Abstract
Background:
Little is known about the long-term prognosis of osteochondral lesions of the talus (OLTs) after nonoperative treatment.
Purpose:
To evaluate the clinical and radiological long-term results of initially successfully treated OLTs after a minimum follow-up of 10 years.
Study Design:
Case series; Level of evidence, 4.
Methods:
Between 1998 and 2006, 48 patients (50 ankles) with OLTs were successfully treated nonoperatively. These patients were enrolled in a retrospective long-term follow-up, for which 24 patients could not be reached or were available only by telephone. A further 2 OLTs (6%) that had been treated surgically were excluded from the analysis and documented as failures of nonoperative treatment. The final study group of 22 patients (mean age at injury, 42 years; range, 10-69 years) with 24 OLTs (mean size, 1.4 cm2; range, 0.2-3.8 cm2) underwent clinical and radiological evaluation after a mean follow-up of 14 years (range, 11-20 years). Ankle pain was evaluated with a visual analog scale (VAS), ankle function with the American Orthopaedic Foot and Ankle Society (AOFAS) score, and sports activity with the Tegner score. Progression of ankle osteoarthritis was analyzed based on plain ankle radiographs at the initial presentation and the final follow-up according to the Van Dijk classification.
Results:
At final follow-up, the 24 cases (ie, ankles) showed a median VAS score of 0 (IQR, 0.0-2.25) and a median AOFAS score of 94.0 (IQR, 85.0-100). Pain had improved in 18 cases (75%), was unchanged in 3 cases (13%), and had increased in 3 cases (13%). The median Tegner score was 4.0 (IQR, 3.0-5.0). Persistent ankle pain had led to a decrease in sports activity in 38% of cases. At the final follow-up, 11 cases (73%) showed no progression of ankle osteoarthritis and 4 cases (27%) showed progression by 1 grade.
Conclusion:
Osteochondral lesions of the talus that successfully undergo an initial nonoperative treatment period have minimal symptoms in the long term, a low failure rate, and no relevant ankle osteoarthritis progression. However, a decrease in sports activity due to sports-related ankle pain was observed in more than one-third of patients.
Keywords: osteochondral lesion, talus, ankle, nonoperative treatment, long-term prognosis
Osteochondral lesions of the talus (OLTs) have become an umbrella term for various conditions such as osteochondral fractures, osteochondritis dissecans, and osteochondral defects. OLTs are defined as lesions that involve the articular cartilage and the subchondral bone of the talus.15 Trauma is the most important etiological factor for OLTs. A history of ankle trauma has been reported in 93% to 98% of lateral talar dome lesions and in 61% to 70% of medial talar dome lesions.9,20,22
Loose osteochondral fragments of the talus may cause catching or locking symptoms; however, these symptoms are relatively rare in the ankle compared with other joints.8 The majority of patients with an OLT have vague symptoms, such as diffuse ankle pain and swelling.23 OLTs are commonly seen with other ankle injuries; chondral lesions in the talus were arthroscopically detected in 61% of 84 patients with an acute ankle fracture12 and in 55% of 148 patients with chronic ankle instability.10 Because OLTs may not appear on plain radiographs, cross-sectional imaging, such as magnetic resonance imaging (MRI) or computed tomography, should be performed in patients with prolonged symptoms to detect these lesions and to exclude other foot and ankle conditions.5
Nonoperative treatment of OLTs includes activity reduction, nonsteroidal anti-inflammatory drugs, bracing, physical therapy, protected weightbearing, or even temporary immobilization, depending on the severity of the symptoms.2,13,18,19 Despite limited evidence, a recent review proposed that the initial treatment attempt should be nonoperative.8 The nonoperative approach is also supported by the fact that no clear recommendation for a specific surgical procedure can be made based on the current evidence.7 However, even if patients complete a nonoperative regimen with sufficient pain relief, there is scant knowledge of the long-term success of this treatment.11
The aim of this study was to evaluate the clinical and radiological long-term outcomes of OLTs after successful nonoperative treatment in the initial phase. The enrolled patients had been investigated previously in a midterm follow-up with good to excellent results.11 We hypothesized that these patients would have a favorable long-term prognosis.
