Editor
We have recently noticed an outbreak of chilblain‐like lesions in Italy contemporarily to COVID‐19 epidemic. Due to the well‐known lockdown‐related difficulties to visit the patients, 1 we created a Google form aimed to collect information about patients presenting with these singular clinical findings. An easy to access and quick tool was chosen by the investigators in order to permit the other colleagues to spend the least amount of time, given the severe health emergency. The form was submitted through social media and email to hundreds of Italian dermatologists and paediatricians. In 5 days, we collected 63 patients through the form, but data are still going to be collected. Here the first preliminary results. No significant difference in gender was noticed (57.4% females vs 47.6% males). The median age was 14 years (IQR: 12–16). Feet alone were mostly affected (85.7%) followed by feet/hands together (7%) and hands alone (6%). Pictures of patients were uploaded in 54 patients, with 31/54 presenting with erythematous–oedematous lesions (Fig. 1) and 23/54 with blistering lesions (Fig. 2). Pain and itch were equally observed (27% vs. 27%), followed by pain/itch together shown in 20.6% of patients. Asymptomatic lesions were present in 25.4%. Median time from the onset to clinical diagnosis was 10 days (IQR: 6–15). At time of diagnosis, most patients presented active lesions, so it was not possible to establish the overall duration of the lesions. Most lesions (79.4%) were stable during the following days, 14.3% had a relapsing course, and only 6.3% were fugacious and quickly resolved. In most cases, no other cutaneous signs were observed. As concerning extracutaneous findings, gastrointestinal symptoms were the most frequently observed (11.1%) (median duration: 7 days with an IQR of 1–9), followed by respiratory symptoms (7.9%) (median duration: 7 days with an IQR of 3–10) and fever (4.8%) (median duration: 4 days, with an IQR of 3–8, 5); in most cases, systemic symptoms preceded cutaneous findings. As previously reported, due to the difficulty of execution, information about COVID‐19 status was available in a minority of cases: swab was performed in 11 patients (17.5%) and resulted positive in 2 cases (3.2%); serology was available in 6 cases (9.5%) and was positive in the 2 patients with positive swab; cohabitants with confirmed COVID‐19 infection were reported in 2 cases and not confirmed infection in 8 cases. Serology/PCR for other infections was available just in 10 patients (15.9%) and resulted positive for Mycoplasma pneumoniae in one case. History of autoimmune disorders was found in only 6 patients (one with ANA positivity), while familial or personal history of coagulation defects was seen in 4 cases. Information about other comorbidities was irrelevant except for 3 cases (Wolff‐Parkinson‐White, peripheral neuropathy, drug allergy).
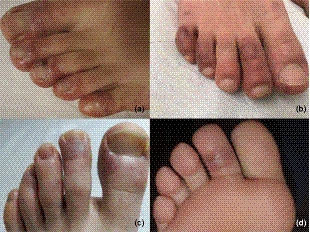
Figure 1.

Type 1 of CLL. Four different examples of erythematous oedematous lesions of the feet (a, b, c, d). (COVID swab: not performed).
Figure 2.
Type 2 of CLL. Four patients showing erythematous purpuric lesions associated with secondary blistering (a, b, c, d). (COVID swab: not performed).
These preliminary results could be useful to define the phenotype of this peculiar skin sign. The prototype of patient is an otherwise healthy adolescent with occasional history of general symptoms preceding cutaneous lesions. Painful and/or itchy long‐standing and stable lesions mostly affected toes and soles and presented with two different patterns: (i) erythematous‐oedematous type and (ii) blistering type. This appearance is quite similar to chilblains, but as there was no history of exposure to cold and no previous personal history of similar lesions, these cutaneous findings were defined as chilblain‐like lesions (CLL). While primary chilblains are notoriously due to exposure to low temperature, secondary chilblains could be associated with several diseases, such as autoimmune disorders (chilblain lupus), hematologic disorders and rarely viral infections. 2
In our study, the rate of association to autoimmune conditions was very low, allowing us to exclude a note autoimmune disorder as main cause of CLL.
The ‘epidemic’ of CLL strongly supports the hypothesis of and infectious aetiology of this particular condition. In a minority of patients, data about serology/PCR for other infections were available, with only one significant positivity for Mycoplasma serology, whose aetiological role could be matter of discussion, but unlikely. During this period, teledermatology led us to report also and increase in incidence of parvovirus B19‐like lesions (with typical location on the face, ears and hands), but according to us, these cannot be related to the CLL, because of the different clinical presentations and because of the different age of onset of the parvovirus B19 infection, that is the early school age.
As the outbreak of CLL was contemporarily observed with COVID‐19 spread in Italy, it was quite logical to hypothesize that coronavirus infection could be responsible of CLL. In our study, we collected information about patients’ COVID‐19 status: swab was performed in a minority of patients and was positive in 2 cases and serology as well. The rate of positive cohabitants or suspected familial cases was much higher. The major limit of this specific evaluation of COVID‐19 status is related to health institutions’ indications which do not support the execution of swabs in asymptomatic patients, thus making our evaluation incomplete and probably underestimated.
Although its limits related to the absence of a unique diagnostic approach to these patients, our preliminary study best fitted with emergency status and allowed us to define the clinical phenotype of CLL. As concerning aetiology, we are still far from scientifically defining CLL as a manifestation of COVID‐19, but the state of good health, the young age, the latency between mild systemic symptoms and CLL, and the morphology of cutaneous findings, could support the hypothesis of a delayed immune‐mediated reaction to the virus in genetically predisposed patients.
Conversely, the low rate of swabs and serology performed, along with the evidence of outbreak of cutaneous signs related to other notorious infections, such as Parvovirus B19 in this period (personal observation), do not permit to support this hypothesis.
In this period of world pandemic, children presenting even with only skin manifestations potentially imputable to COVID‐19 should be considered contagious until otherwise proven, as it could be important for containment strategies. Further structured molecular and serological studies are mandatory to obtain fast information about CLL in order to address patients towards the right management.
Acknowledgements
The authors thank colleagues who contributed to send cases: Alberta Bracci, Elena Lotti, Tommaso Bianconi, Elena Chiappini, Rachele Mazzantini, Carlomagno Francesco, Concetta De Ciutiis, Giuliana Rispoli, Adina Frasin, Maria di Masi, Giuseppina Mussari, Maria Riello, Cinzia Begliomini, Giuseppe Misiano, Luigi Morcaldi, Giovanna Vaccaro, Giovanna Argo, Brunella Panza, Francesco Santaniello, Franca Sergio, Bruna Tagliabue, Miriana Guarino, Sara Sandri, Claudio Ghionzoli, Vinceno Maione, Giulia Calabrese, Claudio Conforti; the patients in this manuscript have given written informed consent to the publication of their case details.
References
- 1. Piccolo V, Argenziano G. The impact of novel coronavirus on Dermatology. Dermatol Pract Concept 2020; 10: e2020049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Crowson AN, Magro CM. Idiopathic perniosis and its mimics: a clinical and histological study of 38 cases. Hum Pathol 1997; 28: 478–484. [DOI] [PubMed] [Google Scholar]


