Abstract
The landscape of advanced endoscopy continues to evolve as new technologies and techniques become available. Although postgraduate advanced endoscopy fellowships have traditionally centered on ERCP and diagnostic EUS, the breadth of training has increased over the years in response to the ever-growing demand for therapeutic endoscopy. The increasing diversity and complexity of emerging endoscopic techniques accompanied by the shift in focus toward competency-based medical education requires innovative changes to the curriculum that will ensure adequate training yet without compromising best patient practices. The purpose of this review is to highlight the expansive array of advanced endoscopic procedures and the challenges of both defining and measuring competence during training. All authors are interventional endoscopists at their respective institutions performing these complex procedures, as well as training fellows in these techniques. We share our perspectives based on our experience navigating through these issues at our institutions and discuss strategies to standardize training and how to potentially incorporate these measures in the process of credentialing and privileging in endoscopy.
Abbreviations: ASGE, American Society for Gastrointestinal Endoscopy; EBT, endoscopic bariatric therapy; ESD, endoscopic submucosal dissection; ESGE, European Society of Gastrointestinal Endoscopy; POEM, peroral endoscopic myotomy; TTT, train the trainer
Graphical abstract
Advanced endoscopy training: the dilemma with numbers
Advanced endoscopy fellowships were initially introduced to meet the need for training in ERCP and EUS. Although the focus of many programs remains on ERCP and EUS, more trainees are gaining exposure to numerous other procedures, including endoscopic ablative procedures, endoscopic stenting, deep enteroscopy, and more recently, “third space” endoscopy and endoscopic bariatric therapies (EBTs). With the increasing complexity of these procedures and the inherent higher risk for adverse events, trainers and trainees alike face the daunting task of measuring and attaining competence in these various techniques within a relatively short period of time. However, because these fellowships are not formally accredited, there is little to no regulatory oversight on the structure of these programs, which has traditionally resulted in significant variability on how training is provided and assessed.
Traditionally, advanced endoscopy training has been based on an apprenticeship model with volume of cases commonly serving as a surrogate for competence. In this model, trainees learn through the observation and performance of procedures under supervision. Initially, the minimum number of cases required to achieve competence in any given procedure was largely based on expert opinion. With time, multiple studies have attempted to identify and validate the minimal procedural number for competence, perhaps best illustrated with regard to ERCP during advanced endoscopy training. Early studies on ERCP suggested that a threshold number as low as 35 was sufficient to achieve competency.1 Subsequent studies, using predefined target measures (ie, biliary cannulation success rate ≥80%, bile duct clearance of choledocholithiasis, successful placement of an endoprosthesis), showed that a threshold of 100 to 200 ERCPs was necessary for competency.2, 3, 4 Based on these studies, the American Society for Gastrointestinal Endoscopy (ASGE) and National Institutes of Health consensus guidelines published in 2002 recommended that competence be assessed after 200 ERCPs.5 , 6 Yet, subsequent publications have suggested different thresholds, with a study from Mayo Clinic recommending more than 350 ERCPs as the minimal procedural number for competency in patients with native papilla.7 More recently, a systematic review published in 2015 reported that the threshold for competency, defined by a high rate of successful selective duct cannulation, ranged from 79 to 300 ERCPs.8 In aggregate, these findings illustrate how identifying a minimal procedural number can be rather elusive, and further highlights how using thresholds as the only endpoint in competence assessment is flawed. First, most of these studies defined performance of a particular intervention (ie, biliary cannulation) as a maker for procedural competency. Yet, interventions such as biliary cannulation, albeit a crucial step, represents only one of the many maneuvers that are commonly performed during ERCP and may not be a good indicator of a trainee’s global competence. Second, we need to recognize that trainees have different educational backgrounds and learn skills at variable rates, therefore absolute thresholds have limited value in this regard. This is particularly evident nowadays when more and more physicians seeking additional training have been in practice for several years, many of whom already possess a background in advanced endoscopy. In addition, as we previously alluded, in the absence of any regulatory oversight, training programs vary significantly in terms of the educational experience provided. Most faculty in these programs are deemed qualified to teach given their own expertise in the field (master-apprenticeship model); yet most of them lack any formal training in teaching endoscopy. The ASGE has published curricula for training in various advanced endoscopic procedures,9 , 10 but training and skills assessment remains variable across the country. Furthermore, trainees with similar number of cases under their belt may not have the same level of readiness for independent practice due to factors beyond numbers. These may include the trainee’s degree of involvement during training (ie, extent of passive observation vs hands-on activity), diversity of case exposure, and level of difficulty associated with the training procedures. With these issues in mind, there has been an increasing effort in endoscopy training, and in medical education in general, to shift away from time-based training toward competency-based education.11
Definitions
Competence in endoscopy
A primary mission of the ASGE is to promote high-quality patient care by ensuring competence in GI endoscopy. The ASGE defines competence in endoscopy as “the minimum level of skill, knowledge, and/or expertise derived through training and experience that is required to safely and proficiently perform a task or procedure.”12 This definition implies that competency involves a combination of both technical and cognitive skills. Equally as important are the integrative skills needed to extract and interpret the information obtained from the procedure to guide patient management. Although not clearly stated in the ASGE definition, competence in endoscopy implies that the trainee should be able to independently perform the procedure upon completion of training. Although these concepts may appear self-explanatory, how to objectively measure competence during advanced endoscopy training remains controversial and challenging.
