Abstract
Coronavirus disease 2019 (COVID‐19) had its evolution in Wuhan, Hubei Province, China, and now it has spread around the world, resulting in a large number of deaths. Temporary Ark hospitals (TAHs) have played an important role in controlling the spread of the epidemic in the city of Wuhan. Taking one TAH with 800 beds as an example, we summarized details of the layout, setting, working mode of medical staff, patient management, admission standards, discharge standards, and standards for transferring to another hospital, hospital operation, and so on. Over the period of operation, a total of 1124 patients were admitted for treatment. Of these, 833 patients were cured and discharged from the hospital and 291 patients were transferred to other designated hospitals, owing to aggravation of their condition. The achievement was to have zero infection for medical staff, zero in‐hospital deaths among admitted patients, and zero readmission for discharged patients. The rapid deployment of TAH provided a suitable place for treating mild/moderate or no asymptomatic COVID‐19 patients, which successfully helped to control the infection in Wuhan. The successful model of TAH would rapidly and effectively control the spread of COVID‐19 in other cities.
Keywords: control, COVID‐19, Temporary Ark Hospital, Wuhan
Highlights
Temporary Ark hospitals (TAHs) have played an important role in controlling the spread of the epidemic in the city of Wuhan. We described in detail how one TAH works. Zero infection for medical staff, zero in‐hospital deaths among admitted patients, and zero readmission for discharged patients in our TAH. The successful model of TAH would rapidly and effectively control the spread of COVID‐19 in other cities.
1. INTRODUCTION
Since December 2019, an ongoing outbreak of novel coronavirus in Wuhan, Hubei Province, China, has infected a large number of patients, resulting in many deaths. 1 This novel coronavirus was subsequently isolated by Chinese scientists and named severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), which caused coronavirus disease 2019 (COVID‐19). 2 Although COVID‐19 has been effectively controlled in Wuhan, it has spread to more than 200 other countries. On 11 March 2020, World Health Organization (WHO) announced that the current COVID‐19 epidemic could be called a global pandemic according to an assessment. 3 By 27 March 2020, more than 509 164 COVID‐19 patients had been diagnosed in the world, with more than 23 335 deaths, according to WHO COVID‐19 situation reports (https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports).
Wuhan is a metropolis with a population of 10 million. In early February 2020, designated hospitals that were limited in terms of medical resources could not admit all COVID‐19 patients in Wuhan. Meanwhile, nearly 80% of COVID‐19 patients display no symptoms or only mild symptoms, 1 , 4 and these mild COVID‐19 patients may develop into severe or even critically ill patients due to inadequate clinical care, which can cause more shortage of medical resources and worse quality of patient care. Most important, although these COVID‐19 patients comply with home quarantine, it can also lead to the spread of the illness among family members and even in the community. 5 , 6 To effectively control the development of the epidemic, the city of Wuhan took many effective measures. On 3 February 2020, the government of Wuhan decided to establish a number of COVID‐19 Temporary Ark Hospitals (TAHs) in the hope of admitting all asymptomatic or mildly symptomatic COVID‐19 patients, thus ameliorating the serious dilemma in Wuhan. TAHs are a part of the army's mobile field medical system, which is widely used in various emergency situations including natural disasters, wars, and epidemics. 7 Traditional mobile hospitals comprise a medical treatment ward and a technical support area. They include modular sanitary equipment, emergency treatment, surgical treatment, and clinical testing abilities, as well as other functionalities. However, the Wuhan TAHs were different from traditional mobile hospitals. 8 The Wuhan TAHs were constructed using the city's sports stadium, convention centers, and abandoned buildings, offering nearly 20 000 beds for the treatment of COVID‐19 patients with no or mild symptoms.
Here, we describe the experiences from one of our TAHs, Wuchang Temporary Ark Hospital (WTAH), which was constructed using a sports stadium. As the first establishment and the last retirement of COVID‐19 TAH, the experience in construction and management of WTAH has been replicated numerous times by other TAHs and has been proven to be successful. We aim to share our experiences, hoping to provide insights and strategies to conquer this deadly disease in other countries.
