| Challenges of reduced professional support |
P5: “I think I'm most worried if I can't have any appointments and miss weigh ins in which I know for me can be helpful to not constantly be knowing my weight all the time but I think going from one extreme to another will be hard. Also carrying on challenges such as going to restaurants etc well will come to a stop… I'm worried how this will affect my recovery.” P6: “…My ED treatment has gone virtual. I completely understand and agree with it as a course of action, but it will certainly lack something both in terms of therapeutic content and physically with a lack of weigh ins etc. The level of accountability seems far lower, but in some ways the incentive to ensure health at such an unsettling time (and with kids to care for) weighs in the opposite direction. It's certainly a very unsettling time.” C2: “My daughter finds cooking a stress reliever but […] she will now have much more time on her hands at home and it will be a question of not allowing cooking to be the only thing she does as this in itself can become a compulsion and unhelpful.” |
|
Balancing the needs of the ED individual within the family |
P3: “…[I]… like structure and routine whereas my husband and kids are the opposite which i find challenging” P7: “I will try and plan some non‐ED activities to do with my carer. Hopefully this isolation period will be a good bonding experience and a time during which I can challenge some ED behaviours within a safe environment and with support” C2: “…definitely a good idea to plan in non‐ED activities in the weeks ahead ‐ there is a lot of unknown and I think most patients with an ED find this extremely challenging at the best of times.” C8: “Thanks [patient] for the reminder that our daughter may appreciate more help than usual in planning activities to keep her busy in these chaotic times.” |
3.1. Connecting in isolation
Handling the dramatic shift in communication during isolation prompted discussion on strategies to stay connected. AN patients were ambivalent about using social media and video calls. A negative consequence of video calls was the heightened awareness of bodily self, which prompted self‐criticism that they perceived as harmful to their recovery. Some patients coped with this through modifying what was visible in their social media accounts and sought comfort in viewing positive and recovery‐focused peer‐support accounts. However, others believed it was safer not to use potentially triggering forms of communication. Carers demonstrated a strong awareness around the issues of isolation and increased communication challenges for their loved ones with AN, as well as for themselves. However, they were resourceful in learning and sharing ideas for remote communication methods.
3.2. Helping others versus helping oneself
Helping vulnerable others was highlighted as providing a sense of purpose for both patients and carers. Reaching out to friends and family as well as people in need of support within the wider community (e.g., elderly members of the neighborhood) were used to counteract loneliness. However, there was recognition among some patients that a tendency to put others' needs before their own negatively affected their ability to manage their own health. Strategies for self‐care (e.g., relaxing distractions, including reading/television/photography) were discussed among the patients as important when dealing with overwhelming feelings associated with the sudden change in daily life. Carers did not report strategies for self‐care other than the need to stay in communication with family/friends/neighbours/support groups.
3.3. Challenges of reduced professional support
Fears around sudden reduction in contact with the patients' clinical teams were strongly expressed by the group. A lack of time for professionals to prepare patients and their families for a change in treatment was connected to increased feelings of panic and a sense of loss of control already felt with the escalation of COVID‐19. Although some patients had access to online therapy, it was agreed that a lack of face‐to‐face accountability (i.e., lack of weigh‐ins) would require increased self‐management for patients. Patients and carers alike feared for a deterioration in AN recovery. There was an awareness among all that this period of uncertainty and instability would lead to increased reliance on ED thoughts and behaviours. In particular, how to manage reliance on activities that had the potential to be harmful to recovery (e.g., obsessive exercise and cooking) were discussed as being critical for managing ED recovery at home.
3.4. Balancing the needs of the ED individual within the family
A need for routine and structure was highlighted as being crucial for patients as a way of coping with change and preventing boredom, which often led to increased ED preoccupations. Carers described their increased role in the support and management of their loved one's recovery. They shared creative ideas such as creating meal plans at home and undertaking therapeutic activities (e.g., constructing restaurant challenges at home). “Stay at home” and self‐isolation strategies were discussed as resulting in increased burden for carers and changing family dynamics. Balancing the needs of the individuals with an ED (for stability) with flexibility to adjust for the needs of the whole family, particularly children, was seen as crucial but challenging. It was evidently difficult to balance multiple care giving needs and work adjustment, whether working from home, sudden lack of employment, or increased workload.