New technology in advanced endoscopy training
The landscape of advanced endoscopy training continues to evolve as new technologies and techniques become available. The skill set and degree of training required for these novel endoscopic procedures will vary based on multiple factors, including but not limited to the complexity of the technique. In light of this fact, the ASGE has previously set forth guidelines to provide a framework on how to evaluate competence involving new and emerging technologies in GI endoscopy.12
According to the ASGE, a “major skill” describes a new technique or procedure that involves a high level of complexity, interpretative ability, and/or new type of technology. Thus, the development of major skills requires formal training under the supervision of a preceptor(s). Competence in a major skill, as detailed by the ASGE, involves the following: (1) understanding of the indications, benefits, risk, and alternatives to the procedure; (2) having the ability to perform the procedure proficiently and safely; (3) identifying and managing adverse events that may arise; (4) interpreting endoscopic findings accurately; (5) incorporating these into the overall clinical evaluation of the patient; and (6) providing a comprehensive pre- and postprocedural plan.12 , 13 By the completion of training, the trainee is expected to have a degree of competence that allows them to perform the major skill at hand. Based on these criteria, most advanced endoscopic procedures, such as EUS, ERCP, endoscopic submucosal dissection (ESD), and peroral endoscopic myotomy (POEM) would constitute “major” skills requiring dedicated training (Table 1 ). Conversely, the ASGE also recognizes that, in some instances, endoscopic advances may represent minor extensions or minor refinements of established endoscopic procedures. This may include improvements or modifications of existing techniques familiar to the endoscopist (Table 1). As per the guidelines, acquisition of a “minor skill” can thereby be accomplished through limited education and practical exposure, which may involve didactic resources (ie, instructive videos, interactive tutorials) and short dedicated courses.12 , 13 We should emphasize that these definitions by the ASGE should only be used as a framework, because ultimately, the extent of training necessary to achieve competence will largely fluctuate based on the endoscopist’s background. For instance, although radiofrequency ablation may represent a “minor” skill for an endoscopist with experience in the treatment of Barrett’s esophagus, this technique may constitute a “major” skill for a trainee with little to no background in ablative techniques and/or familiarity in the diagnostic evaluation of Barrett’s esophagus. Similarly, as discussed later, although some EBTs may be considered “minor” skills (Table 1), these procedures should not be performed in silo, and most endoscopists may still require dedicated training to fully understand the role of these procedures within the multifaceted treatment of obesity.
Table 1.
Sample classification of endoscopic procedures as either major or minor skills based on the American Society for Gastrointestinal Endoscopy definitions
| Major skill | Minor skill |
|---|---|
| EUS ERCP Endoscopic submucosal dissection Peroral endoscopic myotomy |
Radiofrequency ablation of Barrett’s esophagus Endoscopic placement of intragastric balloons for weight loss Over-the-scope clip |
Current trends in advanced endoscopy training involving new technologies
The practice of GI endoscopy is dynamic, and the breadth of procedures continues to increase. Consequently, endoscopists are faced with the challenge of seeking and attaining proper training in these new technologies over the course of their career. In recent years, with the transition toward a competency-based training curriculum, we have witnessed the development and integration of standardized measurement tools that aim at providing both quantitative and qualitative assessment in endoscopic training.14, 15, 16 However, with the expanding array of endoscopic techniques, both the challenge and focus is now shifting on how do we adequately measure competence among trainees in novel technologies. Among these, “third space” and bariatric endoscopy have gained traction over recent years as budding subspecialties within the field of advanced endoscopy.
Third-space endoscopy
Third-space endoscopy, also referred as submucosal endoscopy, is based on the concept that the deeper layers of the GI tract can be accessed via the submucosal space. With advances in endoscopic devices and refinement in techniques, we have witnessed the evolution of third-space endoscopy from a vanguard concept to techniques in routine clinical use, including the widespread adoption and dissemination of procedures such as ESD and POEM.
Endoscopic submucosal dissection
ESD was initially introduced in Japan as a minimally invasive alternative to surgery for the management of early gastric cancer. Given its efficacy and safety in the hands of Japanese experts, this technique has evolved and shifted to include lesions in the lower GI tract. The main advantage of ESD over endoscopic mucosal resection (EMR) is the ability to achieve en bloc resection of lesions irrespective of size and thereby lowering the risk for local recurrence.17 However, this procedure is associated with a steep learning curve and potential risk for serious adverse events.
ESD training in Japan follows the traditional master-apprentice model. This template for therapeutic training has been very successful in Japan, where trainees are highly subspecialized and undergo extensive cognitive and technical training under direct supervision. However, due to multiple factors, including the limited number of local ESD experts and training opportunities, this model is not translatable to Western countries. Consequently, the transition of ESD to the West has been slower than its uptake in Asia.18 In light of these issues, the European Society of Gastrointestinal Endoscopy (ESGE) recently issued a position statement with recommendations for a core curriculum to achieve high-quality training in ESD,19 clearly outlining that trainees should not perform complex endoscopic procedures in humans independently without having undergone sufficient training (ie, supervised cases by experts, structured focused fellowships). The primary aims of this curriculum included (1) the definition of skills and competence needed before ESD training; (2) development of a standardized core curriculum for ESD practice through the establishment of minimum standards; (3) and definition of a training program for endoscopists who want to start ESD practice in their center.
The ESGE recognizes that competence in ESD requires an in-depth understanding of all the available modalities for appropriate lesion characterization and selection. Hence, proficiency in advanced diagnostic techniques, including knowledge of endoscopic classification systems, are considered a requisite before ESD training. Given that ESD is a technically complex procedure that requires precise endoscope control, previous EMR skills are necessary to serve as a foundation for the skills needed in advanced resection, including injection, hemostasis, and management of adverse events.