Methods
Participants
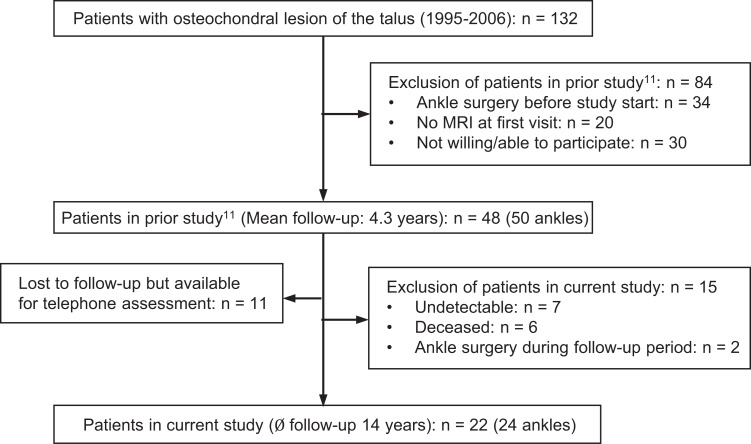
We retrospectively enrolled a study group of 48 patients (50 ankles) who had undergone successful nonoperative treatment for symptomatic OLTs between 1998 and 2006. These patients had been investigated previously at our institution after a midterm follow-up of 4 years.11 The patient selection process is shown in Figure 1. Of the initial 132 eligible patients, 34 (26%) had undergone ankle surgery before the start of the prior study. All of them had attempted nonoperative treatment for more than 6 months, and all had experienced treatment failure. Another 50 patients were excluded because they did not have MRI scans during their first visit or they did not consent to be included. The remaining 48 patients (50 ankles) achieved successful pain reduction with a nonoperative treatment regimen consisting of temporary activity reduction and pain medication within a 6-month period and did not receive any surgery involving the osteochondral lesion before the reported midterm follow-up of our prior study.11
Figure 1.
Flowchart showing the patient selection process. MRI, magnetic resonance imaging.
During the enrollment period for the current study, all 48 study participants had completed a minimum follow-up of 10 years after the initial consultation in our outpatient clinic. Of these, 11 patients (23%) were not willing to attend an examination in-person but were interviewed by telephone, 7 patients (15%) could not be located, and 6 patients (13%) had died. All patients who had undergone a surgical procedure for OLT during the follow-up period were excluded from the final analysis and their treatments were documented as failures. This was the case in 2 of the 35 available patients (6%). The OLTs had been addressed with autologous matrix-induced chondrogenesis at 4.3 years and 6.1 years, respectively, after the initial consultation.
The final study group of 22 patients (24 ankles, in the following referred to as “cases”) attended a clinical and radiological follow-up examination during 2018. The mean follow-up period was 14 years (range, 11-20 years). There were 13 males and 9 females with a mean age of 42 years (range, 10-69 years) and a mean body mass index (BMI) of 26 kg/m2 (range, 19-36 kg/m2) at the initial visit. Of the 24 cases, 22 cases (92%) had at least 1 previous ankle trauma before symptom onset (Table 1).
Table 1.