2. AIM OF THE WTAH
The main purpose of the WTAH was to isolate COVID‐19 patients, isolate the source of infection, prevent family transmission of infections caused by home isolation, prevent contamination of the environment caused by repeated hospital trips, and reduce staff member infection. Under the circumstance in which the existing medical resources in Wuhan were already saturated, the WTAH allowed patients with mild or moderate illness to receive basic medical assistance, to prevent aggravation of the illness, and further isolated sources of viral shedding.
3. SITE SETTING
The WTAH was divided into three areas (A, B, and C) with the same configuration, and it could admit about 800 patients at its maximal capacity. Areas A and C had 250 beds, respectively, and area B had 300 beds. The medical teams of WTAH were a combination of the national emergency teams and Wuhan local medical teams. The Renmin Hospital of Wuhan University team served as the leading clinical team. Our medical team was responsible for Area C, which included three zones (clean zone, semicontaminated zone, and contaminated zone) and three channels (medical staff channel, new/transfer patient channel, discharged patient channel). The clean zone was mainly responsible for office area, which included medical department, nursing department, administrative office, infection control department, and material support department to ensure stable operations in our hospital. The semicontaminated zone was composed of buffer area, entrance, and exit. The contaminated zone included isolation ward, nurses' station, pharmacy, doctor's office, recreation room, storeroom, emergency room, shower room, toilet, mobile computed tomography (CT) vehicle, mobile P3 inspection vehicle, ambulance and triage. The detailed site setting is shown in Figure 1.
Figure 1.
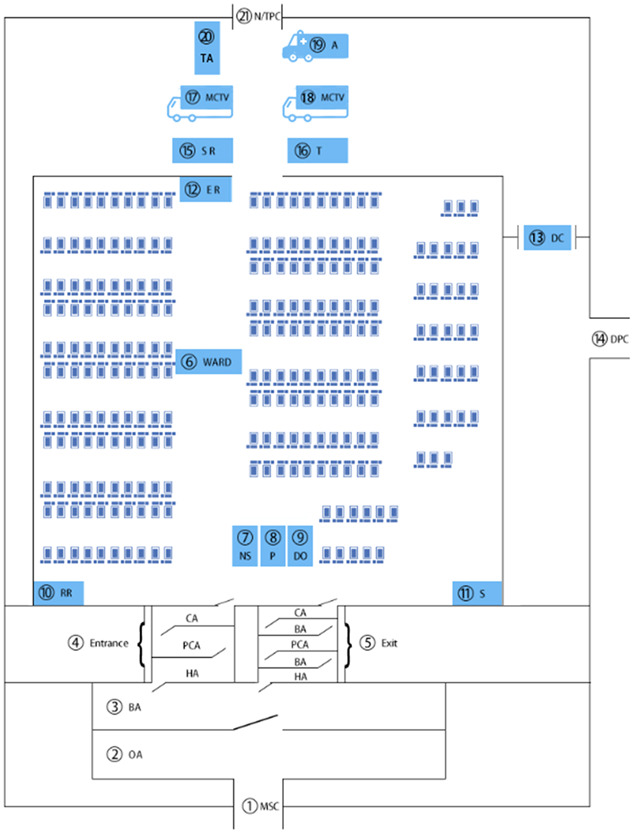
A schematic diagram of medical unit layout in the temporary ark hospital. (1) MSC, medical staff channel; (2) OA, office area, including clinical care, nursing, administrative office, infection control, and supply chain to ensure stable operations in the hospital; (3) BA, buffer area; (4) Entrance; CA, contaminated area; PCA, potential contaminated area; HA, hygienic area; (5) exit; (6) ward; (7) NS, nurses' station; (8) P, pharmacy; (9) DO, doctor's office; (10) RR, recreation room; (11) S, storeroom; (12) ER, emergency room; (13) DC, disinfection channel; (14) DPC, discharged patient channel; (15) SR, shower room; (16) T, toilet; (17) MCTV, mobile computed tomography vehicle; (18) MP3IV, mobile P3 inspection vehicle; (19) A, ambulance; (20) TA, triage; (21) N/TPC, new/transfer patient channel
4. DOCTORS AND NURSES
Area C had a total of 250 beds grouped into various 20 to 30‐bed medical units, and each unit was equipped with a minimum of two doctors and six nurses. Area C has 25 doctors and 80 nurses, and 5 doctors and 8 nurses who were responsible for communicating with medical staff in the ward regularly worked in office area, and 20 doctors and 72 nurses took turns to work in the ward.