4. THERAPIST AND STAFF WORKING IN ED
Pandemics pose a double care burden on health care professionals (Aoun, Joundi, & El Gerges, 2019; Li et al., 2018; Raven, Wurie, & Witter, 2018). A recent study in China in health care workers (nurses, physicians) who were exposed to COVID‐19 showed that many of them were suffering from distress, depression, anxiety and insomnia (Lai et al., 2020). Symptom severity was more pronounced in nurses, women and frontline health care workers (Lai et al., 2020). Quarantine can lead to post‐traumatic stress symptoms, anger, confusion, and suicide. The severity of these symptoms increases with the duration of the quarantine and can persist over many years (Brooks et al., 2020). Health care professionals have concerns about becoming infected themselves, causing their units to be understaffed and/or infecting their loved ones (Brooks et al., 2020).
Self‐care, teamwork, networking and cooperation between health care professionals is crucial. The following factors reduced stress: (i) communication with colleagues from own/other centers, (ii) team supervision, (iii) appreciation from clients/superiors/society and (iv) awareness of doing something meaningful (Binder et al., 2020). Finally, in this critical situation, where fears and uncertainty are involved, it is also important for health care professionals to disconnect from work and to take care of themselves. Self‐care includes structuring the day, developing a connected healthy lifestyle and accessing professional help when necessary (Counselling & Development Centre, 2020; Greenberg, Docherty, Gnanapragasam, & Wessely, 2020).
5. FUTURE CHALLENGES AND POTENTIAL THERAPY CHANGES
The COVID‐19 pandemic will have important clinical repercussions for mental health and may produce substantial changes in the usual diagnostic and therapeutic strategies. It highlights the core need for connection and the pain of loneliness which are often central but sometimes forgotten symptoms of people with pre‐existing mental health problems. Patients, such as those with EDs, who often have poor insight into their illness and find social–emotional communication difficult, may delay help‐seeking. Likewise, this fact will become even more relevant in cases in which there is, in addition to the ED, dual disorders and/or comorbidity with other pathologies, which complicates the progression and severity of the main ED (see some recommendations in Table S1, as supplementary information online, and its translation into different languages).
Necessity, the mother of invention, may again be proved to lead to a step change in our care models. Thus, the current enforced immersion in new online therapeutic and management strategies may lead to more widespread adoption of more efficient and effective, mixed methods of connection. Because we are forced to overcome our own fear of novelty and uncertainty, we may find we have more choice and flexibility with a more personalized treatment palette as to what and how might work best for whom.
Supporting information
Table S1 STRATEGIES AND RECOMMENDATIONS IN FRONT OF COVID‐19
ACKNOWLEDGEMENTS
We thank CERCA Programme/ Generalitat de Catalunya for institutional support. This work was partially supported by Instituto de Salud Carlos III (PI17/01167 and SLT006/17/00246). CIBEROobn and CIBERSAM are both initiatives of ISCIII Spain. We thank Dr. Monica Leslie, Isabel Sánchez, Isabel Baenas, Nadine Riesco, Paolo PP Machado, Jon Arcelus, Walter Bouman, Jue Chen, Nathalie T. Godart, Anna Keski‐Rahkonen, Youl‐Ri Kim, Anders Hakansson, Tetyana Ilnytska, Jan Rosenvinge, Daniel Stein, Mikhail F. Borisenkov, Sergey Popov, Ferenc Túry, Brigita Bax and Robert van Voren, for their translations and suggestions in the recommended material.