Demographic Data and Clinical and Radiological Long-Term Results of 24 OLTs After Initial Successful Nonoperative Treatmenta
| Case No. | Sex | Age, y | BMI, kg/m2 | Trauma History | OLT Location | OLT Type | OLT size, cm2 | FU, y | VAS at FU | AOFAS at FU | Tegner at FU | Van Dijk, Initial | Van Dijk at FU |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 3 | M | 39 | 27 | Yes | Medial | 1 | 1.2 | 13 | 1 | 96 | 5 | I | I |
| 4 | F | 57 | 26 | No | Medial | 1 | 2.0 | 16 | 0 | 92 | 4 | NA | II |
| 6 | M | 58 | 36 | No | Medial | 5 | 3.8 | 14 | 0 | 85 | 0 | II | II |
| 10 | M | 37 | 23 | Yes | Medial | 1 | 2.2 | 14 | 0 | 96 | 3 | NA | 0 |
| 11 | M | 38 | 26 | Yes | Lateral | 1 | 0.5 | 14 | 0 | 100 | 5 | NA | I |
| 12 | M | 28 | 25 | Yes | Lateral | 1 | 1.1 | 15 | 2 | 100 | 5 | 0 | 0 |
| 13 | M | 28 | 25 | Yes | Lateral | 1 | 0.8 | 15 | 2 | 90 | 5 | I | I |
| 18 | F | 56 | 30 | Yes | Medial | 1 | 1.0 | 14 | 0 | 100 | 3 | 0 | I |
| 19 | M | 59 | 32 | Yes | Lateral | 1 | 0.2 | 14 | 0 | 100 | 3 | NA | II |
| 21 | M | 39 | 23 | Yes | Medial | 5 | 3.6 | 11 | 0 | 100 | 5 | 0 | I |
| 23 | M | 46 | 29 | Yes | Lateral | 1 | 0.9 | 14 | 0 | 100 | 4 | NA | I |
| 24 | M | 34 | 28 | Yes | Medial | 5 | 1.7 | 14 | 0 | 87 | 4 | 0 | I |
| 26 | M | 69 | 24 | Yes | Medial | 1 | 0.9 | 13 | 8 | 64 | 3 | 0 | I |
| 27 | F | 10 | 22 | Yes | Central | 1 | 0.5 | 16 | 0 | 100 | 5 | 0 | 0 |
| 32 | F | 40 | 32 | Yes | Medial | 5 | 0.2 | 14 | 6 | 38 | 0 | 0 | 0 |
| 33 | F | 49 | 21 | Yes | Medial | 1 | 2.2 | 15 | 1 | 86 | 4 | I | I |
| 34 | M | 36 | 27 | Yes | Medial | 1 | 1.2 | 14 | 4 | 82 | 3 | I | I |
| 37 | M | 30 | 21 | Yes | Lateral | 1 | 0.4 | 20 | 1 | 85 | 3 | 0 | 0 |
| 38 | F | 52 | 26 | Yes | Medial | 5 | 0.7 | 13 | 0 | 97 | 4 | 0 | 0 |
| 42 | F | 34 | 21 | Yes | Medial | 3 | 1.1 | 16 | 3 | 85 | 4 | NA | I |
| 43 | F | 34 | 21 | Yes | Medial | 3 | 2.1 | 16 | 3 | 85 | 4 | NA | I |
| 45 | F | 11 | 19 | Yes | Medial | 3 | 1.5 | 13 | 0 | 100 | 9 | 0 | 0 |
| 46 | F | 64 | 29 | Yes | Medial | 3 | 1.3 | 12 | 3 | 80 | 4 | NA | II |
| 48 | M | 55 | 29 | Yes | Medial | 1 | 3.1 | 13 | 0 | 100 | 4 | NA | II |
aAge and BMI are recorded from the initial consultation. AOFAS, American Orthopaedic Foot and Ankle Society score; BMI, body mass index; F, female; FU, follow-up; M, male; NA, not available; OLT, osteochondral lesion of the talus; VAS, visual analog scale.
The study was approved by the local research ethics committee. All patients received oral and written information, and all signed written informed consent.
Outcome Measures
Ankle pain was documented with a visual analog scale (VAS; 0-10 points). Ankle function was assessed with the American Orthopaedic Foot and Ankle Society (AOFAS; 0-100 points) score, and the results were graded as excellent (90-100 points), good (80-89), fair (70-79), or poor (<70). Sports activity was measured with the Tegner score (0-10 points). Patients were asked whether they had given up their previous sports activities or profession due to persistent ankle pain.
All OLTs had been confirmed by MRI at the initial visit. The location, coronal length, sagittal length, and depth of the lesion were measured as previously reported.11 The surface area of the lesion was calculated using the ellipse formula6: Area = Coronal Length × Sagittal Length × 0.79. The lesions were classified according to the classification system of Loomer et al13 (type 1, subchondral compression; type 2, partially detached but undisplaced fragment; type 3, completely detached but undisplaced fragment; type 4, displaced fragment; type 5, formation of a subchondral cyst).
All patients underwent plain weightbearing radiographs of the ankle (lateral and mortise views). Ankle osteoarthritis was graded based on the classification system by Van Dijk et al21 (grade 0, normal joint or subchondral sclerosis; grade I, osteophytes without joint space narrowing; grade II, joint space narrowing with or without osteophytes; grade III, [sub]total disappearance or deformation of the joint space).