The core curriculum proposed by the ESGE guidelines parallels training pathways that have been previously suggested for ESD training in the West.18 , 20 , 21 As we have previously suggested,18 , 20 , 21 live ESD courses and meetings can serve as an initial venue for trainees to learn the basics on theoretical knowledge, techniques, and ESD devices. Hands-on training on animal models is strongly recommended because this has been shown to improve ESD outcomes and the skills needed for the management of adverse events.22 , 23 The ESGE recommends that trainees should perform at least 20 ESD procedures on animal models before undertaking any human cases. After this, trainees should observe (20 cases) and assist (5 cases) experts on live human ESD procedures before performing cases on carefully selected lesions under direct supervision (10 cases). According to this ESGE curriculum, trainees can then start ESD in their own centers once they have fulfilled these requirements as confirmed by an “expert in ESD.”19 Although these guidelines provide a potential framework for ESD training, several logistical issues should be highlighted. This model is difficult to adopt in the United States where cases are sporadic, even in specialized centers. ESD trainees are often full-time interventional endoscopists at their own institutions and may not be able to arrange travel arrangements at short notice. Due to hospital policies, visiting trainees are often restricted to observing cases only, because they are not credentialed to actively “assist” in the care of patients. We need to recognize that these suggested guidelines are mainly based on expert opinion and that robust data substantiating these training recommendations are lacking.
Peroral endoscopic myotomy
POEM is a minimally invasive endoscopic technique initially developed approximately a decade ago for the management of esophageal motility disorders.24 Since its introduction into clinical practice, POEM has become widely accepted given its excellent short- and mid-term outcomes and safety profile.25 , 26 However, as a modified natural orifice transluminal surgical procedure, training in POEM presents several challenges. The procedure is technically complex and demands advanced endoscopic skills, knowledge of both intra- and extraluminal anatomy of the GI tract, and the ability to manage adverse events that may include pneumothorax and pneumoperitoneum. Despite the rapid dissemination of this technique, there is little published information regarding training in POEM.27 , 28 In 2017, the Japan Gastroenterological Endoscopy Society launched a committee for POEM to establish clinical guidelines to serve as a decision-making tool and to ensure minimum standards of practice.29
The Japan Gastroenterological Endoscopy Society-sponsored clinical guideline introduces several recommendations regarding training and teaching programs for POEM. Similar to the ESGE positional statement on ESD, this clinical guideline on POEM recommends that initial skill acquisition should be met through training on animal models, including organ and live models, although a minimum threshold is not provided.29 However, in a single-center prospective study using both ex vivo and live swine models, mastery, defined as the absence of intraprocedural adverse events and a plateau in procedural time, was achieved by trainees after 26 cases.30 Subsequently, training progresses by observation of POEM cases followed by proctoring of live human cases by an experienced operator, who can provide step-by-step supervision and guidance through the initial cases. The literature on the learning curve for POEM is conflicting due to differences in definitions and heterogeneous training backgrounds. Not surprisingly, there is a wide discrepancy in the learning curve plateau reported, ranging from 7 to 100 cases,31, 32, 33, 34, 35 with many of these reporting data from animal models, or highlighting single-center or single-operator experiences, rather than studies designed to assess training and competency in POEM. Hence, similar to training in ESD, these recommendations are based on expert opinion rather than formal training data.
Endoscopic bariatric therapies
The obesity epidemic continues to increase in the United States and globally; yet, only 1% of eligible patients undergo conventional bariatric surgery.36 More recently, EBTs have emerged as an adjunctive endoscopic option to traditional surgical treatments for obesity, with multiple endoscopic devices and techniques demonstrating safety and efficacy in prospective randomized studies.37 EBT encompasses a broad array of procedures, including primary weight loss interventions and treatment of adverse events from bariatric surgery. Similar to other emerging technologies, there are a paucity of data regarding training requirements in EBT. In 2015, the ASGE issued a position statement on EBT in clinical practice, recommending that endoscopists partaking in EBT should demonstrate competency in upper endoscopy and endoscopic hemostasis.38 Given the diversity of EBT procedures, the duration and type of training will vary, depending on the complexity of the particular intervention. The ASGE suggests that focused training via dedicated courses are potential settings to gain further expertise in certain aspects of EBT.38 , 39 Many of these courses are sponsored and organized by industry, which plays a vital role in the training and education of these new devices. Yet, moving forward, there is a need to introduce standardized criteria for the teaching and evaluation of these new techniques among the various courses, and to reduce variability in learning and potential for conflict of interest. Conversely, EBTs of greater complexity may require proctoring and a structured training program; albeit no specific recommendations regarding procedural thresholds are provided by the ASGE given the scarcity of data in this area. A few studies have attempted to define learning curves with endoscopic sleeve gastroplasty, a gastric-restrictive procedure commonly performed with endoscopic suturing.40, 41, 42 However, threshold numbers to achieve “efficiency” varied greatly from 7 to 38 cases, due to the heterogeneous definitions and variable outcome measures across the studies. These data were based on endoscopists who had extensive previous experience with the endoscopic suturing device. Overall, both the ASGE and the American Society for Metabolic and Bariatric Surgery emphasize that EBT should not be carried out in isolation and that endoscopists performing EBT should be part of a multidisciplinary comprehensive obesity program.38 , 39
Current challenges and strategies in establishing an advanced endoscopy training curriculum for novel procedures
As previously discussed, with the shift toward competency-based medical education, there is an increased emphasis on establishing an outcomes-based training curriculum; with the goals of reducing variation in the quality of endoscopy, and to define standards within the field of advanced endoscopy that may help identify areas for quality improvement. Although major strides have been made in the standardized assessment of ERCP and EUS training,43, 44, 45 several challenges remain when attempting to implement a structured training program for emerging endoscopic procedures.
