Abstract
Aim
The rapid spread of the COVID‐19 pandemic has created unprecedented challenges for the medical and surgical healthcare systems. With the ongoing need for urgent and emergency colorectal surgery, including surgery for colorectal cancer, several questions pertaining to operating room (OR) utilization and techniques needed to be rapidly addressed.
Method
This manuscript discusses knowledge related to the critical considerations of patient and caregiver safety relating to personal protective equipment (PPE) and the operating room environment.
Results
During the COVID‐19 pandemic, additional personal protective equipment (PPE) may be required contingent upon local availability of COVID‐19 testing and the incidence of known COVID‐19 infection in the respective community. In addition to standard COVID‐19 PPE precautions, a negative‐pressure environment, including an OR, has been recommended, especially for the performance of aerosol‐generating procedures (AGPs). Hospital spaces ranging from patient wards to ORs to endoscopy rooms have been successfully converted from standard positive‐pressure to negative‐pressure spaces. Another important consideration is the method of surgical access; specifically, minimally invasive surgery with pneumoperitoneum is an AGP and thus must be carefully considered. Current debate centres around whether it should be avoided in patients known to be infected with SARS‐CoV‐2 or whether it can be performed under precautions with safety measures in place to minimize exposure to aerosolized virus particles. Several important lessons learned from pressurized intraperitoneal aerosolized chemotherapy procedures are demonstrated to help improve our understanding and management.
Conclusion
This paper evaluates the issues surrounding these challenges including the OR environment and AGPs which are germane to surgical practices around the world. Although there is no single universally agreed upon set of answers, we have presented what we think is a balanced cogent description of logical safe approaches to colorectal surgery during the COVID‐19 pandemic.
Keywords: Coronavirus, COVID‐19, pandemic, transmission
What does this paper add to the literature?
This paper discusses and illustrates the critically important facets of surgery during the COVID‐19 pandemic and the roles of laparoscopy and of negative pressure procedural rooms.
Introduction
The first cases of pneumonia caused by a new coronavirus, SARS‐CoV‐2, were reported in Wuhan, China, in December 2019 [1]. The disease caused by this novel virus was called COVID‐19, with its most common presentations being fever, cough, weakness and shortness of breath [1, 2]. On 11 March 2020, the infection was declared a pandemic by the World Health Organization [3]. Additional symptoms were described later, including a gastrointestinal manifestation of diarrhoea [4]. This unprecedented situation requires special considerations for surgeons dealing with abdominal surgery and, specifically, for colorectal surgeons. We will try to address herein some of those new obstacles brought on by the COVID‐19 pandemic.
First and foremost is the adequate use of personal protective equipment (PPE) as per the Centers for Disease Control (CDC) guidelines [5] and other surgical societies such as the American College of Surgeons (ACS) [6] and the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) [7]. With the current recommendations being to abstain from performing elective colorectal surgery, colorectal surgeons worldwide will still continue to operate on patients with symptomatic cancer as well as patients with perforated diverticulitis, toxic colitis and other acute problems.
The spread of the virus causing COVID‐19 is mainly through droplets and surfaces, with an aerosol transmission also suggested [8]. In order to optimize the protection of caregivers from contagious pathogens in the operating room (OR), a negative‐pressure OR has been recommended. This guideline is based upon antecedent use for other diseases including tuberculosis, measles, chickenpox, Middle East respiratory syndrome (MERS‐CoV), influenza and severe acute respiratory syndrome (SARS‐CoV). In a negative‐pressure OR, which has a lower air pressure than its surroundings, the air is allowed to flow into the room but not to escape, thus protecting personnel in adjacent areas. During the SARS outbreak in Hong Kong hospitalists and engineers demonstrated that a positive‐pressure OR can be converted to a negative‐pressure OR [9]. The recommendations of the ACS [6] and of Liang et al. [10] are for the allocation of negative‐pressure ORs for patients who are positive for COVID‐19 or suspected of having the infection. Additional emphasis should be given to the anteroom, which must also be a negative‐pressure room, preferably with a separate entrance [6]. The donning of PPE including N95 mask, cap, gloves, face and eye protection, and boot covers must be performed in the anteroom. Extubation is extremely dangerous for viral spread and therefore should be performed either in the negative‐pressure OR or in a dedicated anaesthesia recovery room, as recommended by Ti et al. [11]. The negative‐pressure OR and anteroom should ideally be in a corner of the OR complex with separate access and egress. In addition, regardless of whether the OR is positive pressure, negative pressure or neutral pressure, all personnel other than the anaesthesiologist should leave the room during both intubation and extubation. Based upon our review of the available data, we strongly recommend that every hospital in which COVID‐19 patients are treated should try to have at least one dedicated negative‐pressure OR, preferably in the corner of the OR complex.
