Dear editor,
As stated by Estébanez et al., 1 incidence of dermatological affection in COVID‐19 patients may be different than reported until now.
Data and evidences are building up every day, and we wanted to add a contribution describing the case of a 67‐year‐old patient, Caucasian, with moderate obesity, a history of alcoholism and various chronic morbidities. No drug allergy was referred. She was sent to ER due to progressive dyspnoea and fever: after RT‐PCR resulted positive to SARS‐CoV‐2, she was admitted to hospital and then intubated a week later due to worsening of the respiratory condition.
Therapy included hydroxychloroquine, omeprazole, piperacillin/tazobactam and remdesivir, all interrupted after two weeks. She continued assuming potassium canrenoate and enoxaparine 4000 I.U. twice a day.
A month later, while respiratory function improved but pharyngeal swab was still positive to the virus, an erythema associated with fever’s recurrence (38.0°C) appeared.
At physical examination, we observed a moderately itching erythematous confluent rash, with undefined margins, bleaching, mostly located at the neck, trunk, back and proximal portions of upper and lower limbs (Fig. 1). The palmoplantar skin, face and mucous membranes were spared.
Figure 1.
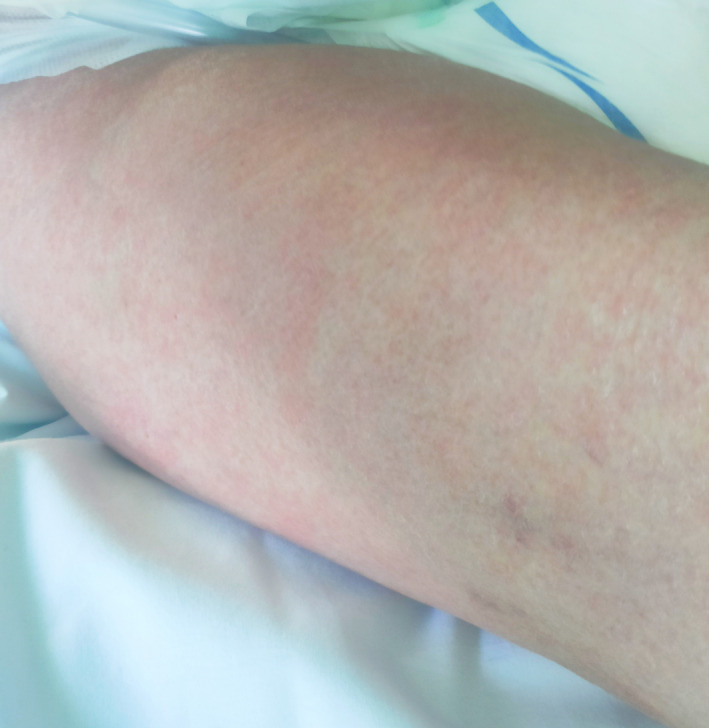
Detail of confluent exanthema on right thigh.
Due to its resembling a classical viral exanthema, a punch biopsy for histological examination was obtained from the patient’s abdomen. Haematoxylin–eosin‐stained tissue specimens showed slight superficial perivascular lymphocytic infiltrate, extremely dilated vessel in the papillary and mid dermis (Fig. 2). A week after the rash onset, our patient was newly tested through SARS‐CoV‐2 pharyngeal swab, resulted negative. Fever and rash were disappeared .
Figure 2.
