Abstract
Objective:
Educating medical students about buprenorphine may lessen barriers to providing treatment for opioid use disorder (OUD) by addressing stigma, removing the need to complete training while practicing, and normalizing it as a pharmacological option. We conducted a needs assessment to measure student interest in buprenorphine waiver training and pilot tested an online course with an in-person discussion for feasibility and acceptability.
Methods:
All 2019 graduating students were surveyed to assess interest in completing buprenorphine waiver training and understand in which format they preferred to receive the training. Interested students received information about a free online buprenorphine waiver course and an optional in-person case discussion with a faculty member. Baseline and follow-up surveys were used to assess the intervention.
Results:
Out of 228 students contacted, 173 (75.9%) responded to at least 1 survey. Of the 228, 62 (27.2%) responded to the initial survey asking students about receiving buprenorphine waiver training. The 166 non-responding students were sent a second survey, and 111 (66.9%) students responded. Of those 111, 29 (26.1%) indicated they forgot to respond to the first survey, and 24 (21.6%) did not see the survey. Of the 62 interested students, 41 students (66.1%) wanted a combination of online and in-person training. Of the 62, 30 (48.4%) interested students completed the online course and 10 (16.1%) attended the case discussion. While not significantly different, a higher proportion of students (88.9%) indicated being likely to prescribe buprenorphine after attending the case discussion than after completing the online course only (69.2%).
Conclusions:
This assessment suggested that most of the medical students are willing to complete a buprenorphine waiver course. Feedback indicated an in-person component could increase future prescribing more than an online-only curriculum, and additional advertising could result in higher participation.
Keywords: Buprenorphine, opioid use disorder, waiver, x-license
Introduction
Since the 1990s, rates of opioid misuse and opioid mortality in the United States have continually increased.1 Effective treatment of opioid use disorder (OUD) plays an essential role in mitigating negative outcomes.2,3 Medications for opioid use disorder (MOUD), including buprenorphine, have been shown to effectively treat patients, improving outcomes through promoting abstinence and reducing high-risk behaviors such as injection drug use.4-6 However, only 30% of patients receive MOUD following an opioid overdose, demonstrating a gap in connection to effective and evidence-based treatment for OUD.7 A 2012 national study of buprenorphine prescribing capacity estimated a treatment gap of 1.4 million patients.8 The number of clinical providers who are waivered to prescribed buprenorphine treatment is inadequate to meet the current and growing need, creating a major disconnect in care.
Many factors may contribute to the shortage of clinicians prescribing buprenorphine. As outlined in the Drug Addiction Treatment Act of 2000, prescribing buprenorphine requires physicians to undergo 8 hours of training and the completion of an application for a waiver from the Drug Enforcement Administration (DEA).9 Physicians also describe systematic barriers such as a lack of peer or institutional support, reimbursement concerns, and available mental health services.10-13 However, another contributing factor is likely stigma and bias around treating patients with OUD. While negative beliefs and attitudes toward this patient population are found in the general population14 and can begin prior to medical school, student stigma and bias can be directly addressed through educational interventions in medical school when students may alter their opinions about disease and public health. Research shows that negative attitudes lessen with increased exposure to relevant patient populations.15-17 Reaching students early in their medical career may help break down barriers to providing MOUD by addressing stigma, removing the need to receive the waiver course while actively practicing, and normalizing MOUD as a safe and significant pharmacological option.
Few studies examine efforts to address these gaps in OUD education at health professional schools around the country.18-20 We completed a needs assessment to measure student interest in buprenorphine training and in what educational format they would like to receive the training (online, in-person, or a combination). Based on the needs assessment, we then developed a pilot intervention in which a free online buprenorphine waiver training was offered to fourth-year medical students, along with an optional follow-up in-person case-based discussion with an experienced faculty member. Our objectives were to describe the feasibility of delivering effective buprenorphine training to undergraduate medical students, the resources required, and the barriers to successful implementation and participation.
