Abstract
The coronavirus disease 2019 (COVID‐19) pandemic has necessitated drastic changes across the spectrum of health care, all of which have occurred with unprecedented rapidity. The need to accommodate change on such a large scale has required ingenuity and decisive thinking. The field of physical medicine and rehabilitation has been faced with many of these challenges. Healthcare practitioners in New York City, the epicenter of the pandemic in the United States, were among the first to encounter many of these challenges. One of the largest lessons included learning how to streamline admissions and transfer process into an acute rehabilitation hospital as part of a concerted effort to make acute care hospital beds available as quickly as possible.
Introduction
Transition of patients from an acute care hospital to an inpatient rehabilitation facility (IRF) is typically cumbersome and labor intensive. The decision‐making process for identifying and referring any individual patient to an IRF is multifactorial. It involves multiple practitioners from various specialties and agreement on recommended discharge disposition. Once past this initial hurdle, others remain. Patients must meet regulatory criteria (such as the “60% rule,” the ability to participate in an intensive level of therapy referred to as the “3‐hour rule,” and receive close medical supervision) as well as patient‐specific insurance criteria in order to obtain authorization for admission. In addition, there must be available beds in the receiving rehabilitation hospital and patients and families must agree with the discharge plan and facility. Given the multifaceted complexity of the process, it is not unusual for it to take 24 to 48 hours from start to finish. 1 In the setting of the mass influx of patients during the coronavirus disease 2019 (COVID‐19) pandemic, a widespread bed shortage was created in local acute care hospitals and local healthcare systems, as well as around the world. 2 In order to respond to this challenge and using the freedom from the declared health emergency in our region, we set out to decrease the complexity of the screening and admission process to less than 6 to 8 hours. In addition to streamlining admissions, we also allowed for flexibility in new types of diagnoses being admitted to our IRF facility, courtesy of the Centers for Medicare & Medicaid Services (CMS) Section 1135 emergency waivers, 3 to both help patients and unload our overburdened acute care system hospitals. After several iterations, we ultimately proved successful.
Administrative Challenges
During times of medical crises, such as the current COVID‐19 pandemic, there is likely to be an extreme shortage of beds in acute care hospitals. In New York City, the epicenter of COVID‐19 in the United States, 4 this bed crisis was drastic with the anticipated need for beds being twice the number of licensed beds in the state. Having an acute care bed shortage can contribute to an increase in mortalities. As opposed to skilled nursing facilities (SNFs), IRFs are required to provide a higher level of medical care and supervision to their patients and at more regular intervals. 5 , 6 Thus, IRFs have the potential ability to substantially contribute to the bed availability in acute care hospitals by transferring patients who are stable enough for acute care discharge but still require medical care or are not yet ready to go home. In many of our regional academic medical centers, inpatient rehabilitation units were temporarily suspended, so that their beds could be added to the cohort of available beds for medical/surgical patients. We have a 150‐bed freestanding acute inpatient rehabilitation hospital in our system that remained operational and thus provided a potential relief for the pressure in the acute care hospitals in the system. We immediately realized that there were two fundamental tasks to complete in order to successfully allow our freestanding rehabilitation hospital to serve to offload patients from the overwhelmed acute care hospitals. The following strategic plans were executed in parallel. The first was to increase bed capacity at the IRF according to perceived need. The second was to develop criteria and adopt a plan to screen and accept patients in an expeditious manner. We recognized that successfully implementing these plans could be lifesaving by making acute care beds available for the most acute COVID‐19 affected patients.
Within the Montefiore Health System there are 11 acute care hospitals and 1 freestanding rehabilitation hospital all located in the Bronx and the lower Hudson valley in New York State. Burke Rehabilitation Hospital is a 150‐bed, freestanding acute inpatient rehabilitation hospital. When the COVID‐19 pandemic reached the United States in January 2020, the earliest identified “hot spot” was located in New Rochelle, New York between Burke and the Montefiore campus in Bronx, New York. The probable impact of this crisis at the local, regional, and state level was immediately apparent to hospital leadership and to local and state government officials. As a result, these leaders identified the need for a rapid response by hospitals to make beds available for the anticipated surge of patients.