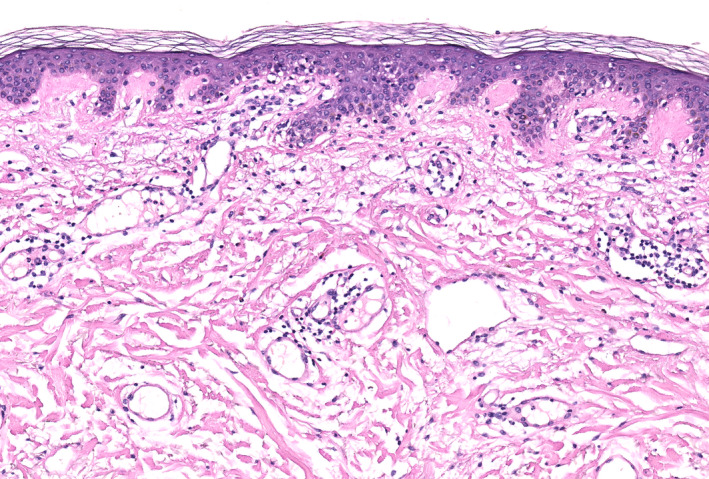
Superficial perivascular lymphocytic infiltrate, dilated vessel in the papillary and mid‐dermis. Focal spongiosis, lymphocytes along the dermoepidermal junction and vacuolar alteration were present. Cornified layer was spared. H&E 10×.
Many non‐respiratory signs and symptoms related to COVID‐19 have been reported recently. In the work by Guan et al., 2 a large number of clinical manifestations and their incidence associated with RT‐PCR‐positive patients were described, but out of 1099 subjects, only two showed some kind of unspecified cutaneous reaction. Specifically referring to skin reactions related to COVID‐19, one of the most recent papers published by Recalcati et al. describes the presence of various cutaneous affections in 18 out of 88 patients. Of these, 14 (15.9% of the total) reported having an erythematous type affection, three urticarial (3.4%) and one (1.13%) chickenpox‐like. 3 To date, indexed on MEDLINE, another two authors have reported an erythematous rash, 4 , 5 one a skin reaction with petechiae 6 and one with urticarial lesions 7 in COVID‐19 affected patients, all of them presented as onset symptoms, even though clinical images were supplied only in one case.
In our case, the clinical skin manifestation appeared after hospitalization, as described in some cases by Recalcati et al. 3 First cases of COVID‐19 arrived in our hospital at the beginning of March and from then more than 360 bed sites have been reserved for this specific patient, but until now this is the only one case associated with a cutaneous exanthema that we could observe. Our report focuses on a COVID‐19‐related rash description and is supported by clinical images and histopathological examinations. Histological examination did not show any particular signs that can make this affection different from other rashes of viral aetiology except for extremely dilated vessels in the dermis which could represent a histological diagnostic finding 8 . It should be kept in mind that skin manifestations associated with this virus could present in any form and at any time during the natural history of the disease and we have no data demonstrating a direct correlation with the prognosis of this illness. More studies of the physiopathology of the SARS‐CoV‐2 action are needed, above all regarding its interaction with endothelial cells in small vessels sites and its possible prognostic role.
Acknowledgements
The patient in this manuscript has given written informed consent to the publication of her case details.
References
- 1. Estébanez A, Pérez‐Santiago L, Silva E, Guillen‐Climent S, García‐Vázquez A, Ramón MD. Cutaneous manifestations in COVID‐ 19: a new contribution. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Guan W, Ni Z, Hu Y et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382: 1708–1720. 10.1056/nejmoa2002032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Recalcati S. Cutaneous manifestations in COVID‐ 19: a first perspective. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16387 [DOI] [PubMed] [Google Scholar]
- 4. Hunt M, Koziatek C. A case of COVID‐19 pneumonia in a young male with full body rash as a presenting symptom. Clin Pract Cases Emerg Med 2020; 4: 2. 10.5811/cpcem.2020.3.47349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mahé A, Birckel E, Krieger S, Merklen C, Bottlaender L. A distinctive skin rash associated with coronavirus disease 2019? J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Joob B, Wiwanitkit V. COVID‐19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol 2020; 82: e177. 10.1016/j.jaad.2020.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Henry D, Ackerman M, Sancelme E, Finon A, Esteve E. Urticarial eruption in COVID‐19 infection. J Eur Acad Dermatol Venereol 2020. 10.1111/jdv.16472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Singh S, Khandpur S, Arava S et al. Assessment of histopathological features of maculopapular viral exanthem and drug‐induced exanthem. J Cutan Pathol 2017; 44: 1038–1048. 10.1111/cup.13047 [DOI] [PubMed] [Google Scholar]