5. MEDICINE AND EQUIPMENT
Patient therapy combined Western and traditional Chinese medicines with established expert consultation procedures. Only oral medication was routinely provided to patients in the COVID‐19 hospital. In an emergency, first aid drugs were administered intravenously. The drugs available in our area included antibiotics, antivirals, antipyretic and analgesic drugs, antihypertensive drugs, antidiarrheal drugs, hypoglycemic drugs, hormones, first aid drugs, and traditional Chinese medicines. The details are described in Table S1.
Equipment in our area included thermometers, sphygmomanometers, pulse oximeter finger clips, glucometers, ECG monitors, and oxygen cylinders. The WTAH was also equipped with a mobile CT vehicle, a mobile P3 vehicle for nucleic acid test, routine blood analyzer, ECG machine, ambulance, and defibrillator.
6. PATIENT MANAGEMENT
The first inclusion criterion for admission to the WTAH was as follows: a patient diagnosed with mild COVID‐19 and/or a patient with no symptoms according to the diagnosis and treatment guidelines of the National Health and Fitness Commission. 9 The guidelines for mild COVID‐19 stipulate mild clinical symptoms and no pulmonary imaging changes (no signs of pneumonia, no multiple small plaque shadow and interstitial changes, no multiple ground glass shadow or infiltration shadow, and no lung consolidation in both lungs). Typical patients developed fever, respiratory symptoms, and other symptoms, but presented mild imaging manifestations. Other inclusion criteria included the following: age between 18 and 65 years, ability to take care of oneself, with no serious respiratory, cardiovascular, or other basic diseases or mental illnesses. Additionally, the patient's influenza virus nucleic acid test must be negative.
The COVID‐19 patients confirmed by the hospital's outpatient department in the early stage of their illness could not be directly admitted to the main hospital in Wuhan. The COVID‐19 patients in the TAH mainly came from the community and were transferred by ambulance. For entering WTAH, the patients only needed to carry personal daily necessities, medical records, and documents; the WTAH would provide food and common daily necessities. After the patients were transferred to the WTAH, the first step was meeting a doctor in the triage, who conducted a simple assessment of their condition and recorded information. The patients who met the admission criteria were then sent into the ward. After the patient admission, the second step included an additional detailed assessment by medical staff in the ward. According to the patient's symptoms, lab examination, and CT chest results, some patients were transferred to a designated hospital for further treatment. Other patients were kept in the ward on the basis of the detailed evaluation. Oral medication and other medical examinations were given according to the patient's medical status, and the patient's condition was closely observed.
Health workers used disinfectants, twice in the morning and evening, to scrub and disinfect the floor, beds, tables and chairs, doctors' offices, nurses' stations, recreation rooms, and other public areas of the ward, and they disposed of the patients' household garbage timely, keeping the ward tidy. The spacing between beds was kept at a minimum of 1.2 m. Patients had to wear surgical masks. When patients were admitted into the hospital, they were instructed to cover their mouth and nose with a tissue or with their elbow when coughing or sneezing, wash hands with flowing water after contact with respiratory secretions, and use a quick hand disinfectant for hand sanitization when there was no visible contamination on the hands.
