Abstract
Aims
COVID‐19 is now a global pandemic. At the time of survey, fewer than 150 children in Australia and New Zealand had documented infection. The aim of this study was to assess attitudes, readiness and confidence in the early stages of the COVID‐19 pandemic through an online survey of paediatric physicians and sub‐specialists across Australia and New Zealand.
Methods
Multiple email list groups were used to contact paediatric physicians to undertake an online Likert scale survey between 17 and 24 March. Respondents' specialty, experience and work setting were recorded. Ordinal logistic regression was used to determine respondent factors.
Results
There were 542 respondents from across Australia and New Zealand: an estimated 11% of the paediatric physician workforce. A minority (36.6%) agreed that their national response had been well coordinated; the majority (92.7%) agreed that senior‐level hospital administrators were taking the situation seriously. Most reported a good understanding of the natural history of COVID‐19 in children, and knowledge of where to find local information. A large proportion of physicians (86.1%) were worried about becoming infected through their work; few (5.8%) reported that they would not come to work to avoid infection. Closure of school and childcares would reduce the ability to continue work at current capacity for 23.6% of respondents.
Conclusion
Despite limited experience in pandemics, most paediatric physicians felt informed. Concern about exposure at work is common; most were willing to work regardless. The closure of schools and daycares may have an impact on staffing. Coordination and leadership will be critical.
Keywords: COVID‐19, paediatric services, survey
What is already known on this topic
COVID‐19 is a rapidly expanding global pandemic.
Hospitals and health services are working rapidly to prepare for large numbers of cases.
Children with COVID‐19 tend to have milder illness and lower mortality than adults.
What this paper adds
Paediatric physicians in Australia and New Zealand feel that their own hospital administrators are taking COVID preparations seriously, but a minority of Australian paediatricians feel the national response has been well coordinated.
As a group, paediatricians feel well informed about COVID's clinical course, testing and infection control, with differences between sub‐specialty groups and physicians in different size hospitals.
Paediatricians are concerned about their own risk of infection at work, but almost all plan to continue working.
Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), a novel coronavirus, emerged in late 2019 in the Wuhan Province of China and has since rapidly spread across the globe.1 COVID‐19, the disease caused by SARS‐CoV‐2, has a wide clinical spectrum from mild upper respiratory tract illness through to severe acute respiratory distress.2 Emerging epidemiological data indicate differences in SARS‐CoV‐2 infection between children and adults. Disease course appears to be mild in the vast majority of children and asymptomatic infection has been described.3, 4 There have been very few deaths reported in children with COVID‐19.3, 4, 5 Some data also suggest children are less susceptible to acquiring SARS‐CoV‐2 infection, although reports on paediatric infection attack rates are conflicting.6, 7
With the World Health Organization declaring SARS‐CoV‐2 a pandemic on the 11 March 2020, health‐care organisations around the world have been rapidly moving to ameliorate the impending impact of COVID‐19. Specific areas of focus include instituting appropriate infection prevention strategies, workforce planning and accelerating scalable and applicable research on SARS‐CoV‐2. Similar to the SARS outbreak in 2003, health‐care workers are in a rapidly evolving environment in which personal exposure risk is balanced against professional obligation and responsibility8 although the scale of the current pandemic is unprecedented in recent history.
While COVID‐19 is well recognised to cause significant disruption across adult health‐care organisations, paediatric health‐care providers face a unique set of issues. Limited and conflicting information on SARS‐CoV‐2 transmissibility, particularly from asymptomatic children, places front line paediatricians in a position of uncertainty.9, 10 The impact of workforce shortages may be amplified in the paediatric setting, which tends to have a relatively smaller physician workforce than adult health services. Similarly, proportionally smaller numbers of paediatric hospital beds are a challenge for surge capacity planning in the paediatric setting.11
As of 22 March 2020, there were 1765 confirmed cases of COVID‐19 in Australia, including over 100 in children.12 An initial large proportion of imported cases in returned travellers have been followed by a rise in cases among household contacts and early community transmission. New Zealand has seen a similar trajectory of COVID‐19, with a smaller total number of cases.12
In this study, we aimed to explore the attitudes of Australian and New Zealand Paediatric Physicians towards COVID‐19 as institutions prepare for the impending impact of the pandemic in our region. We aimed to determine paediatric readiness and confidence in responding appropriately to COVID‐19 and to elucidate demographic factors that influence attitudes.