Statistical Analysis
Demographic analysis included measurements of demographic and MRI data in means, standard deviations, and ranges. Clinical outcome variables showed a skewed distribution and were thus presented as median and interquartile range (IQR). Correlations between potential negative predictive factors (sex, age, BMI, stage and size of the lesion) and the clinical outcome at the final follow-up (VAS and AOFAS scores) were assessed with Spearman rank correlation tests. We did not calculate the correlations for OLT location and trauma history given the small case numbers in those subgroups. Statistical analysis was conducted with SPSS Statistics for Windows (version 25.0; IBM Corp). The level of significance was set at α = .05.
Results
Clinical Assessment
The final study group of 22 patients (24 ankles [cases]) showed a median VAS of 0 points (IQR, 0.0-2.25 points), with 88% either being pain-free (VAS 0; n = 13) or having only mild symptoms (VAS 1-3; n = 8). The patients showed further pain reduction from the midterm (median VAS, 1 point; IQR, 0.75-2.25 points) to the current long-term follow-up. Compared with the initial presentation, pain was improved in 18 cases (75%), unchanged in 3 cases (13%), and increased in 3 cases (13%).
The median AOFAS score was 94.0 points (IQR, 85.0-100 points), with good or excellent results in 22 cases (92%). The median Tegner score was 4.0 points (IQR, 3.0-5.0 points). In 9 cases (38%), a decrease in sports activity attributable to persistent ankle pain was reported. There were 2 patients (case numbers 6 and 32) who had to change their profession because of persistent ankle pain. The clinical results did not correlate with the radiological findings. Case 32 had by far the worst clinical outcome at the final follow-up (VAS, 6 points; AOFAS, 38 points) but showed only a small OLT (0.2 cm2) and no radiological osteoarthritis (Van Dijk grade 0). In contrast, case 6 had good clinical results (VAS, 0 points; AOFAS, 85 points) but presented with the largest OLT (3.8 cm2) and osteoarthritic changes (Van Dijk grade 2) at initial presentation. These changes remained stable until the final follow-up.
Telephone Assessment
In 11 cases, with a mean age of 53 years (range, 33-71 years) and a mean BMI of 27 kg/m2 (range, 21-35 kg/m2), patients were not willing to attend a clinical evaluation but were available for a telephone survey after a mean follow-up of 16 years (range, 13-17 years). None had undergone an operative procedure addressing the OLT during the follow-up period. The median VAS score was 0 points (IQR, 0.0-2.5 points), showing a slight improvement compared with the midterm follow-up (median VAS, 1 point; IQR, 0.25-1.0 points).
Radiological Assessment
In total, 17 OLTs (71%) were located on the medial talar dome, 6 lesions (25%) were located on the lateral talar dome, and 1 lesion (4%) was located centrally. There were 15 type 1 lesions, 4 type 3 lesions, and 5 type 5 lesions. None of the patients showed a type 2 or 4 lesion (Table 1). The OLTs had a mean ± SD coronal extension of 10.3 ± 4.7 mm, sagittal extension of 16.0 ± 5.4 mm, and depth of 8.6 ± 3.7 mm. The mean surface area of the OLT was 1.4 cm2 (range, 0.2-3.8 cm2).
At the final follow-up, 7 cases (29%) showed no signs of ankle osteoarthritis, 12 cases (50%) were grade I, 5 cases (21%) were grade II, and 0 cases showed grade III osteoarthritis. A median Van Dijk grade of I (range, 0-II) was calculated. In 15 of the 24 cases, plain radiographs had been performed at the initial consultation. At the final follow-up, 11 cases (73%) showed no osteoarthritis progression, and 4 (27%) showed a progression by 1 grade (Figures 2 -4).
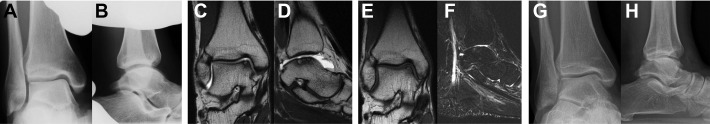
Figure 2.