REFERENCES
- Anastasiadou, D. , Folkvord, F. , & Lupiañez‐Villanueva, F . (2018). A systematic review of mHealth interventions for the support of eating disorders. Eur Eat Disord Rev, 26(5), 394–416. doi:10.1002/erv.2609 [DOI] [PubMed] [Google Scholar]
- Anderson, K. E. , Byrne, C. E. , Crosby, R. D .,
- Aoun, A. , Joundi, J. , & El Gerges, N. (2019). Prevalence and correlates of a positive screen for eating disorders among Syrian refugees. European Eating Disorders Review, 27, 263–273. 10.1002/erv.2660 [DOI] [PubMed] [Google Scholar]
- Barakat, S. , Maguire, S. , Smith, K. E. , Mason, T. B. , Crosby, R. D. , & Touyz, S . (2019). Evaluating the role of digital intervention design in treatment outcomes and adherence to eTherapy programs for eating disorders: A systematic review and meta‐analysis. Int J Eat Disord, 52(10), 1077–1094. doi:10.1002/eat.23131 [DOI] [PubMed] [Google Scholar]
- Binder, A. , Denkinger, J. , Rometsch‐Ogioun El Sount, C. , Windthorst, P. , Engelhardt, M. , Ringwald, J. , … Junne, F. (2020). Psychological burden, stressors and resources of social workers working with women and children who suffered extreme violence by the ‘Islamic state’: A mixed method study. Journal of Psychosomatic Research, 132, 109959 10.1016/j.jpsychores.2020.109959 [DOI] [PubMed] [Google Scholar]
- Brooks, S. K. , Webster, R. K. , Smith, L. E. , Woodland, L. , Wessely, S. , Greenberg, N. , & Rubin, G. J. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395, 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, W., Fang, Z., Hou, G., et al. (2020). The psychological impact of the COVID‐19 epidemic on college students in China [published online ahead of print, 2020 Mar 20]. Psychiatry Res, 287, 112934. doi:10.1016/j.psychres.2020.112934 [DOI] [PMC free article] [PubMed]
- Counselling & Development Centre . (2020). Self‐care tips for your psychological well‐being during the coronavirus outbreak. Hong Kong, China: Hong Kong Baptist University Centre, Office of Student Affairs; https://sa.hkbu.edu.hk/cdc/self-care-tips_2020#know-you-stress-level [Google Scholar]
- Dalle Grave, R. (2020). Coronavirus disease 2019 and eating disorders Eating Disorders: The Facts. Retrieved from https://www.psychologytoday.com/us/blog/eating-disorders-the-facts/202003/coronavirus-disease-2019-and-eating-disorders
- Duan, L. , & Zhu, G. (2020). Psychological interventions for people affected by the COVID‐19 epidemic. Lancet Psychiatry, 7, 300–303. 10.1016/S2215-0366(20)30073-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiorillo, A. , & Gorwood, P. (2020). The consequences of the COVID‐19 pandemic on mental health and implications for clinical practice. European Psychiatry, 63, 1–4. 10.1192/j.eurpsy.2020.35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenberg, N. , Docherty, M. , Gnanapragasam, S. , & Wessely, S. (2020). Managing mental health challenges faced by healthcare workers during covid‐19 pandemic. The BMJ, 368 10.1136/bmj.m1211 [DOI] [PubMed] [Google Scholar]
- Kang, L. , Li, Y. , Hu, S. , Chen, M. , Yang, C. , Yang, B. X. , … Liu, Z. (2020). The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry, 7(3), e14 10.1016/S2215-0366(20)30047-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keshen, A. , Helson, T. , Ali, S. , Dixon, L. , Tregarthen, J. , & Town, J. (2020). Efficacy and acceptability of self‐monitoring via a smartphone application versus traditional paper records in an intensive outpatient eating disorder treatment setting. European Eating Disorders Review, 28(4), 1–7. 10.1002/erv.2727 [DOI] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. , Cai, Z. , Hu, J. , Wei, N. , … Hu, S. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease. JAMA Network Open, 3(3), e203976 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, S. , Wang, Y. , Xue, J. , Zhao, N. , & Zhu, T. (2020). The impact of COVID‐19 epidemic declaration on psychological consequences: A study on active Weibo users. International Journal of Environmental Research and Public Health, 17(6), E2032 10.3390/ijerph17062032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, Y. , Wang, H. , Jin, X. , Li, X. , Pender, M. , Song, C. , … Wang, Y. (2018). Experiences and challenges in the health protection of medical teams in the Chinese Ebola treatment center, Liberia: A qualitative study. Infectious Diseases of Poverty, 7, 92 10.1186/s40249-018-0468-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, N. , Zhang, F. , Wei, C. , Jia, Y. , Shang, Z. , Sun, L. , … Liu, W. (2020). Prevalence and predictors of PTSS during COVID‐19 outbreak in China hardest‐hit areas: Gender differences matter. Psychiatry Research, 287, 112921 10.1016/j.psychres.2020.112921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manasse, S. M. , Schumacher, L. M. , Goldstein, S. P. , Martin, G. J. , Crosby, R. D. , Juarascio, A. S. , … Forman, E. M. (2018). Are individuals with loss‐of‐control eating more prone to dietary lapse in behavioural weight loss treatment? An ecological momentary assessment study. European Eating Disorders Review, 26, 259–264. 