Methods
We conducted a survey of paediatric physicians in Australia and New Zealand. Respondents were contacted through a number of different channels; through the Australasian Society of Infectious Diseases (ASID) Paediatric special interest group, ANZPID (Australia New Zealand Paediatric Infectious Diseases), with subsequent dissemination to local hospital networks, Paed‐forum (an online mailing list of paediatricians and paediatric trainees in Australia) and through social networks. A web‐based data collection tool (Survey Monkey, Palo Alto, CA, USA) was used to collect de‐identified data over the period 17–24 March 2020. Data collected included speciality, country, size and setting (metropolitan vs. regional) of hospital, years of experience and level of training (full survey available in Appendix S1, Supporting Information). Specialties were categorised into groups: acute care (paediatric emergency, intensive care, neonatology and anaesthetics), paediatric infection diseases (ID), paediatric sub‐specialty and general paediatrics.
Five‐point Likert scale questions, with response options ranging from ‘strongly agree’ to ‘strongly disagree’, were utilised to assess respondents' agreement with statements. These were grouped into agree, neutral and disagree to improve visualisation.
Data were analysed using Excel 2013 for data collation, cleaning and descriptive statistics and Stata/IC 11.2 (Stata Corp, College Station, TX, USA) for all other statistical analyses. Ordinal logistic regression was used to determine odds ratios of factors associated with Likert responses to statements. In the regression analysis, the explanatory variables were made binary: years post qualification as a doctor (≤15 and >15 years), country (Australia vs. New Zealand), hospital size (≤150 vs. >150 beds) and hospital setting (metropolitan vs. regional). Results of this comparative analysis are expressed as raw comparison of sub‐groups and associated ordinal logistic regression odds ratios.
Ethics approval was not sought for this survey.
Results
There were 542 responses. Seventy‐four of these responses were excluded: 23 reported not being involved in paediatric care, 10 were outside of Australia and New Zealand and 41 were incomplete. Of the remaining 468 completed responses, 403 (86.1%) were from Australia, representing an estimated 14.5% of the consultant clinical paediatric workforce in Australia and 11.7% of the total paediatric work force13 There were 65 New Zealand responses, including 9.2% (39/426) of the national consultant paediatric workforce.14 Table 1 demonstrates the demographic breakdown. General paediatrics was the most common specialty (59.4%). Nearly three quarters of respondents were female (72.6%).
Table 1.
Demographics of survey respondents
| Total, n (%) | |
|---|---|
| Country | 468 |
| Australia | 403 (86.1) |
| New Zealand | 65 (13.9) |
| Speciality | |
| Acute care | 50 (10.7) |
| Infectious diseases | 19 (4.1) |
| Sub‐speciality | 120 (25.6) |
| General paediatrics | 279 (59.6) |
| Hospital setting | |
| Metropolitan | 370 (79.1) |
| Regional | 98 (20.9) |
| Inpatient beds | |
| <50 | 170 (36.3) |
| >50 but <150 | 40 (8.5) |
| >150 but <300 | 146 (31.2) |
| >300 | 112 (23.9) |
| Years post qualification | |
| <5 | 26 (5.6) |
| 5–15 | 193 (41.2) |
| 15–25 | 130 (27.8) |
| >25 | 119 (25.4) |
| RACP training level | |
| Basic | 50 (10.7) |
| Advanced | 110 (23.5) |
| Consultant or similar | 308 (65.8) |
| Gender | |
| Female | 340 (72.6) |
| Other/prefer not to say | 3 (0.6) |
Of the respondents, 36.6% (171/467) agreed that their national response has been well coordinated, while a similar percentage (35.5%, 166/467) disagreed (Fig. 1). The majority of respondents (92.7%, 432/466) agreed that senior‐level hospital administrators at their institution are taking the situation seriously. Regarding hospital preparedness, 38.6% (180/466) agreed, while 27.3% (127/466) disagreed that their institution is adequately prepared.
Figure 1.
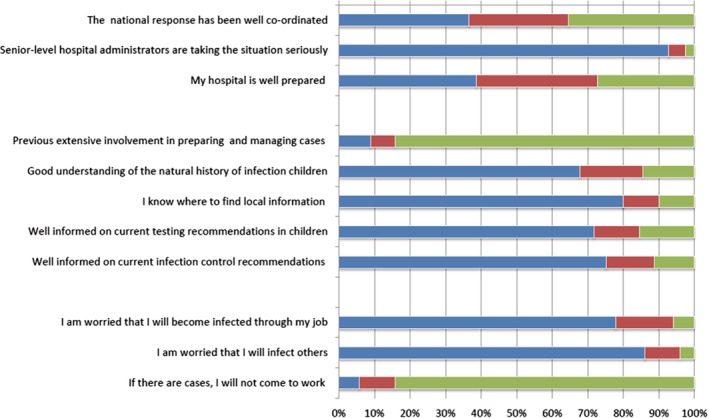
Percentage response to statements by Likert scale from agree to disagree. ( ), Agree; (
), Agree; ( ), neutral; (
), neutral; ( ), disagree.