Methods
Needs assessment survey
In August 2018, a needs assessment survey was sent to all fourth-year medical students in the 2019 graduating class to assess interest in completing buprenorphine waiver training and understand in what format students would like to receive the training (online, in-person, or a combination of the two). The survey included a brief description of the requirements of buprenorphine training so students were informed prior to indicating their interest level. Only the students who indicated interest in the needs assessment survey were sent information about how to register for an online buprenorphine course and participate in an in-person case discussion (described below). Two reminder emails were sent at 1 month and 2 months following the initial course invitation to encourage participation.
Those students who did not respond to the needs assessment survey were not eligible to participate in the online course or in-person case discussion. A follow-up survey was sent to these non-responders in March 2019 to understand why they did not indicate interest in participating to determine if the content did not seem relevant, if students felt they did not have enough time to complete the training, or if they simply overlooked the initial survey email. An electronic US$5 Starbucks gift card was used to incentivize student responses.
Training intervention
The intervention consisted of two parts: (1) a free online buprenorphine training course through BupPractice,21 which contained the mandatory 8 hours of training required to receive the buprenorphine waiver, and (2) an optional in-person case discussion with a faculty member. Training materials through the online course were written at the level appropriate for practicing providers because, at the time, there was no available training option tailored to medical students. The online training was delivered through downloadable PDF readings with case-based knowledge checks interspersed. Topics covered included the following: screening, diagnosing and assessing patients with OUD, various buprenorphine formulations, induction and maintenance procedures, clinical management practices, and federal regulations. As part of the course, students were required to pass a post-test and complete a survey regarding the effectiveness of BupPractice. Students were instructed to complete the online waiver training prior to participating in the patient case discussion.
The optional in-person patient case discussion was held in March 2019 for 1.5 hours. The discussion included 4 written patient cases, ranging from a complex chronic pain patient to a patient with polysubstance use. Discussion was led by a faculty member with expertise in treating patients with OUD and complex pain and facilitated using pre-determined questions based on each patient’s scenario. Cases were written in a way to facilitate discussion about both patient and provider stigma and to work through difficult treatment scenarios. Time was given at the end of the discussion for individual student questions. To encourage participation in the case discussion, the study coordinator ensured students would be excused from their current rotations.
Evaluation surveys
A survey was fielded after students completed the online course to assess likelihood to prescribe buprenorphine after completing the online course but prior to attending the case discussion. The survey also asked about what resources students wanted to increase their likelihood to prescribe in the future. The survey included steps for registering for the in-person patient case discussion.
Participants were sent a survey immediately following the case discussion, which included closed- and open-ended questions, to gain feedback about future prescribing likelihood, resources needed to prescribe, the effectiveness of the discussion, and suggestions for improvement.
All variables, with the exception of prescribing likelihood, were evaluated descriptively. Prescribing likelihood was compared in both the pre- and the post-discussion surveys using a paired samples t-test. All data were compiled and analyzed using R. The University of Michigan Institutional Review Board approved this study and deemed it exempt.