As part of a concerted effort throughout our system, all hospitals, including Burke Rehabilitation Hospital, immediately implemented surge plans to increase bed capacity to 150% of regularly licensed limits in accordance with a mandate issued by Andrew Cuomo, the Governor of New York. 7 In the Burke IRF, the process to achieve this mandate required creative thinking. To have more beds available, we closed one of our inpatient therapy gymnasiums and converted that space into a new hospital unit. Beds were quickly purchased, supplemental oxygen using concentrators was put in place, tracks for privacy curtains were purchased and installed, increased staffing demands were anticipated and accommodated, and within 1 week this therapy gym became a new 14‐bed hospital surge unit.
During construction of this new unit, the task of developing new admission criteria and pathways proved even more daunting. Again, this required thinking creatively and beyond our standard operating procedures. Changing our established process required close collaboration between leadership and faculty at the acute care hospitals and specifically physiatry leadership at all sites including the IRF.
The first step involved in developing a new patient screening process was to acknowledge that the patients who would be admitted to the IRF during this emergency were different from the traditional rehabilitation patient. Most of the pending admissions were likely to have unique needs related to complications of COVID 19 infection and were not going to be “traditional candidates” for admission to an acute rehabilitation service. As a result, one of the initial challenges we faced was to prioritize the “traditional rehabilitation candidate” with patients who required more medical support in addition to their rehabilitative needs. In our facility prior to this pandemic, approximately 60% to 65% of our patients were admitted for rehabilitation of a primary neurologic diagnosis, with 20% being admitted for cardiac or pulmonary rehabilitation and the remaining 15% to 20% receiving rehabilitation for a musculoskeletal condition. As the prevalence of COVID‐19 increased in the community it became clear that we would not be able to maintain a COVID‐19 free facility. To identify the best patients for our acute rehabilitation hospital, we worked closely with internal medicine colleagues to best identify the cohort of patients who, although not ready to go home, would be stable enough to continue their recovery in a rehabilitation setting without the level of care provided in an acute care hospital. However, many patients with COVID‐19 pneumonia seemed to be on their way to recovery when they subsequently decompensated to varying degrees. 8 Identifying patients with this clinical profile was complex and resulted in continuously modifying our screening process as new trends emerged. Because of the importance of knowing each patient's COVID‐19 status, every patient in the acute care hospitals displaying any COVID‐19 related symptom was tested. Patients who were hospitalized for other diagnoses and were asymptomatic relative to COVID‐19 were not tested. For patients who were being considered for transfer to IRF and who were found to be COVID‐19 positive, the decision to transfer was made when they were deemed medically stable from a respiratory standpoint and thought to be unlikely to decompensate. Although it has been suggested that ideally patients admitted to IRFs should either be asymptomatic or test COVID negative, we took a different approach given the overwhelming volume of COVID‐19 positive patients in our area. 9 Given our limited knowledge about this disease and its course, these decisions were made on a case‐by‐case basis. We did find that patients with downward trending inflammatory markers and either normal or downward trending ferritin levels tended to be more appropriate for admission to our freestanding acute rehabilitation hospital.
To screen and transfer patients as promptly and safely as possible, we instituted a direct physician‐to‐physician referral and discussion process as the first step of screening. Prior to the epidemic, when a patient was deemed medically appropriate for discharge to an IRF, the referral was made by a social worker or case manager. Although a physician was always the ultimate authority with respect to accepting patients to the rehabilitation hospital, direct communication between physicians at the acute care hospital and rehabilitation hospital did not always occur routinely. We now felt it important that physician‐to‐physician communication occur for each patient under consideration to hasten the decision‐making process and to ensure medical appropriateness of the patent. A physiatrist at the acute care hospital spoke directly with a rehabilitation physician at the rehabilitation hospital at least twice daily to review patients being referred. The value of direct physician to physician communication was quickly appreciated and proved beneficial. This communication improved our ability to triage patients in the acute care hospital and significantly increased the acceptance rate of referred to IRF. Of the first 84 patients in the acute care facility referred for consideration for IRF, 51 were deemed appropriate by the consulting physiatrist. All 51 of these patients were referred to the acute rehabilitation hospital and 50 were accepted and admitted.