), disagree.
A small number of respondents (9%, 42/467) agreed that they have had previous extensive involvement in preparing for and managing cases in previous outbreaks (e.g. severe acute respiratory syndrome, Middle Eastern respiratory syndrome, pandemic influenza in 2009). The majority of physicians (67.7%, 317/468) reported a good understanding of the natural history of COVID‐19 in children and knowledge of where to find local information on how to manage patients (79.9%, 373/467). Most reported being well informed on current paediatric testing (71.7%, 335/467) and infection control (75.2%, 352/468) recommendations.
A large proportion of physicians (86.1%, 402/468) are worried about becoming infected with SARS‐CoV‐2 through their work. Likewise, many are concerned about the risk of transmitting the infection to others, such as their friends and family (91.6% 428/467). Only a small portion reported that they would not come to work to avoid getting infected 6% (28/468).
Respondents were asked if they could work at the same capacity if childcare facilities and schools were closed. Of the 462 respondents to this question, 23.6% (109) reported that they would have to reduce their capacity.
Comparative sub‐group analysis
Physicians in New Zealand were more likely to agree that their national response was well coordinated compared with Australian respondents (81.5% (53/65) vs. 29.4% (118/402), odds ratio (ordinal logistic regression)[OR] 10.9, P < 0.001 (95% confidence interval (CI) 6.17–19.2)), but were less likely to agree that they were well informed on testing (52.3% (34/65) vs. 74.9% (301/402), OR 0.34, P < 0.001 (95% CI 0.20–0.58)) (Fig. 2).
Figure 2.
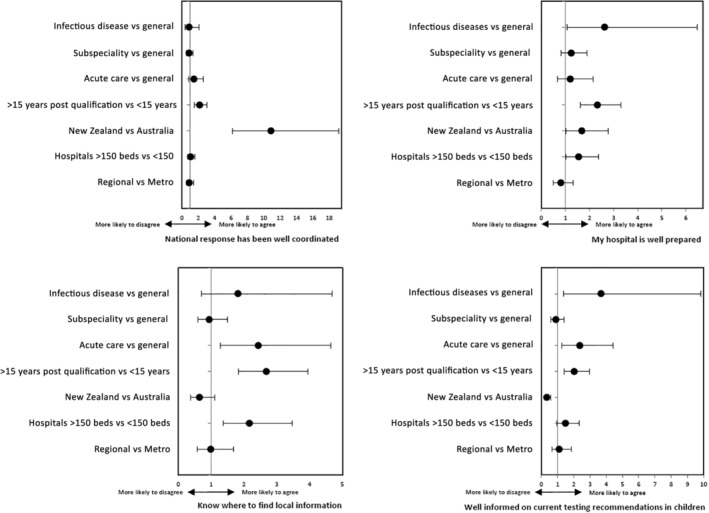
Ordinal regression analysis comparing Likert responses to key statements. A higher odds ratio in this figure indicates an increased likelihood that the sub‐group, compared with the base group, agrees with the statement. A lower odds ratio indicates an increased likelihood that the sub‐group disagrees with the statement.
The responses of physicians in speciality groups (acute care, infectious diseases and sub‐speciality) were compared with those of general paediatricians. Acute care physicians, when compared to general paediatricians, had a higher likelihood of agreeing that they are well informed on current testing (80% (40/50) vs. 69% (192/278), OR 2.37, P = 0.007 (95% CI 1.27–4.43)) and infection control practices (88% (44/50) vs. 72.4% (202/279), OR 3.23, P < 0.001 (95% CI 1.75–5.93)).
Similarly, ID physicians were more likely than general paediatricians to report being well informed on testing recommendations (84.2% (16/19) vs. 69% (192/278), OR 3.68, P = 0.009 (95% CI 1.38–9.8)) and infection control recommendations (94.7% (18/19) vs. 72.4% (202/279) OR 3.07, P = 0.02 (95% CI 1.19–7.87)), respectively. ID physicians were also more likely to report previous experience in outbreak management (63.2% (12/19) vs. 5% (14/279) OR 19.19, P < 0.001 (95% CI 7.65–48.12)).