Training the trainers
In the traditional “see one, do one, teach one” training model, teachers are identified based on their own expertise within a particular field of interest. These teachers then serve as mentors and are responsible for identifying when their students have fulfilled their training requirements. A national audit of colonoscopy performance in the United Kingdom identified the numerous pitfalls of this informal and highly subjective teaching approach,46 , 47 which subsequently sparked the implementation of various strategies aimed at improving endoscopic training.15 , 16 One of the key issues identified included the importance of developing programs to “train the trainer” (TTT), based on the premise that simply acquiring the skill of performing an endoscopic procedure does not explicitly translate to an ability to be an effective endoscopy trainer.48 Since their implementation in the United Kingdom in an effort to improve colonoscopy quality outcomes, these TTT programs have been applied in other countries with proven impact on endoscopic training.49 The TTT model promotes standardization of training by (1) educating the trainer on how to effectively and efficiently teach endoscopy; and (2) stressing the need to develop a structured curriculum with pre-established learning objectives.48 The adoption of this training program, designed to upskill endoscopists, should help build an effective trainer pool over time, which is paramount for the dissemination of novel endoscopic skills.50
Lack of local experts and training opportunities
As happens with any technology, novel techniques are often only performed by a few experts before their widespread dissemination and adoption. Strategies to overcome this limitation, as has been the case for procedures such as ESD and POEM, have involved the pilgrimage of Western endoscopists to Asia to learn these techniques. However, this model of training is both impractical and unsustainable by most trainees, particularly those who are already in clinical practice. In response to this increasing need, we have witnessed an exponential growth in educational resources for individuals interested in acquiring new endoscopic skills. Live and hands-on courses for various endoscopic techniques (ie, endoscopic resection techniques, POEM, EBT) have become readily available at national and international endoscopy conferences, through individual institutions and professional societies.18 It is important to acknowledge, however, that these focused training courses, although possibly adequate for the acquisition of new minor endoscopic skills, should be regarded as only complementary in the training of more complex techniques. Although hands-on practice on animal models has often been advocated as an integral component in endoscopy training, particularly in the acquisition of major skills,19 animal laboratories are costly and not widely available. Simulation-based training in GI endoscopy may be a valuable adjunct tool that can help trainees acquire new skills and accelerate the learning curve in a low-risk environment.51 , 52 This may be particularly attractive for training in third space endoscopy, given the lack of local experts, training opportunities, and high stakes with these complex interventions. Theoretically, with simulation-based training, learners should be able to repetitively perform the intended skills and adjust training to target specific skills or build upon existing competencies with no risk to patients. However, there is currently a scarcity of data examining the ability of simulators as tools to assess endoscopic skill. Hence, although promising, additional studies on simulator-based assessment tools with predictive validity are necessary before we can determine their role compared with the acquisition of technical and cognitive competency via standard endoscopic training.53
Similarly, real-time assessment and provision of data on trainee performance can be challenging, depending on the available of local experts. More recently, indirect assessment methods, including video-recorded procedures, have been evaluated as an alternative to live assessment.54 Video recording allows careful review and debriefing of procedures after the training session, which may facilitate the exchange between mentor and trainee. With technological innovations and increasing broadband availability, video-based live instruction (during animal hands-on training, simulation-based sessions, or even human cases) may be a potential strategy for endoscopic education of highly specialized new techniques even with mentors in geographically distant locations.55 This approach may become even more prominent due to the expected higher precautionary restrictions on travel and visiting endoscopists in light of the recent worldwide coronavirus (SARS-CoV-2) pandemic.56
Standardization of training and assessment tools
Trainees learn and acquire endoscopic skills at variable rates; thus, recommended minimum volume thresholds in silo cannot ensure competence. For example, with ESD training, we cannot expect that the needs and requirements of an individual who just graduated from GI fellowship will be the same as that of a practicing endoscopist with extensive experience in EMR. Hence, the duration and intensity of training should be in part dictated by the trainee’s background. Given the complexity of some of these techniques, it is unrealistic to expect that all trainees can acquire these skills through the standard advanced endoscopy fellowship pathway. In recognition of this limitation, several advanced endoscopy training programs have modified their curriculum to meet the specific needs and expectations of the trainee. Likewise, we need to acknowledge that many endoscopists seeking training in novel technologies do not necessarily do so through the formal advanced endoscopy fellowship pathway. Given this heterogeneity, there is an urgent need to standardize training, especially given the paucity of data on learning curves for novel procedures and the numerous training pathway permutations.50
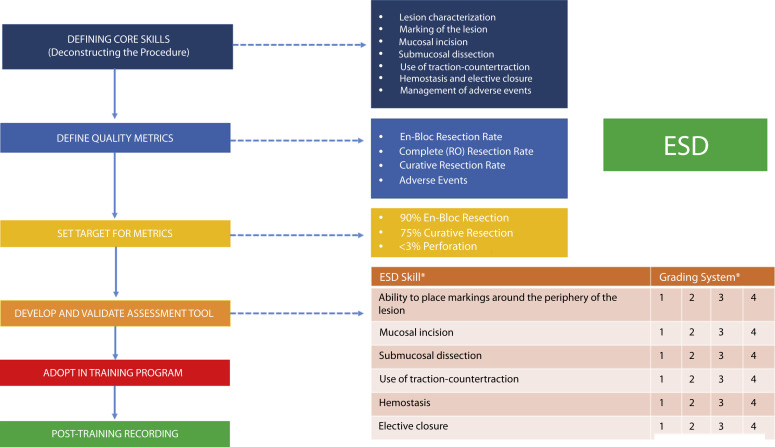
In Figure 1 , we outline the suggested steps to consider when developing a training curriculum for a novel endoscopic procedure. First, core skills for each novel procedure should be defined, which can be achieved by deconstructing the technique into a series of sequential steps. In the case of ESD, these steps may include lesion assessment before resection, marking the margins of the lesion, mucosal incision, submucosal dissection, use of traction-countertraction during the procedure, elective closure, and management of adverse events. The next step is to define quality metrics based on outcomes data and set these as benchmarks during training (ie, en bloc resection and adverse event rates). For instance, the ESGE training curriculum for ESD proposes a 90% en bloc resection rate with <3% perforation rate as threshold targets.19 Once these core skills and target metrics are established, the next steps would involve the development and validation of an assessment tool followed by its adoption in formal competency-based training programs (Fig. 1). These assessment tools must be procedure specific based on the predefined outcome metrics, which is key in ensuring that endoscopists, irrespective of their training background, meet the expected quality benchmarks for clinical practice. Post-training evaluation (ie, assessment of prospective case log with documentation of quality indicators) will be key in validating the efficacy of the assessment tools in establishing competency in terms of independent practice.