7. PHYSICIAN WORKING PROCEDURES
Every day, our area had to serve more than 200 patients, placing a heavy work burden on doctors and nurses; therefore, a good workflow helped to reduce the work burden, save human resources, protect the safety of health care workers, and provide better quality of patient care. In our area, the doctors were subdivided into doctors outside the ward and doctors inside the ward. Doctors outside the ward worked according to an 8‐hour rotation system, and doctors inside the ward worked according to a 4‐hour rotation system (Figure 2). The doctors outside the ward were responsible for issuing doctor's orders, preparing patient medical records, and coordinating information exchange between the doctors inside the ward and the headquarters. In the buffer region, doctors had to wear medical protective masks (N95 or above), disposable medical cap, eye/face shields (anti‐fog), protective clothing, disposable gloves, and disposable shoe covers, in accordance with the two‐level protective standards, before crossing the personnel passage into the ward. The doctors in the ward included three resident doctors and two attending physicians for ward rounds every morning, and two resident doctors were on duty during the other periods to treat patients during the shift. The morning ward rounds focused on the newly admitted patients and key special patients, and changes in each patient's condition and medication status were recorded. After the ward rounds were completed, the doctor in the ward would decide whether the patient should continue to be treated at the WTAH, be discharged home, or be transferred to the corresponding designated hospital for further treatment. The information obtained inside the ward was sent to the doctors outside the ward via a mobile phone. The doctors outside the ward issued electronic examination requests and oral medication orders. If there was a patient transfer, the doctor would inform the headquarters to contact the transfer personnel; if there was a discharge, the headquarters would contact the designated person to pick up the patient, and the discharged patient and personal belongings must be disinfected before leaving the WTAH. Medical documents in the modular setting only recorded the patients' special changes, which sped up the work progress and saved human resources. Doctors on duty had at least 24 hours of rest between shifts. All doctors met once a week to discuss the difficulties they faced in their work in the past week and the problems they had to solve; they proposed solutions and continuously optimized the current work procedures.
Figure 2.
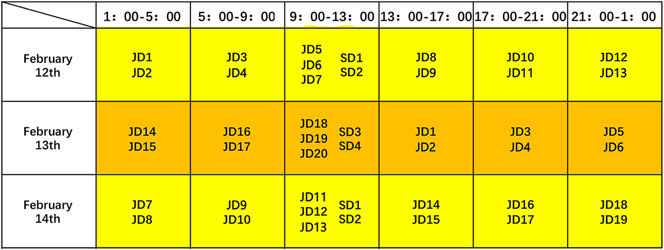
The physician duty schedule. This graph depicts three consecutive days of physician duty. JD, junior doctor; SD, senior doctor
8. NURSE WORKING PROCEDURES
The nurses were also divided into two groups: the nurses outside the ward and the nurses inside the ward. The nurses outside the ward were replaced every 8 hours, whereas the nurses inside the ward were replaced every 4 hours (Figure 3). The nurses outside the ward were responsible for carrying out the doctor's orders, printing the application forms for medical examination, and preparing the drugs, which were then brought into the ward by the nurses inside. In the buffer region, nurses had to wear medical protective masks (N95 or above), disposable medical cap, eye/face shields (anti‐fog), protective clothing, disposable gloves, and disposable shoe covers, in accordance with the two‐level protective standards, before crossing the personnel passage into the ward. Each shift was assigned nine nurses, including one head nurse and eight others, each responsible for about 30 patients. The nurses' job mainly included measuring the patients' vital signs, including temperature, pulse, blood pressure, and oxygen saturation, carrying out the doctor's orders, such as distributing examination application forms and drugs. The nurses also distributed three meals daily to the patients and helped patients solve difficulties and provided simple psychological counseling.
Figure 3.
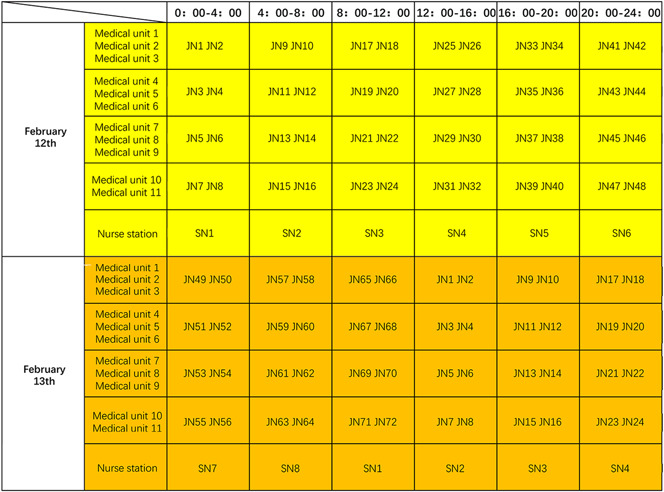
A nurse duty schedule. This graph depicts two consecutive days of nurse duty. JN, junior nurse; SN, senor nurse
9. TRANSFER AND DISCHARGE PROCEDURES OF THE TAH
9.1. Transferring to a designated hospital
COVID‐19 patients who progressed to a severe or critical condition were transferred to a designated hospital. Some patients did not progress or improve significantly, but they were accompanied by other diseases (chronic diseases worsen), which necessitated transfer to the main hospital.