Images for a 39-year-old man (case no. 3). (A, B) Initial ankle radiographs show an osteochondral lesion of the talus (OLT) at the lateral talar dome; the ankle joint shows grade I osteoarthritic changes. (C, D) Initial magnetic resonance imaging scans confirm OLT. Radiographs at (E, F) midterm and (G, H) long-term follow-up show unchanged OLT and stable grade I osteoarthritis after a 13-year follow-up.
Figure 3.
Images for a 28-year-old man (case no. 12). (A, B) Initial ankle radiographs, suspected of an osteochondral lesion of the talus (OLT) at the medial talar dome and no osteoarthritic changes. (C, D) Initial magnetic resonance imaging (MRI) scans confirm OLT diagnosis. (E, F) MRI scans at midterm follow-up show a slight decrease in size of the lesion. (G, H) Long-term radiographs show a persistent OLT and no osteoarthritis after a 15-year follow-up.
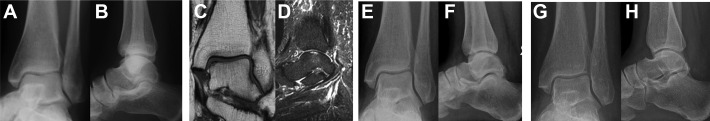
Figure 4.
Images for a 56-year-old woman (case no. 18). (A, B) Initial radiographs without any detectable osteochondral lesion of the talus (OLT); the ankle joint shows no osteoarthritic changes. (C, D) Magnetic resonance imaging scans reveal an OLT at the medial talar dome. (E, F) Unchanged radiographs at midterm follow-up. (G, H) Long-term radiographs show development of grade I osteoarthritis after a 14-year follow-up.
Prognostic Factors
When Spearman analysis was used to assess for correlation between different possible prognostic factors and outcome scores, older age at initial consultation (Spearman = –0.52; P = .01) was found to have a negative correlation with the Tegner score at the final follow-up. This correlation may indicate that older patients are generally more likely to have a lower sports activity level (Table 2).
Table 2.
Spearman Analysis to Assess for Correlation Between Different Prognostic Factors and Clinical Outcome Scoresa
| VAS Score | AOFAS Score | Tegner Score | ||||
|---|---|---|---|---|---|---|
| Spearman Correlation | P Value | Spearman Correlation | P Value | Spearman Correlation | P Value | |
| Age | –0.05 | .79 | –0.17 | .42 | –0.52 | .01b |
| BMI | –0.15 | .47 | 0.02 | .93 | –0.34 | .10 |
| OLT size | –0.19 | .37 | –0.02 | .92 | 0.08 | .71 |
| OLT stage | 0.00 | .99 | –0.28 | .18 | –0.06 | .77 |
aAOFAS, American Orthopaedic Foot and Ankle Society; BMI, body mass index; OLT, osteochondral lesion of the talus; VAS, visual analog scale.
bP < .05.
Discussion
In this study, we report on the long-term clinical and radiological results of patients with an OLT who initially underwent successful nonoperative treatment. We previously found that 86% of these patients were either pain-free or had only mild symptoms (VAS score, 1-3) at midterm follow-up of 4.3 years.11 The most important finding of this study is that only 2 patients (6%) needed a surgical procedure for their OLT in the long-term if they initially completed a nonoperative treatment phase successfully. Furthermore, 88% of our study participants who did not receive any surgery remained minimally symptomatic (VAS score, 0-3) until the final follow-up of 14 years. However, more than a third of the patients had to reduce their sports activity due to persistent ankle pain, an adverse finding of which patients must be informed. We found a correlation between older age at initial consultation and lower Tegner scores at the final follow-up. Since sports activity naturally decreases with increasing age, we interpret age as an independent risk factor for lower levels of sports activity. We therefore recorded the reduced sports activity only as such if the decrease resulted from persistent ankle pain during the activity. Nevertheless, there is still a chance that some patients may have developed ankle pain due to age-related degenerative changes in the ankle joint, independently from the osteochondral lesion. We did not find any negative prognostic factors that may have influenced the clinical success rate of nonoperative treatment for OLTs; however, this may be due to the small size of the cohort. Progression of ankle osteoarthritis by 1 grade was seen in 27% of the cases, whereas 73% of the cases showed no deterioration. The minimal progression of ankle osteoarthritis may also be interpreted as the natural course in a patient group with a mean age of 42 years at first presentation, thus a mean age of 56 years at the 14-year follow-up.