Figure 1.
Flow diagram for the creation of a structured training curriculum for novel endoscopic procedures using endoscopic submucosal dissection (ESD) as an example. ∗The ESD assessment tool in the diagram is used to illustrate potential core skills that could be graded using a numerical score. This is not a complete list or a validated tool.
Maintenance of skills/competence
The maintenance of endoscopic competence is equally as important as the skill acquisition process. Many of these novel advanced endoscopic techniques, such as ESD and POEM, are complex and technically demanding. Maintaining skills is highly dependent on case volume, which can be difficult to attain due to multiple factors, including low incidence of certain illnesses (ie, gastric cancer in the United States) or reimbursement issues (ie, ESD, POEM, EBT). Thus, endoscopists should have a well thought out plan before undertaking training in new endoscopic skills. This initial plan should include prediction of future case volume at their own center to ensure maintenance of skills, and perhaps even more importantly, justifying the need for training in this new skill in the first place. Obtaining institutional endorsement on various fronts is key before starting training. For instance, institutional support at our institutions (University of Florida and University of Colorado) allowed us to make infrastructural adjustments to facilitate the introduction of POEM and ESD into our endoscopy unit, thereby easing the incorporation of these procedures into the schedule.57 Institutional support in terms of protected time to train in an animal laboratory is also highly desirable, because this can be a complementary strategy to maintain skills and avoid spaced training initially when human cases are relatively infrequent.19 Although beyond the scope of this review, it is important to recognize that many of these interventions do not have dedicated procedural terminology (CPT) codes. Upfront discussion with stakeholders with regard to billing and coding is essential to ensure the necessary case volume to sustain newly acquired skill sets.57
Credentialing and privileging for new endoscopic techniques
Credentialing is the process whereby an institution reviews an endoscopist’s qualifications to determine if they meet the criteria to perform the endoscopic procedure in question. Traditionally, preceptors have been responsible in establishing when a trainee has reached “an acceptable level of competency” and thereby provide written documentation of the successful completion of the training for future credentialing purposes.12 , 13 Hospital credentialing committees then determine who will be granted privileges based on the supporting evidence. There are several issues worthy of discussion with regard to how this process is currently structured.
Definition and assessment of competence
As we have previously discussed, defining competence remains a challenge in endoscopic training. The assessment of competence by tallying the total number of procedures performed is not sufficient. Although the performance of a minimum volume is a prerequisite for skill acquisition, it does not guarantee competence; herein lies the importance of establishing procedure-specific benchmarks that can be used as concrete performance endpoints. Continuous recording of performance data into accessible electronically generated centralized endoscopic databases would potentially allow third parties (ie, hospital credentialing committees) to then identify and search for these target benchmarks.12
Responsibility of establishing competency in endoscopy training
The current certification of competency in endoscopy is usually provided by a training program director. However, there are several limitations to this approach. First, a trainee’s performance is based on the subjective evaluation by his/her mentor, which, by itself, may introduce bias in the credentialing process. Second, in the absence of standards and objective parameters, there is likely substantial variation among training directors on what may be considered an “acceptable level of competency.” Competency should be procedure specific. Hence, competence in a particular procedure does not necessarily translate into competence in a materially different one. Third, as previously discussed, many endoscopists interested in acquiring new endoscopic skills do not undergo formal advanced endoscopy training and may do so through different training pathways. This poses a challenge in the absence of clear guidelines on how or who should be responsible in attesting to the competency of these individuals.
In light of these concerns, the ASGE has previously issued a statement regarding the important role of proctoring in the process of endoscopic privileging.12 , 13 According to these guidelines, a proctor should be an endoscopist who is credentialed in the specific procedure being observed, has no physician or patient relationship, and reports directly to the institution’s credentialing committee. The role of the proctor is to provide an unbiased evaluation of the endoscopist’s competence in the procedure in question. However, similar to the issues regarding the lack of locally available experts, we presume that the pool of qualified proctors for emerging new technologies will also be scarce. Video-based proctoring may be a viable strategy in the future. Reliable, blinded video-based proctoring could potentially provide an unbiased assessment in the credentialing process.54 , 55
Responsibility for privileging, conflicts of interest, and the lack of uniform standards
There are no established national standards for granting endoscopic privileges. The current credentialing process in the United States requires each hospital and its credentialing committee to manage the process of granting privileges. It is the responsibility of each institution to develop and maintain their own guidelines regarding this process, which potentially introduces conflict of interest; hospital credentialing committees may be subject to external pressure from the applicants, their employers, and even competitors.58 Many hospitals may be pressured to offer a broad range of endoscopic procedures due to economic incentives. Similarly, the pursuit for endoscopic innovation and the distinction of being the “first” hospital to offer a novel procedure may unintentionally influence and circumvent the safeguard training and credentialing requirements necessary for such processes. In the case of many novel endoscopic techniques, trainees often use certificates of attendance from industry-sponsored courses to support their application. However, most of these exposure courses vary significantly in length, content, didactics, and hands-on training. Importantly, with a few exceptions for the acquisition of minor skills as previously discussed, most of these courses do not attest to the competence of the attendees. The ultimate solution would be the establishment of an independent board for endoscopic procedural credentialing that would remove conflicts of interest from hospital credentialing committees. Requiring certification for endoscopic procedures by a national board would help oversee that endoscopic privileges are granted to hospitals that meet the established national consensus parameters in order to safeguard best patient practices and ensure uniformity of the process across all institutions. This step is particularly crucial in assuring the safe stepwise dissemination and adoption of new technologies in clinical practice. Until then, criteria for endoscopic privileging could be established by national consensus standards developed by professional societies based on evidence and expert opinion, including experiences from centers across the world. These professional societies could also help identify and assign independent proctors, which would help limit any undue influence from either the applicant or hospital on the evaluation process.