Similar recommendations pertain to endoscopy suites to include a negative‐pressure endoscopy room for patients with COVID‐19 [12, 13]. To minimize the exposure of caregivers, endoscopic procedures should not be performed in the office due to the lack of an appropriate environment and PPE.
There are some lessons about safety in the OR during minimally invasive surgery (MIS) that we can learn from the 10 years of experience with pressurized intraperitoneal aerosolized chemotherapy (PIPAC) [14]. Although PIPAC is not universally available, its mechanism allows important parallels to be drawn in relation to laparoscopy in the COVID‐19 era. Specifically, the PIPAC system must be safely hermetically sealed to prevent inadvertent escape of any of the intraperitoneal gas or fluid which contains chemotherapeutic agents. During standard laparoscopy inadvertent pneumoperitoneum leakage is not dangerous, and in fact is sometimes deliberately undertaken to evacuate smoke from the abdominal cavity. PIPAC is a laparoscopic procedure for delivering chemotherapeutic agents as an aerosol to treat advanced peritoneal metastases with a palliative or neoadjuvant intent [15, 16]. Therefore, during PIPAC, even miniscule leaks must be assiduously avoided. Active replication of the SARS‐CoV‐2 virus has been proved to occur in the respiratory and gastrointestinal tracts [17, 18]. Therefore, during digestive surgery the potential danger for aerosol transmission has been noted despite the fact that isolation of SARS‐CoV‐2 in aerosol from pneumoperitoneum has not been reported. A passive evacuation system using the electrostatic filter from ventilator machines has been proposed [19]. We present validated occupational health safety measures which meet the US National Institute for Occupational Safety and Health (NIOHS) standards and were implemented to protect healthcare workers from accidental exposure to toxic aerosols during PIPAC procedures [14, 20, 21, 22]. By analogy, some of these measures could be implemented during laparoscopic surgery in COVID‐19 patients. These protective measures include:
The required amount of abdominal distension is achieved by reducing the number of trocars to a minimum (in general two) by the use of balloon trocars such as Kii® (Applied Medical, Ranch Santa Margarita, California, USA) and by verifying zero gas flow on the panel of the CO2 insufflator. Since some insufflators are able to reabsorb CO2 in order to prevent intra‐abdominal pressure peaks, a microparticle filter should be intercalated on the CO2 inflow line between the insufflator and the patient.
Desufflation of the toxic aerosols occurs over a so‐called closed aerosol waste system (CAWS), consisting of hermetic tubing with two consecutive microparticle filters. The CAWS is then connected to a mobile high‐efficiency particulate air (HEPA) filter (Buffalo Filter Systems Inc., Lancaster, New York, USA).
As an additional safety measure, the patient is completely covered with a large plastic drape extending to the floor [23]. The plastic drape is perforated and a stoma bag is sealed to the orifice and connected with hermetic tubing going from the bag to a mobile HEPA filter system, as shown in Fig. 1.
Figure 1.