Physicians >15 years post qualification were more likely to report previous relevant experience (14.2% (34/239) vs. 3.5% (8/228), OR 2.68, P < 0.001 (95% CI 1.82–3.95)). Similarly, they were more likely to report a good understanding of the natural history of this infection in children (77.1% (185/240) vs. 57.9% (132/228), OR 2.47, P = 0.007 (95% CI 1.7–6.63)), testing (78.2% (187/239) vs. 64.9% (148/228), OR 2.03, P < 0.000 (95% CI 1.39–2.95)) and infection control recommendations (86.6%. (207/239) vs. 70.6% (161/228) OR 1.84, P = 0.001 (95% CI 1.27–2.65)).
Compared with respondents in small hospitals, those in larger centres were more likely to agree that their hospital is well prepared (42.2% (108/256) vs. 34.3% (72/210), OR 1.55, P = 0.043 (95% CI 1.01–3.311)) and that local information was readily accessible (85.2% (219/257) vs. 73.3% (154/210), OR 2.17 P = 0.001 (95% CI 1.36–3.46)).
Research
Of the respondents, 63.9% (299/468) report that their hospital is engaged in COVID‐19 related research activities. Additional research questions were answered by 53.6% (251/468). When asked about enrolling children into treatment efficacy trials, as a hierarchy, 10.4% (26/251) would include only children with severe infection (non‐invasive ventilation or ICU level care), 41% (103/251) would include all hospitalised children, 1.6% all symptomatic children (4/251). A number were undecided (13.9, 35/251) or did not know (27.1%, 68/251). None of the above was chosen by 5 (2%) respondents.
Discussion
Since its emergence, COVID‐19 has rapidly crossed borders and placed significant strain on social and economic systems, as well as health‐care networks.15 Hospitals around Australia and New Zealand have been pushed to respond to an evolving and complex situation. Despite early data suggesting a milder course in children,3, 4 many uncertainties remain, and paediatric institutions in the region face unique challenges in meeting the needs of both patients and staff. This survey provides important context as to the perceptions of paediatricians entering the early stages of this pandemic in Australia.
Approximately one in three paediatricians felt that their national response has been well coordinated. This echoes the findings of a similar survey of infectious diseases physicians in Australia and New Zealand (under review). Recognising the inherent difficulty and need for expert leadership in directing a pandemic response, ASID,14 the representative professional body for ID physicians and clinical microbiologists in Australasia, and the Australian Medical Association16 have called for the establishment of a national coordinating body to facilitate a more rapid and coordinated response. This would help reduce confusion and duplication of effort in the development of processes and guidelines.
Although our cohort of Australian paediatric physicians expressed reservations about the national response to COVID‐19, the perception of the local response in both Australia and New Zealand is reassuring. The vast majority of respondents (92.7%) reported that their senior‐level hospital administrators were taking the situation seriously. The lower level of agreement (38.6%) that their hospital was prepared may represent the timing of this survey early in the pandemic before preparedness plans are complete. Furthermore, the ultimate impact of the pandemic in the region remains uncertain; however, the experience in Europe and Asia has seen patient demand exceed hospital capacity in many instances. The robust initial public health response in New Zealand and Australia should allow time to continue to build capacity and strengthen systems. This time period is crucial to mitigate the impact on our patients and personnel.17
Paediatric physicians report limited experience preparing for and managing a similar outbreak. Despite their limited prior experience, paediatric physicians overall state that they are well informed on the natural history of COVID‐19, and current testing and infection control recommendations. Infectious diseases physicians, acute care specialists and more senior physicians report higher levels of perceived knowledge. It is important that these groups continue to support and provide guidance to others locally and through national networks. They will be called upon to provide direction and leadership to smaller hospitals, where physicians report feeling less prepared with less knowledge on where to access local information. The ASID sub‐group, ANZPID, comprised of paediatric infectious disease specialists in Australia and New Zealand, is working to share information, including processes and guidelines, to paediatricians.
During outbreaks health‐care workers providing direct care are at risk of infection. Our data show high rates of concern about workplace exposure to COVID‐19. Despite this, paediatric physicians will continue to provide care: only a very small proportion of staff report that they would not come to work because of infection risk. It is possible that these physicians may have other risk factors for severe COVID‐19 which increase their personal susceptibility.
Public health measures can slow the spread of COVID‐19. However, certain broader measures may have unintended effects on health‐care workers and health systems. The closure of schools and day care centres would reduce the capacity of almost one in four of our respondents to work their normal hours. This, coupled with the potential of staff illness and quarantine, would be likely to have a significant impact on service delivery.
Many uncertainties exist with regard to COVID‐19 infection in children and ongoing research is essential to improve understanding of disease course, transmissibility as well as the optimal diagnostic and management approach in children. Promisingly, over 60% report that their hospital is engaged in COVID‐19 related research activities. There was no consensus as to the optimal focus and design of treatment efficacy studies in children with COVID‐19. This was not surprising given the number of unknowns. ANZPID are collaborating across centres to identify research priorities and standardise data collection in order to contribute meaningful paediatric data as the pandemic progresses.