Results
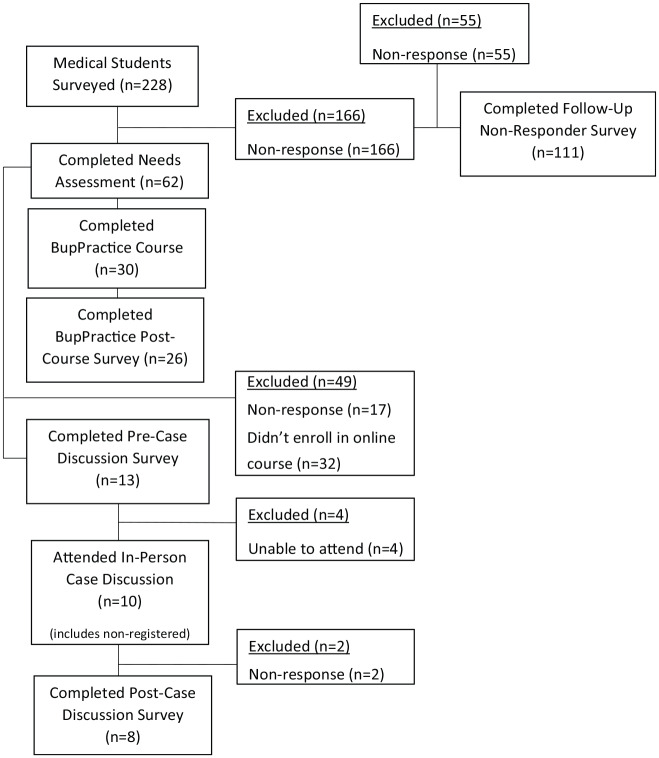
Out of 228 students contacted, 173 (75.9%) responded to at least 1 survey (Figure 1). Of the 228, 62 (27.2%) responded to the needs assessment survey where students were asked whether they would be interested in receiving the buprenorphine waiver training, and all respondents indicated they were interested. Of the 62 interested students, 30 (48.4%) completed the online course, 13 (21.0%) completed the pre-discussion survey, and 9 (14.5%) students registered for the case discussion. Of the 62, 10 (16.1%) students attended the in-person discussion (1 student attended who did not register in advance). Of the 10, 8 (80.0%) students who attended the in-person discussion completed the post-discussion survey.
Figure 1.
Participant flow diagram.
Of the 166 students, 111 (66.9%) who did not respond to the needs assessment survey completed the second survey they received about their reasoning for not wanting to participate in buprenorphine waiver training. Of those 111, 29 (26.1%) indicated they did not express interest in the buprenorphine waiver course because they forgot to respond to the survey (Table 1). An additional 24 (21.6%) students reported that they did not respond because they did not see the initial survey email, and 23 (20.7%) students indicated they did not have time to complete the training in addition to their other curricular requirements. Only a small portion of students reported they did not foresee the need to prescribe buprenorphine (9, 8.1%) or intend to care for patients with OUD (4, 3.6%) in their future. Students were given the option to provide open-ended feedback as well; however, these comments were infrequent and tended to reiterate answer choices provided.
Table 1.
Student reasons for not responding to initial interest survey.
| Reason | Frequency (N = 111) |
% |
|---|---|---|
| Forgot to respond | 29 | 26.1 |
| Did not see the email | 24 | 21.6 |
| Do not have time to complete the training | 23 | 20.7 |
| Do not foresee the need | 9 | 8.1 |
| Feasibility concerns (scheduling, being in town) | 7 | 6.3 |
| Disregard or delete all surveys | 5 | 4.5 |
| Wanted to take at another time | 5 | 4.5 |
| Do not intend to care for patients with OUD | 4 | 3.6 |
| Feel like have adequate training for treating OUD | 3 | 2.7 |
| Did not understand what email was asking | 1 | 0.9 |
| Do not remember | 1 | 0.9 |
Abbreviation: OUD, opioid use disorder.
In the initial interest survey, which also investigated student preferences for educational methods, students were allowed to select multiple modalities that they felt would be useful. Of the 62 interested students, 42 (67.7%) indicated support for receiving the buprenorphine training 100% online, and 41 (66.1%) indicated they would support a combination of in-person and online training (Table 2). Only 21 (33.9%) students indicated support for a 100% in-person format.
Table 2.
Course format preferences (students allowed to select multiple options).
| Course format option | Frequency (N = 62) |
% |
|---|---|---|
| 100% online | 42 | 67.7 |
| Combination of in-person and online training | 41 | 66.1 |
| 100% in-person | 21 | 33.9 |
Of the 30 students, 26 (86.7%) who completed the BupPractice course also took the post-course survey following the completion of the online training. All respondents either agreed or strongly agreed that the course achieved its stated learning objectives and was a useful learning experience. When asked if they felt the PDFs were an effective way of teaching the subject matter, 2 students (7.7%) disagreed, 7 students (26.9%) were neutral, and 17 students (65.4%) agreed.
