Lung ultrasound examination has been suggested as a useful tool with which to detect lung involvement during the COVID‐19 pandemic, desirable particularly for pregnant women 1 , 2 , 3 . We developed a specific single‐day training program to provide gynecologists and obstetricians who are already skilled in ultrasound examination with the theoretical background required for recognition of normal and the main abnormal lung ultrasound patterns.
The training program was developed at the Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy and University of Trento, Trento, Italy, and is available on a dedicated website (https://covid19.disi.unitn.it/iclusdb/login); to obtain access to the platform please send a request to libertario.demi@unitn.it. The program design was presented to the COVID‐19 Research Ethics Committee, who evaluated and approved the project (Prot. 1370/20, ID: 3067).
In this study, we evaluated the feasibility and effectiveness of this rapid training program by providing it to a group of 11 trainees and comparing the number of correct classifications in their pre‐ and post‐training results. The trainees were gynecologists and obstetricians who were skilled in obstetric and/or gynecological ultrasound examination, but with no experience in lung ultrasound; three of them had been involved for 1 week in meetings with pneumologists to prepare the recent publication on ‘How to perform lung ultrasound in pregnant women with suspected COVID‐19’ 4 . The trainers were two pneumologists (A.S. and R.I.) and one pediatrician (D.B.), all of whom have more than 10 years of experience in lung ultrasound examination, in clinical practice as well as for the purposes of research and teaching.
The training program consisted of three phases. Phase 1 consisted of a 15‐min pretraining test, in which each of the 11 trainees was asked to assess 10 ultrasound videoclips, which had been obtained by one of four experts (G.S., R.C., A.S., R.I). Each videoclip showed a normal ultrasound pattern or one of five typical pathological patterns. After watching the videoclip, each trainee was asked to classify the pattern, choosing from among the following possibilities (Figure 1): (a) normal; (b) clear and distinct vertical artifacts with small pleural alterations (Score = 1) or broken pleural line and small consolidations (Score = 2); (c) white lung without evident subpleural consolidations (Score = 3); (d) white lung with evident subpleural consolidations (Score = 3); (e) pattern not compatible with COVID‐19 pneumonia (massive consolidations); (f) pattern not compatible with COVID‐19 pneumonia (pleural effusions) 5 . Phase 2 consisted of a 2‐hour theoretical course, addressing clinical and ultrasound issues related to lung ultrasound imaging 5 . Phase 3 was a 15‐min post‐training test, in which the trainees had to reassess the 10 ultrasound videoclips, which were presented in a different order.
Figure 1.
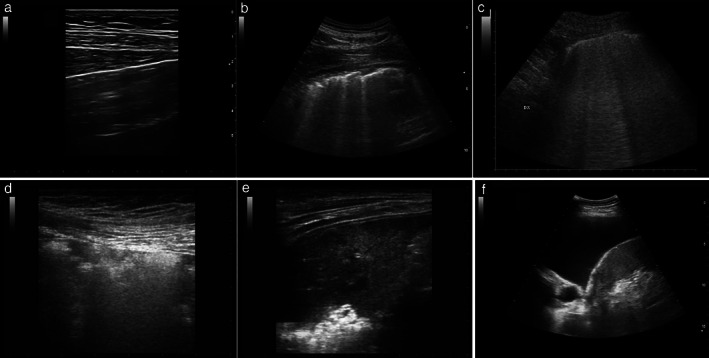
Grayscale ultrasound images (intercostal view) of lungs illustrating six patterns (one normal and five abnormal) from which trainees could choose. (a) Normal lung, showing subcutaneous layers, regular pleural line and horizontal artifacts, called ‘A‐lines’. (b–d) Abnormal patterns suggestive of pneumonia: (b) clear and distinct vertical artifacts with disrupted pleural line; (c) completely white area (so‐called ‘ultrasonographic white lung’) with neither horizontal reverberations (A‐lines) nor isolated B‐lines visible; (d) features of ‘white lung’ and subpleural consolidations. (e,f) Abnormal patterns not compatible with pneumonia: (e) massive consolidation; (f) features of pleural effusion.
