The SARS‐CoV‐2 (COVID‐19) outbreak became a pandemic in less than 4 months1. Most healthcare systems have seen the capacity to treat surgical patients decrease dramatically owing to the reallocation of resources in response to the pandemic2. Thousands of patients are waiting to undergo an elective surgical procedure, and have become part of the ‘second and third waves’, which are not related directly to the virus but to the large number of patients who have seen their conditions worsened by the delay in receiving appropriate treatment.
Individuals who have developed the coronavirus‐associated disease (COVID‐19) can be detected by using a combination of epidemiological, clinical, radiological and laboratory criteria. COVID‐19 presents with variable severity, although in a large number of patients it is not a life‐threatening condition and its course is mostly benign, limited to a few days or weeks. However, there are some risk factors that increase the odds of developing complications with high mortality rates. Major surgery might be one of these factors.
Attention has been drawn to a potential increase in postoperative morbidity and mortality in patients who undergo major surgery during the incubation period of COVID‐19 infection, as reported in China3. The evidence is of low quality, with few and heterogeneous cases included in an observational study, and large disparities in the complexity and type of surgical intervention. Fortunately, global collaborative initiatives have been launched4 and several registries have been instituted worldwide. As predicted, online resources and social media5 are extremely useful in pushing surgical research during a critical situation like this. The CovidSurg Collaborative is an excellent example6, as represented by the network represented in Fig. 1. Therefore, it is highly likely that better data on the outcomes of patients undergoing surgery during the pandemic will be available soon.
Figure 1.
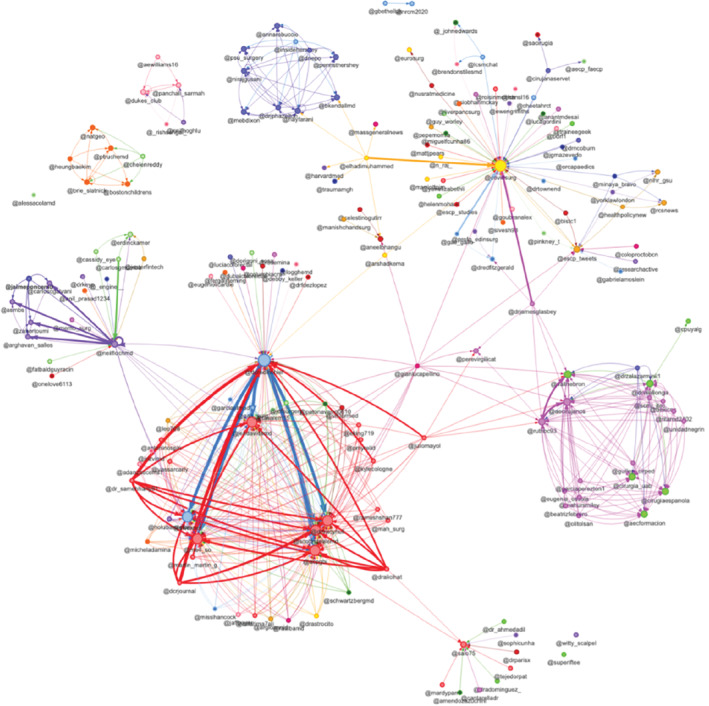
Graphical representation of account network using the hashtag #CovidSurg on Twitter, from 4 to 9 April 2020 Data were analysed and visualized with socioviz.net (https://socioviz.net/).
Given the potential life‐threatening risk for patients, the gradual reintroduction of postponed elective surgical procedures during the pandemic should follow rigorous measures to: avoid a greater perioperative complication rate in patients who develop COVID‐19 in the perioperative period; decrease viral spread within the hospital; and decrease spread of virus beyond the hospital.
Numerous recommendations7, 8, 9 to provide surgical care safely during the pandemic have been issued by national and international scientific societies, but it remains unclear how elective surgery should be restarted under these new, uncertain conditions. In fact, the majority of the actions taken during this pandemic have been made in the absence of hard data to support them. It is reasonable to take into account epidemiological conditions in the community, patients' health, the COVID‐19 status of all members of the surgical team, the facilities and resources available when making decisions about the delivery of surgical care, and provision of information to patients to obtain consent after the peak of the outbreak.
Regarding the community, the actual prevalence of coronavirus infection should be known in order to make the best estimations of the potential risk of COVID‐19 in patients scheduled for elective surgery. However, this would be possible only if mass testing were carried out, and more data gathered to understand and quantify presymptomatic transmission10.
With respect to patients, it is both epidemiologically and clinically reasonable that candidates for elective surgery who may be in the incubation period or who have developed active disease should have their elective procedures postponed until full recovery. Intensive physiotherapy may be wise before the intervention to maximize pulmonary function after surgery. For effective triage, criteria in four domains could be combined (Table 1), although the right time to do this is not certain. Patients cleared for elective surgery should be informed about the general precautions to prevent coronavirus exposure before being admitted to hospital.
Table 1.