Once patients were accepted, assigning a bed within the rehabilitation hospital to meet the patients' needs was the next challenge. Traditionally, the main determinants of room assignments were the gender and diagnosis group. During the COVID‐19 crisis, the COVID status complicated this process and at times even resulted in blocked beds. For double occupancy rooms, there now needed to be consideration of COVID‐19 status in addition to gender or other isolation and respiratory needs. The three groupings of COVID‐19 status that had to be considered were as follows: COVID positive patients, COVID negative patients, and persons under investigation (PUI). Initially, addressing the group of PUI patients was a challenge as it took up to 2 to 3 days for results to return. However, with rapid testing becoming available, the duration of time beds were blocked because of PUI status was markedly reduced to a few hours. Although the process of considering PUI status added a level of complexity to our admissions process, we developed a triaging system that allowed our new fast track system to continue.
We also realized that to decrease the time between referral and IRF admission, we needed to change our processes pertaining to the transfer period. Prior to the COVID‐19 pandemic, following medical acceptance, a preadmission screen and registration process took place at the IRF prior to the actual physical patient transfer. This was identified as a potential point of significant delay but is a regulatory requirement for rehabilitation hospitals. As a result of the CMS 1135 waiver, we were able to create a streamlined process for this part of the admission that allowed more rapid admissions. We instituted a policy allowing the initiation of discharge and transfer immediately upon medical acceptance. Registration, the preadmission screen note, and bed assignment now occur as a parallel process rather than a process in series (Figure 1).
Figure 1.
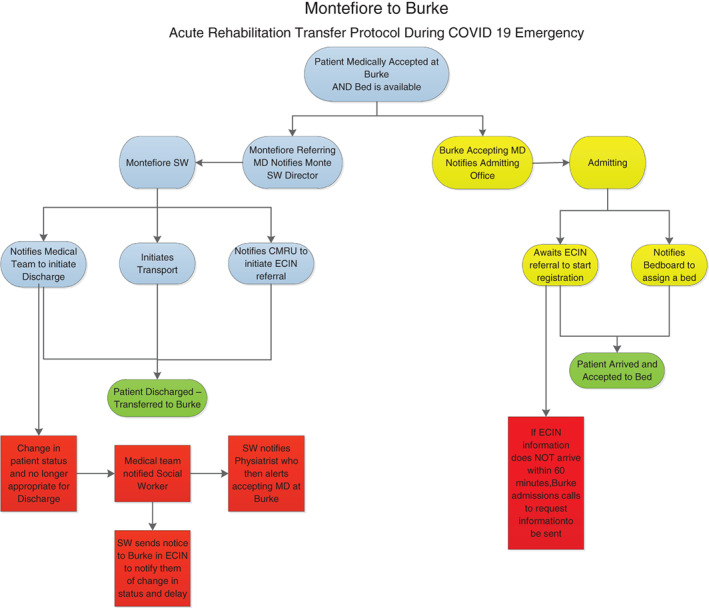
Montefiore to Burke. Acute rehabilitation transfer protocol during COVID‐19 emergency. CMRU = Care Management Resource Unit; ECIN = Extended Care Information Network; SW = social worker
Once admitted, we also had to consider new methods by which we would provide therapy services to our patients. Providing therapy to a large numbers of patients simultaneously in therapy gyms could no longer occur given the need for social distancing. Therapies were transitioned to bedside over time starting with patients who were COVID‐19 positive, followed by PUIs and finally to all remaining patients, while wearing appropriate personal protective equipment (PPE) at all times. The duration of therapy was adjusted, when necessary, to patient tolerance as well any limitations caused by the need for PPE preservation, space, or other logistical concerns. Providing less than 3 hours of therapy, which is normally required in acute rehabilitation hospitals was permitted in accordance with provisions of the Coronavirus Aid, Relief, and Economic Security (CARES) Act, effective 30 March 2020. 10
Conclusion
The value of the lessons learned during this pandemic will have implications as operations return to precrisis state. As it relates to the processes outlined here, the information and experiences that we have attained will help us to restructure our evaluation, referral, and admission processes to acute rehabilitation, but long term they will not entirely match our current state of emergency protocols for a variety of reasons. For example, because of the CMS waiver, we are currently able to immediate accept and transfer a patient once deemed medically appropriate without the need to attain prior authorization (PA), which traditionally can be a rate limiting factor in this process. When the waiver expires and PAs are again required, we will be forced to reintroduce that step into our processes. That said, we have also learned the value of direct physician‐to‐physician discussions about each patient and we will preserve this step.