Overall, limited evidence is available regarding the outcome of nonoperatively treated OLTs. Most studies date back to at least 2 decades, had small case numbers, and lacked outcome scores and staging of the OLTs.1,3,4,9,14,16,17 Furthermore, they reported on only the overall outcome of nonoperatively treated OLTs, not the lesions that had undergone initial successful nonoperative treatment. A meta-analysis of 14 studies including 201 OLTs found nonoperative treatment to be successful in only 45% of the patients.20 These findings are in contrast to another retrospective study by Bauer et al,1 not included in the meta-analysis, who reported on the long-term outcome of nonoperatively treated OLTs. Those authors investigated 23 cases after a follow-up of 20 years and found good to excellent clinical results in 80%. Only 1 patient experienced failed nonoperative treatment, and 1 case developed ankle osteoarthritis. Shearer et al19 reported good to excellent results in 62% of 26 cases, but 50% showed degenerative changes and 15% experienced treatment failure. In a recent study with a follow-up of 6 years, Seo et al18 found that 11% of the 244 reviewed OLTs had been treated surgically, but only 3% because of increased of symptoms. Those investigators noted a significant reduction of VAS scores, improvement of AOFAS and 36-Item Short Form Health Survey scores, and no progression of ankle osteoarthritis for nonoperatively treated patients.
Our study has several limitations. First, we reported on only the relative pain evolution because clinical scores at the initial consultation were not available due to the retrospective study design. In this way, we tried to avoid recall bias as far as possible. Second, all the included patients had been successfully treated nonoperatively but the duration of their symptoms before initiation of the nonoperative treatment in our outpatient clinic had not been recorded. Therefore, we could not further analyze the success rates of nonoperative treatment of acute versus chronic lesions. Third, the mean age of this study group (42 years) was certainly higher compared with many previous reports on operatively treated osteochondral talar lesions. This may have introduced a selection bias because older patients demonstrate a lower sports activity level. Notably, however, our risk factor analysis did not show that older age of the patients correlated with a better clinical outcome. Fourth, the study lacks an operatively treated control group of patients with similar demographic data and lesion characteristics. We are well aware of the fact that this is a very selected group of patients with OLTs who underwent successful nonoperative treatment in the early phase. These patients might have had lower initial pain scores than others who underwent operative treatment after a short time. Because 38% of the patient population (50/132) was excluded before the start of our first midterm follow-up study for reasons other than failed nonoperative treatment, we are not able to draw a valuable conclusion regarding the overall failure rate of nonoperative treatment for osteochondral talar lesions. However, given a median VAS score of 0 points at the final follow-up, it is reasonable to advise patients that they will have low-level symptoms in the long term if they initially reached satisfactory pain reduction within a 6-month period of nonoperative treatment.
Conclusion
Osteochondral lesions of the talus that successfully underwent an initial nonoperative treatment period were associated with minimal symptoms in the long term, a low failure rate, and no relevant ankle osteoarthritis progression. However, a decrease in sports activity due to sports-related ankle pain was observed in more than a third of the patients.
Acknowledgment
The authors acknowledge Nathalie Kühne for her assistance with this research project.
Footnotes
Final revision submitted January 28, 2020; accepted February 14, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the Research Ethics Committee of Zürich (BASEC No. 2017-01786).