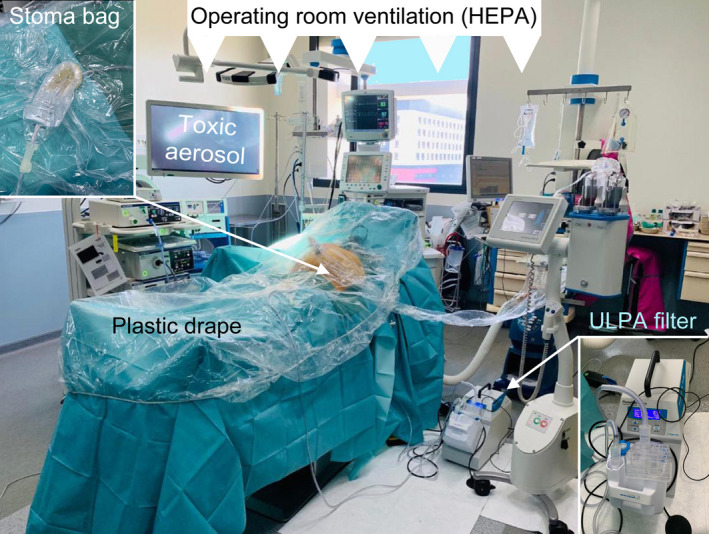
Safety measures in the operating room during laparoscopic surgery in COVID‐19 patients. Courtesy of Clarisse Eveno, MD, PhD, Lille, France.
The use of an active smoke evacuator connected to a proper filter has been recommended by SAGES for laparoscopic or robotic procedures during the COVID‐19 pandemic [24]. Another innovative suggestion for additional safety is the addition of a system of intra‐abdominal electrostatic precipitation, [25, 26] which is able to sediment the aerosolized virus to the peritoneum, thereby precipitating 99.7% of the particles (Fig. 2).
Figure 2.
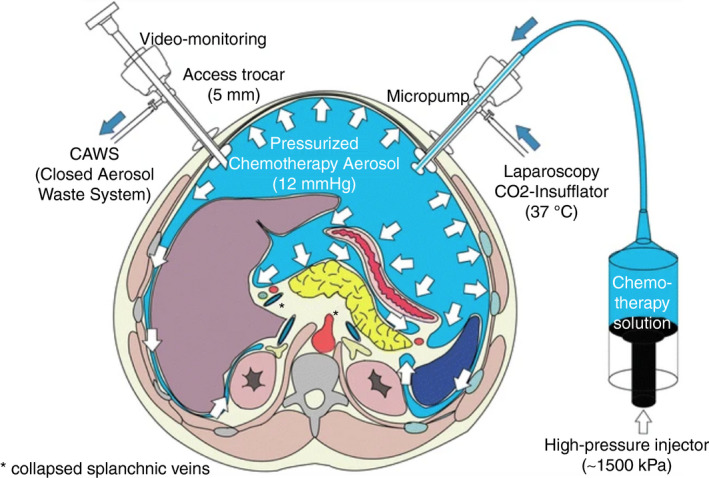
Pressurized intraperitoneal aerosol chemotherapy (PIPAC) from Solass et al. [36]. Open Access: This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Although modern ventilation systems are highly effective in purifying the air in the OR, their filters are not able to capture nanoparticles with a diameter of less than 1 µm, such as SARS‐CoV‐2 which has with a diameter of 60–140 nm [27]. However, viruses are usually transported within aerosols, and the droplets that make up the aerosol will be almost completely removed by the HEPA filters. Typically, the air is completely exchanged every 2.5–4 min, depending on the size of the OR and the performance of the ventilation system.
The decision on the modality of surgical access will be contingent upon local factors, including both the COVID‐19 status of the patient and the availability of laparoscopic instrumentation. The former assessment is in turn reliant upon the local availability of testing. While some authors have suggested that it is potentially safer to perform a closed, controlled procedure than to have an open abdomen with fluids and smoke able to spread widely, others have stated that it is safer to avoid laparoscopy because of the risk of viral spread in the pneumoperitoneum. These issues are further discussed below.
Finally, it is important to note that typical modern ventilation systems utilize purified air from the ceiling and aspirate contaminated air close to the floor. Thus, aerosols contaminated with the SARS‐CoV‐2 virus are directed to the floor, then to the lateral walls and corners of the OR [28]. Smoke simulations during PIPAC procedures have demonstrated that the safest place for surgeons and nurses is in the centre of the OR. To minimize the risk of exposure to toxic aerosols, OR personnel should not bend to the floor, sit on the floor or stay close to the walls due to capillarity effects (see Video S1 in the online Supporting Information, courtesy of Dr Marc Reynard). Recommendations for use of negative‐pressure environments throughout the hospital continue to evolve, as do suggestions for converting positive‐pressure areas to negative‐pressure ones [29, 30].