10.1002/erv.2583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masheb, R. M. , Dorflinger, L. M. , Rolls, B. J. , Mitchell, D. C. , & Grilo, C. M. (2016). Binge abstinence is associated with reduced energy intake after treatment in patients with binge eating disorder and obesity. Obesity (Silver Spring), 24(12), 2491–2496. 10.1002/oby.21664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean, S. A. , Caldwell, B. , & Roberton, M . (2019). Reach Out and Recover: Intentions to seek treatment in individuals using online support for eating disorders. Int J Eat Disord, 52(10), 1137–1149. doi:10.1002/eat.23133 [DOI] [PubMed] [Google Scholar]
- Nguyen, H. C. , Nguyen, M. H. , Do, B. N. , Tran, C. Q. , Nguyen, T. T. P. , Pham, K. M. , … Duong, T. V. (2020). People with suspected COVID‐19 symptoms were more likely depressed and had lower health‐related quality of life: The potential benefit of health literacy. Journal of Clinical Medicine, 9, 965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onder, G., Rezza, G., & Brusaferro, S. (2020). Case‐Fatality Rate and Characteristics of Patients Dying in Relation to COVID‐19 in Italy [published online ahead of print, 2020 Mar 23]. JAMA;10.1001/jama.2020.4683. doi:10.1001/jama.2020.4683Peckm [DOI] [PubMed]
- Peckmezian, T. , & Paxton, S. J. (2020). A systematic review of outcomes following residential treatment for eating disorders. European Eating Disorders Review, 28(3), 1–14. 10.1002/erv.2733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu, J., Shen, B., & Zhao, M., et al. (2020). A nationwide survey of psychological distress among Chinese people in the COVID‐19 epidemic: implications and policy recommendations. General Psychiatry, 33, e100213. doi:10.1136/gpsych‐2020‐100213 [DOI] [PMC free article] [PubMed]
- Raven, J. , Wurie, H. , & Witter, S. (2018). Health workers' experiences of coping with the Ebola epidemic in Sierra Leone's health system: A qualitative study. BMC Health Services Research, 18, 251 10.1186/s12913-018-3072-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torales, J., O’Higgins, M., Castaldelli‐Maia, J. M., & Ventriglio, A. (2020). The outbreak of COVID‐19 coronavirus and its impact on global mental health. International Journal of Social Psychiatry. 10.1177/0020764020915212 [DOI] [PubMed]
- van den Berg, E. , Houtzager, L. , de Vos, J. , Daemen, I. , Katsaragaki, G. , Karyotaki, E. , … Dekker, J. (2019). Meta‐analysis on the efficacy of psychological treatments for anorexia nervosa. European Eating Disorders Review, 27, 331–351. 10.1002/erv.2683 [DOI] [PubMed] [Google Scholar]
- Vollert, B. , Beintner, I. , Musiat, P. , Gordon, G. , Görlich, D. , Nacke, B. , … Jacobi, C. (2019). Using internet‐based self‐help to bridge waiting time for face‐to‐face outpatient treatment for bulimia nervosa, binge eating disorder and related disorders: Study protocol of a randomized controlled trial. Internet Interventions, 16, 26–34. 10.1016/j.invent.2018.02.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C. S. , & Ho, R. C. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729 10.3390/ijerph17051729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, Y. , Di, Y. , Ye, J. , & Wei, W . (2020). Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID‐19) in some regions of China [published online ahead of print, 2020 Mar 30]. Psychol Health Med, 1–10. doi:10.1080/13548506.2020.1746817 [DOI] [PubMed] [Google Scholar]
- Xiang, Y. T. , Yang, Y. , Li, W. , Zhang, L. , Zhang, Q. , Cheung, T. , & Ng, C. H. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry, 7(3), 228–229. 10.1016/S2215-0366(20)30046-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zerwas, S. C. , Watson, H. J. , Hofmeier, S. M. , Levine, M. D. , Hamer, R. M. , Crosby, R. D. , … Bulik, C. M. (2017). CBT4BN: A randomized controlled trial of online chat and face‐to‐face group therapy for bulimia nervosa. Psychotherapy and Psychosomatics, 86, 47–53. 10.1159/000449025 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 STRATEGIES AND RECOMMENDATIONS IN FRONT OF COVID‐19