According to the guidelines, a COVID‐19 patient is considered of severe type if any of the following is present: dyspnea with respiratory rate greater than or equal to 30/min, SpO2 < 93% in a resting state, PaO2/FiO2 < 300mm Hg, and lung infiltrates greater than 50% within 24‐48 hours.
According to the guidelines, COVID‐19 patients are considered of critical type if they have any of the following conditions, including mechanical ventilation, shock, other organ failure, and hospitalization in the intensive care unit.
9.2. Discharge standard
For patients with COVID‐19‐related symptoms, the hospital stay was greater than 14 days, and symptoms could not be present for more than 3 days. For patients without COVID‐19‐related symptoms, the history of close contact with positive patients must have been greater than 14 days. In addition, patients were discharged from the hospital who met the following criteria: chest CT absorption or recovery, normal blood routine, and two consecutive negative nucleic acid tests (within a gap of 24 hours) (Figure 4).
Figure 4.
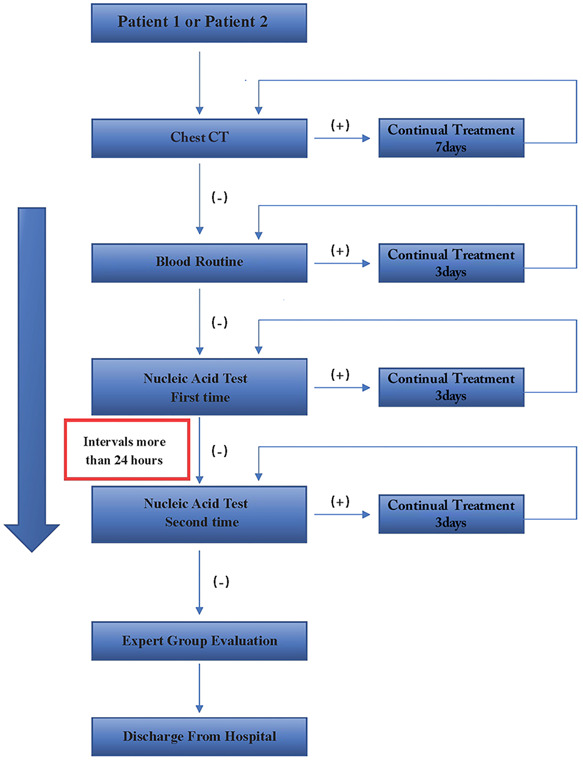
The COVID‐19 patient discharge process. Patient 1: For patients with COVID‐19‐related symptoms, the hospital stay was greater than 14 days, and symptoms could not be present for more than 3 days. Patient 2: For patients without COVID‐19‐related symptoms, the history of close contact with positive patients must have been greater than 14 days. CT, computed tomography
10. RESULTS
During the entire operational period, the WTAH admitted 1124 patients, cured 833 patients, and transferred 291 patients (Figure 5). No patients died or experienced other side effects. No patients returned to the WTAH and no medical staff members were infected with COVID‐19.
Figure 5.