Of the 13 students who responded to the pre-case discussion survey, 8 (61.5%) indicated they were likely or very likely to prescribe buprenorphine after completing the online course (Figure 1). Most of the students indicated a need for additional resources prior to prescribing in the future: 10 of 13 (76.9%) indicated they would need resources for behavioral counseling and 9 of 13 (69.2%) desired case management support.
Following the case discussion, 7 of 8 (87.5%) students indicated they were likely or very likely to prescribe buprenorphine, a higher proportion than before completing the case discussion, although this difference was not statistically significant. All students agreed that the in-person discussion made them more confident in their ability to manage a patient on buprenorphine even if they did not go on to prescribe the medication themselves. However, most students still felt the need for additional resources to prescribe: 5 (62.5%) felt they needed resources for behavioral counseling, a non-significantly smaller proportion than prior to the case discussion, and 6 (75.0%) felt the need for supervision from a waivered attending. Only half of students agreed when asked if they felt the in-person discussion heightened their awareness of the stigma and bias associated with treating patients with OUD while 3 (37.5%) were neutral and 1 (12.5%) disagreed.
Feedback from open-ended questions on the post-discussion survey indicated that students felt the in-person discussion was helpful and valuable. Several students noted they appreciated being able to ask questions and discuss the difficulties of prescribing buprenorphine with an experienced faculty member. One student noted that the discussion added “a lot to the more generic online content,” and another noted that the faculty member did well with “reassuring us and encouraging us that this is something positive we can do for our patients.” Three students reported wanting more time to discuss the patient cases, with one indicating a half-day would be appropriate.
Conclusions
This needs assessment and pilot intervention demonstrated the feasibility and acceptability of incorporating an online buprenorphine waiver course and patient case discussion into medical school education. More than one-quarter of all students in the 2019 graduating class expressed interest in completing the buprenorphine waiver training. Of those who did not respond to the initial survey, most students reported not participating simply because they missed or forgot about the email while only a small proportion of students did not foresee the need to prescribe buprenorphine in their future. Combined, these findings demonstrate that the incorporation of this training was both feasible and appropriate within a 4-year medical school curriculum.
In addition, half of those who expressed interest in buprenorphine training went on to actually complete the online course and roughly one-third who completed the online course also participated in the case discussion. While not statistically significant, a higher proportion of students reported being likely to prescribe buprenorphine after participating in the in-person case discussion than after only completing the online course, indicating the in-person component was effective in increasing student confidence in prescribing. That being said, more than half of students who completed the case discussion still reported needing access to behavioral counseling before prescribing, which is a sentiment echoed by inexperienced waivered physicians13 despite the demonstrated effectiveness of treatment in primary care alone.5,6 While the case discussion was set up to discuss controversial topics where patients may experience stigma, such as non-medication versus medication treatment and addressing polysubstance use during treatment, half of the students did not feel that the case discussion increased their awareness of stigma. This may have been because the question evaluating stigma was too broad and did not ask specifically about each of the scenarios discussed or because students who elected to participate were highly engaged with treating this patient population and already aware of stigma surrounding treatment. Regardless, future educational efforts should be made to better define stigma for students and address strategies to mitigate it during treatment.
Our study had multiple limitations. First, as our study was conducted with a modest sample at a large Midwest academic teaching hospital, our results are not representative of all medical students and this type of teaching intervention may not be feasible at all institutions. In addition, the online training students completed was designed for and written at the level of a practicing physician, so it may not be the most effective type of training for medical students. The in-person component was added to help mitigate this limitation and allow for a faculty member to discuss questions and concerns students had following the online component. Adapting the online curriculum to the level of a medical student could increase the effectiveness of the training. Because this intervention was only piloted and evaluated with fourth-year students, we did not measure student interest for this curriculum or potential for larger impact on their attitudes earlier in their medical education. In the future, this curriculum will be expanded to include all third-year medical students as they will have completed their basic clinical clerkships and likely have been exposed to buprenorphine at this point in their schooling.