The number of correct diagnoses (pre‐ and post‐training) was recorded for each participant (Table S1). The median number of correct answers among the trainees was 6 (range, 2–10) at the pretraining test and 9 (range, 6–10) at the post‐training test. All trainees initially achieving 100% correct answers remained at this level post‐training, and all those initially achieving less than 100% improved after training, with the median difference in number of correct answers being + 2 (range, 0 to + 6). Looking more closely at the post‐training classifications, eight of the 11 trainees correctly discriminated normal from pathological patterns in all cases, two did so in 90% of cases and one in 80% of cases.
In conclusion, our preliminary experience suggests that a rapid teaching program is sufficient to provide gynecologists and obstetricians who are already skilled in obstetric and/or gynecological ultrasound examination with the theoretical skills necessary to recognize specific lung ultrasound patterns. We believe that our course represents one possible model for implementing lung ultrasound education and might be a useful launch‐pad for gynecologists and obstetricians involved in the management of pregnant patients with confirmed or suspected COVID‐19.
Supporting information
Table S1 Pre‐ and post‐training test results of 11 participants in rapid‐training program on lung ultrasound examination
Acknowledgments
We thank Dr Antonella Biscione, Dr Francesca Ciccarore, Dr Claudia Codeca, Dr Carmelinda Martino, Dr Floriana Mascilini, Dr Sascia Moresi, Dr Maria Cristina Moruzzi, Dr Marcella Pellegrino and Dr Silvia Salvi of Dipartimento Scienze della Salute della Donna, del Bambino e di Sanità Pubblica, Fondazione Policlinico Universitario Agostino Gemelli, IRCCS, Rome, and Roberto Copetti of the Diagnostic and Interventional Ultrasound Unit, Valle del Serchio General Hospital, Lucca, Italy, for participating in the training program.
Linked article: There is a comment on this article by Joob et al,. Click here to view the Correspondence.
References
- 1. Buonsenso D, Raffaelli F, Tamburrini E, Biasucci DG, Smargiassi A, Inchingolo R, Scambia G, Lanzone A, Testa AC, Moro F. Clinical role of lung ultrasound for diagnosis and monitoring of COVID‐19 pneumonia in pregnant women. Ultrasound Obstet Gynecol 2020; 56: 106–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Buonsenso D, Pata D, De Rose C, Morello R, Moro F, Franchi M, Scambia G, Testa AC. Clinical application of Lung Ultrasound for the management of pregnant women with suspicion of COVID‐19: a review of literature. Ital J Gynaecol Obstet 2020. (In press). [Google Scholar]
- 3. Buonsenso D, Pata D, Chiaretti A. COVID‐19 outbreak: less stethoscope, more ultrasound. Lancet Respir Med 2020. DOI: 10.1016/S2213-2600(20)30120-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moro F, Buonsenso D, Moruzzi MC, Inchingolo R, Smargiassi A, Demi L, Larici AR, Scambia G, Lanzone A, Testa AC. How to perform lung ultrasound in pregnant women with suspected COVID‐19. Ultrasound Obstet Gynecol 2020; 55: 593–598. [DOI] [PubMed] [Google Scholar]
- 5. Soldati G, Smargiassi A, Inchingolo R, Buonsenso D, Perrone T, Briganti DF, Perlini S, Torri E, Mariani A, Mossolani EE, Tursi F, Mento F, Demi L. Proposal for international standardization of the use of lung ultrasound for COVID‐19 patients; a simple, quantitative, reproducible method. J Ultrasound Med 2020. DOI: 10.1002/jum.15285. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 Pre‐ and post‐training test results of 11 participants in rapid‐training program on lung ultrasound examination