Whereas application of the measures above can be assumed to reduce the risk of contamination of surgeons by aerosolized SARS‐CoV‐2 virus particles, they are unlikely to provide complete protection against infection. Thus, during laparoscopic procedures on patients with COVID‐19, surgeons should be equipped with masks with a microparticle filter (FPP2 or FPP3).
Minimally invasive surgery has gained widespread popularity; however, concerns about active virus particles in the pneumoperitoneum have been raised. Previous studies have demonstrated particles from papillomavirus, HIV and some other viruses [31, 32] and it is unclear whether SARS‐CoV‐2 shares the same properties. However, one needs to assume that SARS‐CoV‐2 particles are also released during laparoscopy with CO2. SAGES recommends that the use of devices to filter released CO2 for aerosolized particles is considered [7]. Zheng et al. [33] advised caution with MIS, limiting the intra‐abdominal pressure, reducing the electrocautery settings and minimizing the Trendelenburg position. In many centres, a high‐flow insufflator is used for MIS procedures. Based upon our assessment of the evidence, laparoscopy may be performed in patients who are negative for SARS‐CoV‐2 in whom urgent or emergency indications necessitate the performance of surgery during the pandemic. However, appropriate caution must be exercised, as outlined in the above references. In many parts of the world, the requisite laparoscopic equipment safeguards may not be available. If the surgeon cannot access the recommended precautionary tools, such as airtight ports and filters, it may be safer to offer laparotomy using full PPE. However, even during laparotomy, great care must be taken to ensure complete immediate evacuation of all diathermy/electrocautery smoke plumes. Thus, the negative‐pressure OR again shows its value in helping achieve this safety goal. In addition, the availability of PPE has been challenging and may be exacerbated by both the regional incidence of COVID‐19 and the rate of infection as well as by institutional and governmental financial resources. To meet this challenge, numerous guidelines have been issued by the CDC, the National Institutes of Health and many societies including SAGES on the safe reuse of PPE [5, 7, 34, 35]. Ultimately, the decisions on availability and conservation of PPE are made at a local level using the various published guidelines as resources.
Within the realm of colorectal surgery, high‐flow insufflation is an integral component of transanal total mesorectal excision (TaTME). While high‐flow insufflation facilitates gas evacuation during laparoscopy and is instrumental in establishing pneumorectum in TaTME, its benefits are also potential disadvantages. The higher flow and gas evacuation capabilities potentially increase the surgeon’s exposure to aerosolized viral particles. Until further evidence is produced, it seems prudent to avoid TaTME during the COVID‐19 pandemic.
The European Association for Endoscopic Surgery (EAES) Technology Committee reported that standard electrostatic filters used for ventilation machines are effective in evacuating the generated smoke and filtering the potential viral load [19]. This filter can be connected via standard tubing to the trocar evacuation port. Another commercial product that was approved by the US Food and Drug Administration (FDA) is the UltravisionTM (Alesi Surgical, Cardiff, UK) [24]. This may be used as an adjunct to significantly decrease the concentration of aerosolized particulates in the CO2 gas during laparoscopic procedures by the method of electrostatic precipitation.
We do not have clear solutions to all of the above problems. Furthermore, the solutions will vary contingent upon local resources, guidelines and COVID‐19 incidence. However, we believe that with prudent leadership these issues can be dealt with in a thoughtful and adequate manner. This initiative will be undertaken on national, international and institutional levels. Furthermore, local governance groups will need to decide which of the rapidly expanding myriad of guidelines from professional societies and organizations and from governmental bodies they should follow. Ultimately, in adopting and adhering to these guidelines the local institution must consider its COVID‐19 testing capabilities, laparoscopic resources and availability of PPE. Thus, the publication of a plethora of guidelines may be helpful given the disparities in resource availability around the world [6, 7]. As with every crisis, along with many hardships there are also numerous opportunities to improve our professional knowledge, technique and, perhaps, the most important aspect of our calling as surgeons, which is solidarity and help to both our peers and patients.