Conclusion
GI endoscopy is an exciting and continuously evolving field. The age-old dictum of “see one, do one, teach one” is dated with the increasing diversity and complexity of emerging endoscopic techniques and the shift toward competency-based medical education. Minimal threshold numbers are an integral part of training; yet do not guarantee competence. Defining competence in endoscopy must be procedure specific, starting with the identification of core skills, and establishing quality metrics and benchmarks for a given technique. The development of validated procedure-specific assessment tools can then help in the evaluation of these predefined targets. Training in novel emergent endoscopic techniques can be obtained through various pathways, and the integration of standard advanced fellowships and other resources, including simulation-based learning and video-based teaching, may further broaden and tailor the educational opportunities to a widely diverse trainee population. It cannot be overemphasized that short weekend courses and training in animal models do not necessarily qualify as a permit to start performing these newer endoscopic procedures ion humans independently. National consensus standards for endoscopic privileging are needed in order to reduce variation in endoscopy practice and ensure that all patients are optimally managed.
Footnotes
DISCLOSURE: Dr Yang is a consultant for Boston Scientific, Lumendi, and Steris. Dr Wagh is a consultant for Boston Scientific, Medtronic, Olympus, and Incyte. Dr Draganov is a consultant for Boston Scientific, Olympus, Cook Medical, Lumendi, and Microtech.
References
- 1.American College of Physicians. Clinical competence in diagnostic endoscopic retrograde cholangiopancreatography Health and Public Policy Committee, American College of Physicians. Ann Intern Med. 1988;108:142–144. [PubMed] [Google Scholar]
- 2.Watkins J.L., Etzkorn K.P., Wiley T.E. Assessment of technical competence during ERCP training. Gastrointest Endosc. 1996;44:411–415. doi: 10.1016/s0016-5107(96)70090-1. [DOI] [PubMed] [Google Scholar]
- 3.Jowell P.S., Baillie J., Branch M.S. Quantitative assessment of procedural competence: a prospective study of training in endoscopic retrograde cholangiopancreatography. Ann Intern Med. 1996;125:983–989. doi: 10.7326/0003-4819-125-12-199612150-00009. [DOI] [PubMed] [Google Scholar]
- 4.Garcia-Cano J. 200 supervised procedures: the minimum threshold number for competency in performing endoscopic retrograde cholangiopancreatography. Surg Endosc. 2007;21:1254–1255. doi: 10.1007/s00464-006-9013-y. [DOI] [PubMed] [Google Scholar]
- 5.Eisen G.M., Baron T.H., Dominitz J.A. Methods of granting hospital privileges to perform gastrointestinal endoscopy. Gastrointest Endosc. 2002;55:780–783. doi: 10.1016/s0016-5107(02)70403-3. [DOI] [PubMed] [Google Scholar]
- 6.NIH state-of-the-science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy. NIH Consens State Sci Statements. 2002;19:1–26. [PubMed] [Google Scholar]
- 7.Verma D., Gostout C.J., Petersen B.T. Establishing a true assessment of endoscopic competence in ERCP during training and beyond: a single-operator learning curve for deep biliary cannulation in patients with native papillary anatomy. Gastrointest Endosc. 2007;65:394–400. doi: 10.1016/j.gie.2006.03.933. [DOI] [PubMed] [Google Scholar]
- 8.Shahidi N., Ou G., Telford J. When trainees reach competency in performing ERCP: a systematic review. Gastrointest Endosc. 2015;81:1337–1342. doi: 10.1016/j.gie.2014.12.054. [DOI] [PubMed] [Google Scholar]
- 9.ASGE Training Committee. Jorgensen J., Kubiliun N., Law J.K. Endoscopic retrograde cholangiopancreatography (ERCP): core curriculum. Gastrointest Endosc. 2016;83:279–289. doi: 10.1016/j.gie.2015.11.006. [DOI] [PubMed] [Google Scholar]
- 10.ASGE Training Committee. DiMaio C.J., Mishra G., McHenry L. EUS core curriculum. Gastrointest Endosc. 2012;76:476–481. doi: 10.1016/j.gie.2012.04.437. [DOI] [PubMed] [Google Scholar]
- 11.Nasca T.J., Philibert I., Brigham T. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366:1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 12.ASGE Standards of Practice Committee. Faulx A.L., Lightdale J.R., Acosta R.D. Guidelines for privileging, credentialing, and proctoring to perform GI endoscopy. Gastrointest Endosc. 2017;85:273–281. doi: 10.1016/j.gie.2016.10.036. [DOI] [PubMed] [Google Scholar]
- 13.ASGE Guidelines for clinical application. Methods of privileging for new technology in gastrointestinal endoscopy. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. 1999;50:899–900. doi: 10.1016/s0016-5107(99)70190-2. [DOI] [PubMed] [Google Scholar]
- 14.Wani S., Keswani R.N., Petersen B. Training in EUS and ERCP: standardizing methods to assess competence. Gastrointest Endosc. 2018;87:1371–1382. doi: 10.1016/j.gie.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Siau K., Crossley J., Dunckley P. Direct observation of procedural skills (DOPS) assessment in diagnostic gastroscopy: nationwide evidence of validity and competency development during training. Surg Endosc. 2020;34:105–114. doi: 10.1007/s00464-019-06737-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siau K., Crossley J., Dunckley P. Colonoscopy direct observation of procedural skills assessment tool for evaluating competency during training. Am J Gastroenterol. 2019;115:234–243. doi: 10.14309/ajg.0000000000000426. [DOI] [PubMed] [Google Scholar]