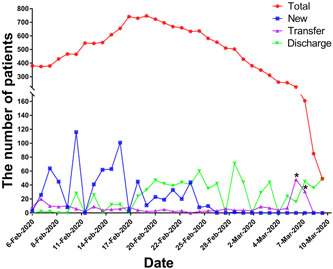
The number of total (red), new (blue), transferred (violet), and discharged (green) patients from 6 February 2020 to 10 March 2020 at Wuchang Temporary Ark Hospital (WTAH). *The asymptomatic patients who were not negative after repeated nucleic acid tests were transferred to designated hospitals for further diagnosis and treatment. Red, the total number of patients per day in WTAH; blue, the number of new patients per day in WTAH; violet, the number of patients transferred to designed hospital per day in WTAH; green, the number of discharged patients per day in WTAH
11. DISCUSSION
Due to China's strong capability of infrastructure construction and organization, 16 TAHs, with more than 20 000 beds, were built within 2 weeks. TAHs were built using an existing stadium, conference center, or other venues; therefore, the required cost and labor were greatly reduced. This TAH was a simple infectious disease hospital, but it had particular requirements for ventilation measures, waste disposal, wastewater disposal, and medical waste disposal. 10 To ensure the safe disposal of hazardous waste, the TAH was equipped with a garbage incinerator. To avoid air contamination, the air ventilation system was modified to meet the epidemic ward criteria.
These TAHs quickly isolated the source of infection in a short period of time. Unlike conventional hospitals, TAHs require less medical equipment, drugs, and staff to operate. 11 , 12 Therefore, the establishment of these hospitals is a good measure for dealing with the outbreak of infectious diseases, especially for the treatment of patients with mild illness. As the operation of the hospital required the cooperation of multiple medical teams, initial communication and cooperation were very important. At the same time, medical material needed to be provided by local designated hospitals. In the process of operation, we also identified some problems. First, it was necessary to do a good job in patient screening, because patients with other basic diseases should not enter the ward. Due to the intensity of cardiovascular and cerebrovascular disease, patients were not always treated and transported in a timely manner. At the same time, the corresponding designated hospital must reserve 5‐10 beds to meet the daily needs of patients arriving from the TAH. Third, with the spread of the epidemic, the concern of patient's psychological problem appears more and more important. 13 Due to the low medical staff allocation, poor medical equipment, and limited medical supplies, some patients were worried about delayed treatment and being marginalized. Medical personnel relieved these patient's worries and eased pressure through singing, dancing, and other activities. However, during the operation period, group events should be avoided as much as possible. Doctors and nurses must strictly follow the procedures to avoid cross‐infection. We discussed each process at weekly meetings and made timely improvements. No medical staff members were infected and no group incidents occurred during the entire period. At the same time, it is also necessary to set the discharge standard and modulate it as the epidemic changes. 9 If the discharge standard is too low, it can lead to many patients being rediagnosed as positive after discharge, requiring readmittance to the hospital. Furthermore, this situation may lead the patients to infect their families.
During the entire operation period, we treated a total of 1124 patients, of which 833 were cured and discharged, and the other 291 patients were transferred to a designated hospital. Most cases of COVID‐19 were mild, and they recovered with active treatment. However, if these patients were not treated, they might have become severe or critical, increasing the mortality rate and increasing the burden on the medical system. 14 This phenomenon can be seen in Figure 5. In the early stage of the epidemic, every day, more patients were admitted to the WTAH, and more patients were transferred to the corresponding designated comprehensive hospital, with a high rate of severe illness. When the epidemic became more controlled and more patients were treated, fewer new patients were admitted to the WTAH, and the time from symptom onset to admission was shorter. Under these circumstances, there were fewer cases of severe disease, the rate of patients being transferred to the corresponding designated comprehensive hospital was lower, and more patients were discharged (Figure 5). If patients might have waited for a hospital bed at home, they might have become more sick, thus unable to be admitted to the hospital; eventually, their illness would have become severe and critical. At the same time, every day, a large number of patients with mild disease recovered from the TAH, which greatly improved the confidence of the patients, isolated the source of infection, and accelerated the improvement of the epidemic situation in the city.
The construction of TAH greatly limited the spread of the epidemic, both within families and in the community, and played a very important role in controlling the source of infection and reducing the number of patients with severe disease.