Funding
None.
Conflicts of interests
SDW: royalties and consulting fees from Karl Storz Endoscopy, Intuitive Surgical and Covidien; consulting fees from Stryker, Regentys and Takeda. DCG, GH and IK: none. MAR: royalties and shares from Capnomed GmbH.
Supporting information
Video S1. Demonstration of flow direction for aerosolized particles in a laminar airflow operating room.
References
- 1. World Health Organization . Pneumonia of Unknown Cause‐ China (2020). Available at: https://www.who.int/csr/don/05‐january‐2020‐pneumoniaof‐unknown‐cause‐china/en/ (accessed 3 April 2020). [Google Scholar]
- 2. Chan Jasper FW, Yuan SF, Kok KH et al. novel coronavirus indicating person to person transmission: a study of a family cluster. Lancet 2019; 395: 514–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. https://www.who.int/dg/speeches/detail/who‐directorgeneral‐s‐opening‐remarks‐at‐the‐media‐briefing‐on‐covid‐19. (11‐March‐2020).
- 4. Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID‐19 and the possibility of faecal transmission. Aliment Pharmacol Ther 2020; 51(9): 843–51. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. https://www.cdc.gov/coronavirus/2019‐ncov/healthcare‐facilities/guidance‐hcf.html (accessed 3 April 2020).
- 6. https://www.facs.org/covid‐19/clinical‐guidance (accessed 3 April 2020).
- 7. https://www.sages.org/recommendations‐surgical‐response‐covid‐19/ (accessed 3 April 2020).
- 8. Li Q, Guan X, Wu P et al. Early Transmission dynamics in Wuhan, China, of novel Coronavirus‐infected pneumonia. N Engl J Med 2020; 382: 1199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chow TT, Kwan A, Lin Z, Bai W. Conversion of operating theatre from positive to negative pressure environment. J Hosp Infec 2006; 64: 371–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. https://www.alnap.org/help‐library/handbook‐of‐covid‐19‐prevention‐and‐treatment (accessed 3 April 2020).
- 11. Ti LK, Ang LS, Foong TW, Ng BSW. What we do when a COVID‐19 patient needs an operation: operating room preparation and guidance. Can J Anaesth 2020; 67: 756–8. 10.1007/s12630-020-01617-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Repici A, Maselli R, Colombo M et al. Coronavirus (COVID‐19) outbreak: what the department of endoscopy should know. Gastrointest Endosc 2020, pii: S0016–5107(20)30245–5. [epub ahead of print]. 10.1016/j.gie.2020.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. https://www.asge.org/home/joint‐gi‐society‐message‐covid‐19 (accessed 3 April 2020).
- 14. Solass W, Giger‐Pabst U, Zieren J, Reymond MA. Pressurized intraperitoneal aerosol chemotherapy (PIPAC): occupational health and safety aspects. Ann Surg Oncol 2013; 20: 3504–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Odendahl K, Solass W, Demtröder C et al. Quality of life of patients with end‐stage peritoneal metastasis treated with Pressurized IntraPeritoneal Aerosol Chemotherapy (PIPAC). Eur J Surg Oncol 2015; 41: 1379–85. [DOI] [PubMed] [Google Scholar]
- 16. Alyami M, Hübner M, Grass F et al. Pressurised intraperitoneal aerosol chemotherapy: rationale, evidence, and potential indications. Lancet Oncol 2019; 20: e368–77. [DOI] [PubMed] [Google Scholar]
- 17. Wölfel R, Corman VM, Guggemos W et al. Virological assessment of hospitalized patients with COVID‐2019. Nature 2020; 1–10. [epub ahead of print]. 10.1038/s41586-020-2196 [DOI] [PubMed] [Google Scholar]