Triage criteria for COVID‐19
| Epidemiological evaluation | Close contact in the past 14 days with a possible, probable or confirmed case |
| Clinical assessment | Fever, coughing, sore throat, asthenia, dyspnoea, headache, myalgia or arthralgia, chills, diarrhoea, nausea or vomiting, nasal congestion, hyposmia/anosmia of recent onset |
| Routine laboratory testing | Complete blood count, C‐reactive protein, reverse transcriptase–PCR for SARS‐CoV‐2, specific IgM and IgG |
| Chest imaging | X‐ray (routinely), chest CT (selectively) |
Assessing the health status of the surgical team should involve members across the full cycle of care, including anaesthetists, surgeons, intensivists, nurses, technicians, physiotherapists, etc. A health status checklist might be useful for rapid evaluation of workers before inclusion in teams delivering care to patients who are COVID‐19‐negative. Every member of the team should be either COVID‐19‐negative (as described in Table 1), or should have recovered from symptomatic COVID‐19 with negative reverse transcriptase–PCR tests (2 negative results separated by 48 h may be ideal) or after specific immunity testing (IgM‐negative and IgG‐positive for SARS‐CoV‐2).
Designated operating theatres, ICUs and wards should be used to avoid any contact between patients and teams considered negative for COVID‐19 and patients who may be COVID‐19‐positive and the teams who take care of them. Operating theatres with negative pressure are preferred, and special attention should be paid to procedures considered high risk for aerosol generation (laparoscopy, robotic surgery, thoracic and gastrointestinal surgery). Other strict precautions to avoid direct exposure to patients' secretions should be taken and use of personal protective equipment as indicated by health authorities considered routine.
Very few certainties exist about the management of surgical patients during the COVID‐19 outbreak. For surgical teams and all healthcare providers, the main objectives should be the safe delivery of surgical care without contributing viral spread under what remain incompletely understood conditions. Funders should consider it a top priority to deliver high‐level research facilitating safe surgical care during and after this pandemic. This time will define how our surgical generation will be measured by the scales of history, so let us lead our patients through the mire of pusillanimous polemic that has marred coordinated global responses to our collective vicissitude. We should support the WHO and related bodies ably coping with the Sisyphean strain of viral pandemic problems. Worldwide challenges supersede individual and national interests driven by solipsism and isolationist ideals. This is an opportunity for surgery on a global scale to navigate beyond the healthcare horizon drawn by politicians reliant on our vision. May we lead well, choose well, cut well, stay well.
Disclosure
The authors declare no conflict of interest.
The BJS team wish to reach out to express our support and gratitude to surgeons and healthcare workers around the globe. These are difficult times and your leadership is key to providing the best care possible. BJS welcomes submissions relating to the challenges faced in this pandemic (expect publication within a week). A blog has been launched (cuttingedgeblog.com) and publication of accepted pieces will be within hours.
Best wishes to you all.
Des Winter MD (Editor‐in‐Chief) on behalf of the BJS Editors, Editorial Council and Board
References
- 1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song Y et al.; China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China 2019. N Engl J Med 2020; 382: 727–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Spinelli A, Pellino G. COVID‐19 pandemic: perspectives on an unfolding crisis. Br J Surg 2020; 10.1002/bjs.11627 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lei S, Jiang F, Su W, Chen C, Chen J, Mei W et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID‐19 infection. EClinicalMedicine 2020; 10.1016/j.eclinm.2020.100331 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Søreide K, Hallet J, Matthews JB, Schnitzbauer AA, Line PD, Lai PBS et al. Immediate and long‐term impact of the COVID‐19 pandemic on delivery of surgical services. Br J Surg 2020; 10.1002/bjs.11670 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mayol J, Dziakova J. Value of social media in advancing surgical research. Br J Surg 2017; 104: 1753–1755. [DOI] [PubMed] [Google Scholar]
- 6. CovidSurg Collaborative . Global guidance for surgical care during the COVID‐19 pandemic. Br J Surg 2020; 10.1002/bjs.11646 [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Society of American Gastrointestinal and Endoscopic Surgeons. SAGES and EAES Recommendations Regarding Surgical Response to Covid‐19 Crisis; 2020. https://www.sages.org/recommendations‐surgical‐response‐covid‐19/ [accessed 15 April 2020].
- 8.Royal College of Surgeons. Clinical Guide to Surgical Prioritisation During the Coronavirus Pandemic; 2020. https://www.england.nhs.uk/coronavirus/wp‐content/uploads/sites/52/2020/03/C0221‐specialty‐guide‐surgical‐prioritisation‐v1.pdf [accessed 15 April 2020].
- 9.American College of Surgeons. COVID‐19 and Surgery; 2020. https://www.facs.org/covid‐19/clinical‐guidance [accessed 15 April 2020].
- 10.Peak CM, Kahn R, Grad YH, Childs LM, Li R, Lipsitch M et al. Modeling the comparative impact of individual quarantine vs. active monitoring of contacts for the mitigation of COVID‐19. MedRxiv 2020. [DOI] [PMC free article] [PubMed]