- 17.Yang D., Othman M., Draganov P.V. Endoscopic mucosal resection vs. endoscopic submucosal dissection for Barrett’s esophagus and colorectal neoplasia. Clin Gastroenterol Hepatol. 2019;17:1019–1028. doi: 10.1016/j.cgh.2018.09.030. [DOI] [PubMed] [Google Scholar]
- 18.Kotzev A.I., Yang D., Draganov P.V. How to master endoscopic submucosal dissection in the USA. Dig Endosc. 2019;31:94–100. doi: 10.1111/den.13240. [DOI] [PubMed] [Google Scholar]
- 19.Pimentel-Nunes P., Pioche M., Albeniz E. Curriculum for endoscopic submucosal dissection training in Europe: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2019;51:980–992. doi: 10.1055/a-0996-0912. [DOI] [PubMed] [Google Scholar]
- 20.Draganov P.V., Coman R.M., Gotoda T. Training for complex endoscopic procedures: how to incorporate endoscopic submucosal dissection skills in the West? Expert Rev Gastroenterol Hepatol. 2014;8:119–121. doi: 10.1586/17474124.2014.864552. [DOI] [PubMed] [Google Scholar]
- 21.Coman R.M., Gotoda T., Draganov P.V. Training in endoscopic submucosal dissection. World J Gastrointest Endosc. 2013;5:369–378. doi: 10.4253/wjge.v5.i8.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gromski M.A., Cohen J., Saito K. Learning colorectal endoscopic submucosal dissection: a prospective learning curve study using a novel ex vivo simulator. Surg Endosc. 2017;31:4231–4237. doi: 10.1007/s00464-017-5484-2. [DOI] [PubMed] [Google Scholar]
- 23.Martinek J., Suchanek S., Stefanova M. Training on an ex vivo animal model improves endoscopic skills: a randomized, single-blind study. Gastrointest Endosc. 2011;74:367–373. doi: 10.1016/j.gie.2011.04.042. [DOI] [PubMed] [Google Scholar]
- 24.Inoue H., Minami H., Kobayashi Y. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy. 2010;42:265–271. doi: 10.1055/s-0029-1244080. [DOI] [PubMed] [Google Scholar]
- 25.Akintoye E., Kumar N., Obaitan I. Peroral endoscopic myotomy: a meta-analysis. Endoscopy. 2016;48:1059–1068. doi: 10.1055/s-0042-114426. [DOI] [PubMed] [Google Scholar]
- 26.Crespin O.M., Liu L.W.C., Parmar A. Safety and efficacy of POEM for treatment of achalasia: a systematic review of the literature. Surg Endosc. 2017;31:2187–2201. doi: 10.1007/s00464-016-5217-y. [DOI] [PubMed] [Google Scholar]
- 27.NOSCAR POEM White Paper Committee. Stavropoulos S.N., Desilets D.J., Fuchs K.H. Per-oral endoscopic myotomy white paper summary. Gastrointest Endosc. 2014;80:1–15. doi: 10.1016/j.gie.2014.04.014. [DOI] [PubMed] [Google Scholar]
- 28.Mittal C., Wagh M.S. Training pathways and competency assessment in peroral endoscopic myotomy (POEM) Techn Gastrointest Endosc. 2017;19:170–174. [Google Scholar]
- 29.Inoue H., Shiwaku H., Iwakiri K. Clinical practice guidelines for peroral endoscopic myotomy. Dig Endosc. 2018;30:563–579. doi: 10.1111/den.13239. [DOI] [PubMed] [Google Scholar]
- 30.Hernandez Mondragon O.V., Rascon Martinez D.M., Muňoz Bautista A. The Per Oral Endoscopic Myotomy (POEM) technique: how many preclinical procedures are needed to master it? Endosc Int Open. 2015;3:E559–E565. doi: 10.1055/s-0034-1392807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Teitelbaum E.N., Soper J.N., Arafat F.O. Analysis of a learning curve and predictors of intraoperative difficulty for peroral esophageal myotomy (POEM) J Gastrointest Surg. 2014;18:92–98. doi: 10.1007/s11605-013-2332-0. [DOI] [PubMed] [Google Scholar]
- 32.El Zein M., Kumbhari V., Ngamruengphong S. Learning curve for peroral endoscopic myotomy. Endosc Int Open. 2016;4:E577–E582. doi: 10.1055/s-0042-104113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kurian A.A., Dunst C.M., Sharata A. Peroral endoscopic esophageal myotomy: defining the learning curve. Gastrointest Endosc. 2013;77:719–725. doi: 10.1016/j.gie.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Patel K.S., Calixte R., Modayil R.J. The light at the end of the tunnel: a single-operator learning curve analysis for peroral endoscopic myotomy. Gastrointest Endosc. 2015;81:1181–1187. doi: 10.1016/j.gie.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 35.Liu Z., Zhang X., Zhang W. Comprehensive evaluation of the learning curve for peroral endoscopic myotomy. Clin Gastroenterol Hepatol. 2018;16:1420–1426. doi: 10.1016/j.cgh.2017.11.048. [DOI] [PubMed] [Google Scholar]
- 36.Goyal D., Watson R.R. Endoscopic bariatric therapies. Curr Gastroenterol Rep. 2016;18:26. doi: 10.1007/s11894-016-0501-5. [DOI] [PubMed] [Google Scholar]
- 37.Sullivan S., Edmundowicz S.A., Thompson C.C. Endosocpic bariatric and metabolic therapies: new and emerging technologies. Gastroenterology. 2017;152:1791–1801. doi: 10.1053/j.gastro.2017.01.044. [DOI] [PubMed] [Google Scholar]