- 18. Xiao F, Tang M, Zheng X et al. Evidence for gastrointestinal infection of SARS‐CoV‐2. Gastroenterology 2020; 158: 1831–3 (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Mintz Y, Arezzo A, Boni L et al. A low cost, safe and effective method for smoke evacuation in laparoscopic surgery for suspected coronavirus patients. Ann Surg 2020. (in press). 10.1097/SLA.0000000000003965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Robella M, Vaira M, De Simone M. (Safety and feasibility of pressurized intraperitoneal aerosol chemotherapy (PIPAC) associated with systemic chemotherapy: an innovative approach to treat peritoneal carcinomatosis. World J Surg Oncol 2016; 14: 128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Graversen M, Pedersen PB, Mortensen MB. Environmental safety during the administration of Pressurized IntraPeritoneal Aerosol Chemotherapy (PIPAC). Pleura Peritoneum 2016; 1: 203–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Cazauran JB, Alyami M, Lasseur A, Gybels I, Glehen O, Bakrin N. Pressurized intraperitoneal aerosol chemotherapy (PIPAC) procedure for non‐resectable peritoneal carcinomatosis (with video). J Gastrointest Surg 2018; 22: 374–5. [DOI] [PubMed] [Google Scholar]
- 23. Seitenfus R, Kalil AN, de Barros ED, Fedrizzi G. Pressurized intraperitoneal aerosol chemotherapy (PIPAC) through a single port: alternative delivery for the control of peritoneal metastases. Rev Col Bras Cir 2018; 45: e1909. [DOI] [PubMed] [Google Scholar]
- 24. https://www.sages.org/wp‐content/uploads/2020/03/Ultravision‐as‐an‐adjunct.pdf (accessed 3 April 2020).
- 25. Ladhani L, Pardon G, Meeuws H et al. Sampling and detection of airborne influenza virus towards point‐of‐care applications. PLoS One 2017; 12: e0174314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kettleson EM, Ramaswami B, Hogan CJ Jr et al. Airborne virus capture and inactivation by an electrostatic particle collector. Environ Sci Technol 2009; 43: 5940–6. [DOI] [PubMed] [Google Scholar]
- 27. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R Features, Evaluation and Treatment Coronavirus (COVID‐19). Treasure Island, FL: StatPearls; [Internet], Last Update: March 20, 2020. [Google Scholar]
- 28. Sadrizadeh S, Holmberg S. Surgical clothing systems in laminar airflow operating room: a numerical assessment. J Infect Public Health 2014; 7: 508–16. [DOI] [PubMed] [Google Scholar]
- 29. https://www.sciencedaily.com/releases/2017/07/170726091518.htm (accessed 3 April 2020).
- 30. https://www.ncbi.nlm.nih.gov/pubmed/15573039 (accessed 3 April 2020).
- 31. Hensman C. Chemical composition of smoke produced by high‐frequency electrosurgery in a closed gaseous environment. Surg Endosc 1998; 12: 1017–9. [DOI] [PubMed] [Google Scholar]
- 32. Gloster HM, Roenigk RK. Risk of acquiring human papillomavirus from the plume produced by the carbon dioxide laser in the treatment of warts. J Am Acad Dermatol 1995; 32: 436–41. [DOI] [PubMed] [Google Scholar]
- 33. Zheng MH, Boni L, Fingerhut A. Minimally invasive surgery and the novel coronavirus outbreak: lessons learned in China and Italy. Ann Surg 2020: 1. [published online ahead of print]. 10.1097/SLA.0000000000003924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. https://www.cdc.gov/niosh/npptl/topics/respirators/disp_part/default.html (accessed 3 April 2020).
- 35. https://www.asahq.org/about‐asa/newsroom/news‐releases/2020/03/update‐the‐use‐of‐personal‐protective‐equipment‐by‐anesthesia‐professionals‐during‐the‐covid‐19‐pandemic (accessed 3 April 2020).
- 36. Solass WMD, Kerb R, Mürdter T et al. Intraperitoneal chemotherapy of peritoneal carcinomatosis using pressurized aerosol as an alternative to liquid solution: first evidence for efficacy. Ann Surg Oncology. 2014; 21: 553–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Video S1. Demonstration of flow direction for aerosolized particles in a laminar airflow operating room.