12. SUMMARY
These TAHs can dramatically and immediately expand the admission capacities of the whole city, reduce the burdens/patient loads of designated comprehensive hospitals, isolate the source of infection, eliminate virus transmission routes, and protect susceptible populations from COVID‐19. In addition, their function was to manage COVID‐19 patients centrally, provide basic medical treatment and care for patients with mild illness, and identify patients with severe illness at an early stage. These hospitals played an important role in the rapid control of COVID‐19 transmission, and they were a successful model in the immediate COVID‐19 epidemic environment.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
AUTHOR CONTRIBUTIONS
XL and HD designed the research study and carried out the research. YY collected and analyzed the data. TW produced the figures and tables. YY and TQ wrote the manuscript.
ETHICS STATEMENT
The study was approved by the ethics committee of Wuhan University Renmin Hospital (Wuhan, China).
Supporting information
Supplementary information
ACKNOWLEDGMENTS
The authors thank Xu Xin for details on the construction of the Wuchang Temporary Ark Hospital. This study was supported by the National Natural Science Foundation of China (Nos. 81870067 and 81972408), Application and Basic Research Project of Wuhan City (No. 2018060401011321), and Innovation Project of Medical School of Wuhan University (TFZZ2018017). The funders had no role in the design of the study and collection, analysis, and interpretation of the data or in writing the manuscript.
Yuan Y, Qiu T, Wang T, et al. The application of Temporary Ark Hospitals in controlling COVID‐19 spread: The experiences of one Temporary Ark Hospital, Wuhan, China. J Med Virol. 2020;92:2019–2026. 10.1002/jmv.25947
Yan Yuan and Tao Qiu contributed equally as co‐first authors in this study.
Contributor Information
Xiuheng Liu, Email: drliuxh@hotmail.com.
Hongping Deng, Email: level1976@163.com.
REFERENCES
- 1. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239‐1242. [DOI] [PubMed] [Google Scholar]
- 2. Lai CC, Liu YH, Wang CY, et al. Asymptomatic carrier state, acute respiratory disease, and pneumonia due to severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2): facts and myths. J Microbiol Immunol Infect. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Velavan TP, Meyer CG. The COVID‐19 epidemic. Trop Med Int Health. 2020;25:278‐280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708‐1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus‐infected pneumonia. N Engl J Med. 2020;382:1199‐1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh PR. Severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) and coronavirus disease‐2019 (COVID‐19): the epidemic and the challenges. Int J Antimicrob Agents. 2020;55:105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Novel Coronavirus Pneumonia Emergency ResponseKey Places Protection and Disinfection Technology Team, Chinese Center for Disease Control and Prevention . Health protection guideline of mobile cabin hospitals during novel coronavirus pneumonia (NPC) outbreak. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54:E006. [DOI] [PubMed] [Google Scholar]
- 8. Bai S, Yu B, Zhang YZ, et al. Challenges of treating adenovirus infection: application of a deployable rapid‐assembly shelter hospital. Disaster Med Public Health Prep. 2018;12:109‐114. [DOI] [PubMed] [Google Scholar]
- 9. Jin YH, Cai L, Cheng ZS, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019‐nCoV) infected pneumonia (standard version). Mil Med Res. 2020;7(1). 10.1186/s40779-020-0233-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhu W, Wang Y, Xiao K, et al. Establishing and managing a temporary coronavirus disease 2019 specialty hospital in Wuhan, China. Anesthesiology. 2020;132(6):1339‐1345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Owens PJ, Forgione A Jr., Briggs S. Challenges of international disaster relief: use of a deployable rapid assembly shelter and surgical hospital. Disaster Manag Response. 2005;3:11‐16. [DOI] [PubMed] [Google Scholar]
- 12. Ren AJ, Sun T, Wang HW, Ge HQ, Ye HJ. Radiology on board the PLA(N) Peace Ark hospital ship during a humanitarian medical relief mission to the Philippines. Disaster Med Public Health Prep. 2016;10:16‐19. [DOI] [PubMed] [Google Scholar]
- 13. Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. Int J Environ Res Public Health. 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID‐19) outbreak—an update on the status. Mil Med Res. 2020;7:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary information