Limitations
Non‐response bias is a limitation in conducting survey‐based data collection. It must be recognised that inherent bias present in surveys may have selected those with more interest in this outbreak, inflating the levels of reported knowledge and confidence. Despite administering the survey at the time of rapid demand on paediatric physicians to prepare their hospitals and practices for the pandemic, a significant response rate was achieved. Responses were received from a broad range of settings and locations, confirming that this survey is representative of the paediatric physicians of Australia and New Zealand, especially the portion of the denominator involved in acute hospital care.
Conclusion
This survey, undertaken at an early stage of the COVID‐19 pandemic in Australia and New Zealand with fewer than 150 infected children when conducted, highlights key strengths within our paediatric workforce. It provides important background for assessing current preparedness and ongoing response planning. Despite limited experience in pandemics and outbreaks, paediatric physicians feel well informed on testing and infection control recommendations with confidence in their hospital executives and administrators. At the same time, it is important that ANZPID continue to provide leadership and guidance. Paediatric physicians are concerned about their exposure to COVID‐19 in the workplace, and the risk that holds for themselves and their families, yet appear willing to work despite those concerns. The closure of schools and day cares may have a significant impact on staffing.
Supporting information
Appendix S1. Survey questions.
Conflict of interest: None declared.
References
- 1. World Health Organization . Coronavirus Disease (COVID‐19) Pandemic. 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [accessed 31 March 2020].
- 2. Livingston E, Bucher K. Coronavirus disease 2019 (COVID‐19) in Italy. JAMA 2020; 323: 1335. [DOI] [PubMed] [Google Scholar]
- 3. Lu X, Zhang L, Du H et al. SARS‐CoV‐2 infection in children. N. Engl. J. Med. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dong Y, Mo X, Hu Y et al. Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics 2020. [Google Scholar]
- 5. Onder G, Rezza G, Brusaferro S. Case‐fatality rate and characteristics of patients dying in relation to COVID‐19 in Italy. JAMA 2020; 10.1001/jama.2020.4683 [DOI] [PubMed] [Google Scholar]
- 6. Mizumoto K, Omori R, Nishiura H. Age specificity of cases and attack rate of novel coronavirus disease (COVID‐19). medRxiv 2020; 10.1101/2020.03.09.20033142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bi Q, Wu Y, Mei S et al. Epidemiology and transmission of COVID‐19 in Shenzhen China: Analysis of 391 cases and 1,286 of their close contacts. medRxiv 2020; 10.1101/2020.03.03.20028423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Maunder R, Hunter J, Vincent L et al. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ 2003; 168: 1245–51. [PMC free article] [PubMed] [Google Scholar]
- 9. Bai Y, Yao L, Wei T et al. Presumed asymptomatic carrier transmission of COVID‐19. JAMA 2020; 323(14): 1406–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Yu P, Zhu J, Zhang Z, Han Y, Huang L. A familial cluster of infection associated with the 2019 novel coronavirus indicating potential person‐to‐person transmission during the incubation period. J Infect Dis 2020; jiaa077. 10.1093/infdis/jiaa077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jones RP. Myths of ideal hospital size. MJA 2010; 193: 298–300. [DOI] [PubMed] [Google Scholar]
- 12. Department of Health . Coronavirus (COVID‐19) Health Report: Australian Government. 2020 Available from: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert [accessed 31 March 2020].
- 13. Australian Government Department of Health . Paediatric and Child Health 2016 Factsheet. 2016. Available from: https://hwd.health.gov.au/webapi/customer/documents/factsheets/2016/Paediatrics%20&%20child%20health%20data.pdf [accessed 31 March 2020].
- 14. Medical Council of New Zealand . Register of Doctors. 2020. Available from: https://www.mcnz.org.nz/registration/register-of-doctors?keyword=&location=&area=paediatrics&status=practising&start=40 [accessed 31 March 2020].
- 15. McCloskey B, Heymann DL. SARS to novel coronavirus–old lessons and new lessons. Epidemiol. Infect. 2020; 148: e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Australian Medical Association . Australian National Centre for Disease Control (CDC) – 2017. 2017. Available from: https://ama.com.au/position-statement/australian-national-centre-disease-control-cdc-2017 [accessed 31 March 2020].
- 17. Maunder RG, Lancee WJ, Balderson KE et al. Long‐term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis. 2006; 12: 1924–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Survey questions.