References
- 1. Bauer M, Jonsson K, Lindén B. Osteochondritis dissecans of the ankle: a 20-year follow-up study. J Bone Joint Surg Br. 1987;69(1):93–96. [DOI] [PubMed] [Google Scholar]
- 2. Berndt A, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am. 1959;41:988–1020. [PubMed] [Google Scholar]
- 3. Blom JM, Strijk SP. Lesions of the trochlea tali: osteochondral fractures and osteochondritis dissecans of the trochlea tali. Radiol Clin. 1975;44(5):387–396. [PubMed] [Google Scholar]
- 4. Canale ST, Belding RH. Osteochondral lesions of the talus. J Bone Joint Surg Am. 1980;62(1):97–102. [PubMed] [Google Scholar]
- 5. Chhabra A, Soldatos T, Chalian M, Carrino JA, Schon L. Current concepts review: 3T magnetic resonance imaging of the ankle and foot. Foot Ankle Int. 2012;33(2):164–171. [DOI] [PubMed] [Google Scholar]
- 6. Choi WJ, Park KK, Kim BS, Lee JW. Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 2009;37(10):1974–1980. [DOI] [PubMed] [Google Scholar]
- 7. Dahmen J, Lambers KTA, Reilingh ML, van Bergen CJA, Stufkens SAS, Kerkhoffs GMMJ. No superior treatment for primary osteochondral defects of the talus. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):2142–2157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dekker TJ, Dekker PK, Tainter DM, Easley ME, Adams SB. Treatment of osteochondral lesions of the talus: a critical analysis review. JBJS Rev. 2017;5(3):104–110. [DOI] [PubMed] [Google Scholar]
- 9. Flick AB, Gould N. Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new surgical approach for medial dome lesions. Foot Ankle. 1985;5(4):165–185. [DOI] [PubMed] [Google Scholar]
- 10. Hintermann B, Boss A, Schäfer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30(3):402–409. [DOI] [PubMed] [Google Scholar]
- 11. Klammer G, Maquieira GJ, Spahn S, Vigfusson V, Zanetti M, Espinosa N. Natural history of nonoperatively treated osteochondral lesions of the talus. Foot Ankle Int. 2015;36(1):24–31. [DOI] [PubMed] [Google Scholar]
- 12. Leontaritis N, Hinojosa L, Panchbhavi VK. Arthroscopically detected intra-articular lesions associated with acute ankle fractures. J Bone Joint Surg Am. 2009;91(2):333–339. [DOI] [PubMed] [Google Scholar]
- 13. Loomer R, Fisher C, Lloyd-Smith R, Sisler J, Cooney T. Osteochondral lesions of the talus. Am J Sports Med. 1993;21(1):13–19. [DOI] [PubMed] [Google Scholar]
- 14. McCullough CJ, Venugopal V. Osteochondritis dissecans of the talus: the natural history. Clin Orthop Relat Res. 1979;144:264–268. [PubMed] [Google Scholar]
- 15. O’Loughlin PF, Heyworth BE, Kennedy JG. Current concepts in the diagnosis and treatment of osteochondral lesions of the ankle. Am J Sports Med. 2010;38(2):392–404. [DOI] [PubMed] [Google Scholar]
- 16. Pettine KA, Morrey BF. Osteochondral fractures of the talus: a long-term follow-up. J Bone Joint Surg Br. 1987;69(1):89–92. [DOI] [PubMed] [Google Scholar]
- 17. Rödén S, Tillegård P, Unander-Scharin L. Osteochondritis dissecans and similar lesions of the talus: report of fifty-five cases with special reference to etiology and treatment. Acta Orthop. 1953;23(1):51–66. [DOI] [PubMed] [Google Scholar]
- 18. Seo SG, Kim JS, Seo DK, Kim YK, Lee SH, Lee HS. Osteochondral lesions of the talus: few patients require surgery. Acta Orthop. 2018;89(4):462–467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Shearer C, Loomer R, Clement D. Nonoperatively managed stage 5 osteochondral talar lesions. Foot Ankle Int. 2002;23(7):651–654. [DOI] [PubMed] [Google Scholar]
- 20. Tol JL, Struijs PA, Bossuyt PM, Verhagen RA, van Dijk CN. Treatment strategies in osteochondral defects of the talar dome: a systematic review. Foot Ankle Int. 2000;21(2):119–126. [DOI] [PubMed] [Google Scholar]
- 21. van Dijk C, Verhagen R, Tol J. Arthroscopy for problems after ankle fracture. J Bone Joint Surg Br. 1997;79(2):280–284. [DOI] [PubMed] [Google Scholar]
- 22. Verhagen RAW, Struijs PAA, Bossuyt PMM, Van Dijk CN. Systematic review of treatment strategies for osteochondral defects of the talar dome. Foot Ankle Clin. 2003;8(2):233–242. [DOI] [PubMed] [Google Scholar]
- 23. Zengerink M, Szerb I, Hangody L, Dopirak RM, Ferkel RD, van Dijk CN. Current concepts: treatment of osteochondral ankle defects. Foot Ankle Clin. 2006;11(2):331–359. [DOI] [PubMed] [Google Scholar]