The cooperation of the acute care hospitals and the IRF teams working together and outside of long‐established protocols allowed the Department of Physical Medicine and Rehabilitation to be an important participant on the throughput team at the Montefiore Health System during the COVID‐19 crisis. With campuses in the Bronx in New York City and in the lower Hudson Valley, including Westchester, Rockland, and Orange counties, we are located at the earliest and most sustained epicenter of this pandemic. Because there was no roadmap for us to follow, we created new processes to bypass chokepoints in the movement of patients throughout the system. Teamwork and the ability to think creatively and cooperatively allowed us to quickly devise a method of transferring patients out of the acute care hospital and into rehabilitation beds, thereby opening acute care beds for patients requiring admission, relieving congestion in our emergency departments, ultimately improving patient flow. It was also essential to work together and coordinate between all system hospitals for rapid testing and other processes that allowed more rapid movement of patients. It is vital that, beyond their medical value, departments of rehabilitation medicine be acknowledged as integral parts of healthcare systems' throughput pathways, especially in times of medical crisis.
Acknowledgments
Jeffrey Menkes for his support.
References
- 1. 2018 Prior Authorization State Law Chart ; 2018. https://www.ama‐assn.org/media/22571/download. Accessed April 9, 2020.
- 2. Boldrini P, Bernetti A, Fiore P. Impact of COVID‐19 outbreak on rehabilitation services and physical and rehabilitation medicine (PRM) physicians' activities in Italy. Eur J Phys Med Rehabil Med. 2020. [DOI] [PubMed] [Google Scholar]
- 3. Lynch C.. Section 1135 waiver flexibilities – New York Coronavirus Disease 2019; 2020. https://www.medicaid.gov/state-resource-center/disaster-response-toolkit/federal-disaster-resources/entry/54067. Accessed April 13, 2020.
- 4. COVID‐19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU) ; 2020. https://coronavirus.jhu.edu/map.html. Accessed April 8, 2020.
- 5.Role of the attending physician in the nursing home. https://www.health.ny.gov/professionals/nursing_home_administrator/docs/11-13_att_phys_role.pdf. Accessed April 13 2020.
- 6.Centers for Medicare and Medicaid Services; 2007. Inpatient rehabilitation therapy services: complying with documentation requirements. https://www.cms.gov/Outreach‐and‐Education/Medicare‐Learning‐Network‐MLN/MLNProducts/downloads/Inpatient_Rehab_Fact_Sheet_ICN905643.pdf. Accessed April 13, 2020.
- 7. Lardieri A. Gov. Andrew Cuomo Orders Hospitals to Increase Capacity by 50%; 2020. https://www.usnews.com/news/health‐news/articles/2020‐03‐23/new‐york‐gov‐andrew‐cuomo‐orders‐hospitals‐to‐increase‐capacity‐by‐50. Accessed April 9, 2020.
- 8. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054‐1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Simpson R, Robinson L. Rehabilitation following critical illness in people with COVID‐19 infection. Am J Phys Med Rehabil. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. The Centers for Medicare and Medicaid Services; 2020. New Waivers for Inpatient Prospective Payment System (IPPS) Hospitals, Long‐Term Care Hospitals (LTCHs), and Inpatient Rehabilitation Facilities (IRFs) due to Provisions of the CARES Act . https://www.cms.gov/files/document/se20015.pdf. Accessed April 17, 2020.