Future assessments will also gather information on both student knowledge of and attitudes toward patients with OUD before and after completing the curriculum. While the response rate for the initial interest survey was low, we corrected for this by fielding a non-responder survey to understand why students were not interested in completing buprenorphine waiver training. A significant portion of students reported not expressing interest simply because the sign-up was forgotten or overlooked. Improving the promotion of such an opportunity and expanding outreach efforts have the potential to elicit more interest from medical students. Of note, one-fifth of students indicated time constraints as their reason for not participating, which could be addressed by finding a way to provide protected time in students’ schedules if they choose to participate in waiver training. More effort could also be dedicated to engaging students across all medical specialties as the likelihood is high that they will encounter patients with OUD in their future practices.
Based, in part, on feedback from the graduating class that participated in this project, members of the study team are currently implementing various training components across all 4 years of medical school training. All students will be required to complete an online, video-based buprenorphine waiver training course with the goal of increasing students’ engagement with the content and perceived effectiveness by making it more interactive. All students will also participate in a half-day in-person workshop about substance use disorder that includes both didactics and small-group case discussion to directly address stigma toward treating patients with addiction. Additional information about behavioral therapy options will also be incorporated into the workshop to equip students with supplementary tools that work synergistically with the use of MOUD. Lessons will also reinforce that treatment is effective in primary care to help quell student concerns about the need for additional counseling resources as a prerequisite to prescribing.
The recent creation of national initiatives to train providers in OUD treatment, such as the Provider Clinical Support System, demonstrates the relevance and urgency of increasing access to MOUD in the larger conversation about public health and medical student education.22 Other medical schools19 and residency programs23 have implemented models that integrate the buprenorphine waiver course into their curricula with the goals of alleviating the physician burden of obtaining a waiver while practicing and expanding access to care for OUD.20 Increasing the number of trained residents and attending physicians is imperative to ensure that advances made in medical education are not lost when learners make the transition into residency. As demonstrated, graduating medical students see a need for being able to prescribe buprenorphine in their future careers and want to receive waiver training as part of their medical school education. Students are open to completing this training in an online format along with an in-person supplementation. This could be easily implemented as a sustainable option for medical schools, where there may be limited resources and educators, rather than building all in-person sessions throughout the entirety of the curriculum.
Acknowledgments
The authors would like to thank Maripat Metcalf, PhD, MPH, and Clinical Tools, Inc. for allowing the medical students to complete the BupPractice online buprenorphine training for free and for sharing their post-course survey data with the team.
Footnotes
Funding:The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the Substance Abuse and Mental Health Services Administration (grant no. TI-H79TI081658-01).
Declaration of Conflicting Interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: JT, SS, GW, KC, and PL contributed to the conception and design of the work. JT, SS, and CM contributed to data acquisition, analysis and interpretation of data. JT and SS drafted the manuscript. All authors critically revised the manuscript for important intellectual content and approved it for publication.
Ethical approval: University of Michigan Institutional Review Board deemed this study exempt as part of study # HUM00155840.
ORCID iD: Jennifer Thomas  https://orcid.org/0000-0001-6301-8521
https://orcid.org/0000-0001-6301-8521
References
- 1. 2017 NSDUH Annual National Report—CBHSQ, https://www.samhsa.gov/data/report/2017-nsduh-annual-national-report. Accessed June 16, 2019.
- 2. Kolodny A, Courtwright DT, Hwang CS, et al. The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559-574. doi: 10.1146/annurev-publhealth-031914-122957. [DOI] [PubMed] [Google Scholar]
- 3. Understanding the Epidemic—Drug Overdose—CDC—Injury Center, https://www.cdc.gov/drugoverdose/epidemic/index.html. Published December 19, 2018. Accessed June 16, 2019.