- 38.ASGE Bariatric Endoscopy Task Force. Sullivan S., Kumar N., Edmundowicz S.A. ASGE position statement on endoscopic bariatric therapies in clinical practice. Gastrointest Endosc. 2015;82:767–772. doi: 10.1016/j.gie.2015.06.038. [DOI] [PubMed] [Google Scholar]
- 39.ASGE/ASMBS Task Force on Endoscopic Bariatric Therapy. Ginsberg G.G., Chand B., Cote G.A. A pathway to endoscopic bariatric therapies. Gastrointest Endosc. 2011;74:943–953. doi: 10.1016/j.gie.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 40.Shahnazarian V., Ramai D., Sarkar A. Endoscopic bariatric therapies for treating obesity: a learning curve for gastroenterologists. Transl Gastroenterol Hepatol. 2019;4:16. doi: 10.21037/tgh.2019.03.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hill C., El Zein M., Agnihotri A. Endoscopic sleeve gastroplasty: the learning curve. Endosc Int Open. 2017;5:E900–E904. doi: 10.1055/s-0043-115387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Saumoy M., Schneider Y., Zhou X.K. A single-operator learning curve analysis for the endoscopic sleeve gastroplasty. Gastrointest Endosc. 2018;87:442–447. doi: 10.1016/j.gie.2017.08.014. [DOI] [PubMed] [Google Scholar]
- 43.Wani S., Hall M., Wang A.Y. Variation in learning curves and competence for ERCP among advanced endoscopy trainees by using cumulative sum analysis. Gastrointest Endosc. 2016;83:711–719. doi: 10.1016/j.gie.2015.10.022. [DOI] [PubMed] [Google Scholar]
- 44.Wani S., Keswani R., Hall M. A prospective multicenter study evaluating learning curves and competence in endoscopic ultrasound and endoscopic retrograde cholangiopancreatography among advanced endoscopy trainees: the Rapid Assessment of Trainee Endoscopy Skills (RATES) study. Clin Gastroenterol Hepatol. 2017;15:1758–1767. doi: 10.1016/j.cgh.2017.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wani S., Han S., Simon V. Setting minimum standards for training in EUS and ERCP: results from a prospective multicenter study evaluating learning curves and competence among advanced endoscopy trainees. Gastrointest Endosc. 2019;89:1160–1168. doi: 10.1016/j.gie.2019.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gavin D.R., Valori R.M., Anderson J.T. The national colonoscopy audit: a nationwide assessment of the quality and safety of colonoscopy in the UK. Gut. 2013;62:242–249. doi: 10.1136/gutjnl-2011-301848. [DOI] [PubMed] [Google Scholar]
- 47.Valori R. Quality improvements in endoscopy in England. Techn Gastrointest Endosc. 2012;14:63–72. [Google Scholar]
- 48.Waschke K.A., Anderson J., Macintosh D. Training the gastrointestinal endoscopy trainer. Best Pract Res Clin Gastroenterol. 2016;30:409–419. doi: 10.1016/j.bpg.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 49.Kaminski M.F., Anderson J.A., Valori R. Leadership training to improve adenoma detection rate in screening colonoscopy: a randomized trial. Gut. 2016;65:616–624. doi: 10.1136/gutjnl-2014-307503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Waschke K.A., Anderson J., Valori M. ASGE principles of endoscopic training. Gastrointest Endosc. 2019;90:27–34. doi: 10.1016/j.gie.2018.10.017. [DOI] [PubMed] [Google Scholar]
- 51.Khan R., Plahouras J., Johnston B.C. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database Syst Rev. 2018;8:CD008237. doi: 10.1002/14651858.CD008237.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mahmood T., Darzi A. The learning curve for a colonoscopy simulator in the absence of any feedback: no feedback, no learning. Surg Endosc. 2004;18:1224–1230. doi: 10.1007/s00464-003-9143-4. [DOI] [PubMed] [Google Scholar]
- 53.Cohen J., Bosworth B.P., Chak A. Preservation and incorporation of valuable endoscopic innovations (PIVI) on the use of endoscopy simulators for training and assessing skill. Gastrointest Endosc. 2012;76:471–475. doi: 10.1016/j.gie.2012.03.248. [DOI] [PubMed] [Google Scholar]
- 54.Scaffidi M.A., Grover S.C., Carnahan H. A prospective comparison of live and video-based assessments of colonoscopy performance. Gastrointest Endosc. 2018;87:766–775. doi: 10.1016/j.gie.2017.08.020. [DOI] [PubMed] [Google Scholar]
- 55.Huang R.J., Limsui D., Triadafilopoulos G. Video-based performance assessment in endoscopy: Moving beyond “see one, do one, teach one”? Gastrointest Endosc. 2018;87:776–777. doi: 10.1016/j.gie.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 56.Castro Filho E.C., Castro R., Fernandes F.F. Gastrointestinal endoscopy during the COVID-19 pandemic: an updated review of guidelines and statements from international and national societies. Gastrointest Endosc. 2020;92:440–445.e6. doi: 10.1016/j.gie.2020.03.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang D., Draganov P.V. Introducing POEM in your institution: the blueprint for launching a new program in the endoscopy suite. Pract Gastroenterol. 2016;32:52–56. [Google Scholar]
- 58.Cappell M.S., Friedel D.M. Stricter national standards are required for credentialing of endoscopic-retrograde-cholangiopancreatography in the United States. World J Gastroenterol. 2019;25:3468–3483. doi: 10.3748/wjg.v25.i27.3468. [DOI] [PMC free article] [PubMed] [Google Scholar]