- 4. Schuckit MA. Treatment of opioid-use disorders. N Engl J Med. 2016;375:1596-1597. [DOI] [PubMed] [Google Scholar]
- 5. Amato L, Minozzi S, Davoli M, Vecchi S, Ferri M, Mayet S. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst Rev. 2008;10:CD004147. [DOI] [PubMed] [Google Scholar]
- 6. Lagisetty P, Klasa K, Bush C, Heisler M, Chopra V, Bohnert A. Primary care models for treating opioid use disorders: what actually works? A systematic review. PLoS ONE. 2017;12:e0186315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Larochelle MR, Bernson D, Land T, et al. Medication for opioid use disorder after nonfatal opioid overdose and association with mortality: a cohort study. Ann Intern Med. 2018;169:137-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Jones CM, Campopiano M, Baldwin G, McCance-Katz E. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am J Public Health. 2015;105:e55-e63. doi: 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Drug Addiction Treatment Act of 2000, H.R. 2634, 106th Cong. (2000).
- 10. Hutchinson E, Catlin M, Andrilla HA, Baldwin L, Rosenblatt RA. Barriers to primary care physicians prescribing buprenorphine. Ann Fam Med. 2014;12:128-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Andrilla HA, Coulthard C, Larson EH. Barriers rural physicians face prescribing buprenorphine for opioid use disorder. Ann Fam Med. 2017;15:359-362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Haffajee RL, Bohnert ASB, Lagisetty PA. Policy pathways to address provider workforce barriers to buprenorphine treatment. Am J Prev Med. 2018;54: S230-S242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Netherland J, Botsko M, Egan JE, et al. Factors affecting willingness to provide buprenorphine treatment. J Subst Abuse Treat. 2009;36:244-251. doi: 10.1016/j.jsat.2008.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Barry CL, McGinty EE, Pescosolido BA, Goldman HH. Stigma, discrimination, treatment effectiveness, and policy: public views about drug addiction and mental illness. Psychiatr Serv. 2014;65:1269-1272. doi: 10.1176/appi.ps.201400140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Weinstein SM, Laux LF, Thornby JI, et al. Medical students’ attitudes toward pain and the use of opioid analgesics: implications for changing medical school curriculum. South Med J. 2000;93:472-478. [PubMed] [Google Scholar]
- 16. Mukherjee R, Fialho A, Wijetunge A, Checinski K, Surgenor T. The stigmatisation of psychiatric illness: the attitudes of medical students and doctors in a London teaching hospital. Psychiatr Bull. 2002;26:178-181. doi: 10.1192/pb.26.5.178. [DOI] [Google Scholar]
- 17. Silins E, Conigrave KM, Rakvin C, Dobbins T, Curry K. The influence of structured education and clinical experience on the attitudes of medical students towards substance misusers. Drug Alcohol Rev. 2007;26:191-200. [DOI] [PubMed] [Google Scholar]
- 18. Dumenco L, Monteiro K, Collins S, et al. A qualitative analysis of interprofessional students’ perceptions towards patients with opioid use disorder after a patient panel experience. Subst Abus. 2019;40:2-7. doi: 10.1080/08897077.2018.1546262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Monteiro K, Dumenco L, Collins S, et al. An interprofessional education workshop to develop health professional student opioid misuse knowledge, attitudes, and skills. J Am Pharm Assoc 2017;57:S113-S117. doi: 10.1016/j.japh.2016.12.069. [DOI] [PubMed] [Google Scholar]
- 20. McCance-Katz EF, George P, Scott NA, Dollase R, Tunkel AR, McDonald J. Access to treatment for opioid use disorders: medical student preparation. Am J Addict. 2017;26:316-318. doi: 10.1111/ajad.12550. [DOI] [PubMed] [Google Scholar]
- 21. BupPractice. Buprenorphine training activity for residents. https://bup.clinicalencounters.com/trainings/physicians-bup/. Published April 15, 2019. Accessed September 19, 2019.
- 22. SAMHSA. Providers’ Clinical Support System for Medication Assisted Treatment (PCSS-MAT). https://www.samhsa.gov/providers-clinical-support-system-medication-assisted-treatment. Published April 4, 2019. Accessed September 26, 2019.
- 23. Kunins HV, Sohler NL, Giovanniello A, Thompson D, Cunningham CO. A buprenorphine education and training program for primary care residents: implementation and evaluation. Subst Abus. 2013;34:242-247. doi: 10.1080/08897077.2012.752777. [DOI] [PMC free article] [PubMed] [Google Scholar]