Abstract
Background
Circulating tumor cells (CTCs) are an established prognostic marker in castration-resistant prostate cancer but have received little attention in localized high-risk disease. We studied the detection rate of CTCs in patients with high-risk prostate cancer before and after androgen deprivation therapy and radiotherapy to assess its value as a prognostic and monitoring marker.
Patients and methods
We performed a prospective analysis of CTCs in the peripheral blood of 65 treatment-naïve patients with high-risk prostate cancer. EpCAM-positive CTCs were enumerated using the CELLSEARCH system at 4 timepoints. A cut off of 0 vs ≥ 1 CTC/7.5 ml blood was defined as a threshold for negative versus positive CTCs status.
Results
CTCs were detected in 5/65 patients (7.5%) at diagnosis, 8/62 (12.9%) following neoadjuvant androgen deprivation and 11/59 (18.6%) at the end of radiotherapy, with a median CTC count/7.5 ml of 1 (range, 1–136). Only 1 patient presented a positive CTC result 9 months after radiotherapy. Positive CTC status (at any timepoint) was not significantly associated with any clinical or pathologic factors. However, when we analyzed variations in CTC patterns following treatment, we observed a significant association between conversion of CTCs and stages T3 (P = 0.044) and N1 (P = 0.002). Detection of CTCs was not significantly associated with overall survival (P > 0.40).
Conclusions
Our study showed a low detection rate for CTCs in patients with locally advanced high-risk prostate cancer. The finding of a de novo positive CTC count after androgen deprivation therapy is probably due to a passive mechanism associated with the destruction of the tumor. Further studies with larger samples and based on more accurate detection of CTCs are needed to determine the potential prognostic and therapeutic value of this approach in non-metastatic prostate cancer.
Trial registration
ClinicalTrials.gov ID: NCT01800058.
Keywords: Prostate cancer; Circulating tumor cells (CTCs); Radiotherapy; Androgen suppression; Treatment outcome; Prognostic factor, detection
Background
High-risk prostate cancer is a challenging disease. The combination of high-dose radiotherapy and androgen deprivation represents the standard of care and has yielded encouraging results [1]. More recently, preliminary results with the addition of abiraterone acetate or docetaxel [2, 3] to luteinizing hormone–releasing hormone agonists point to an improved outcome in selected patients. However, given that some subgroups of patients with unfavorable prognostic factors do not respond as well to these treatments, it is necessary to identify improved biomarkers in order to identify patients who require a more aggressive approach. Growing evidence of the clinical importance of detecting circulating tumor cells (CTCs) in the peripheral blood of cancer patients indicates that this is a relevant prognostic and predictive biomarker after care [4, 5].
Counting CTCs using the CELLSEARCH assay (Menarini, Silicon Biosystems Inc., Bologna, Italy) was recently proven to be a reliable prognostic biomarker in metastatic castration-resistant prostate cancer [6–9]. Even more recently, the results of 2 prospective trials with abiraterone and chemotherapy [10] showed that changes in CTCs as early as 4 weeks after treatment identified patients who were not benefiting from treatment, thus suggesting that the CTC count could be an intermediate biomarker for overall survival in advanced metastatic prostate cancer.
These data contradict the limited available information in non-metastatic prostate cancer. The few studies that have examined the response of CTCs to radiotherapy or radical prostatectomy in patients with localized prostate cancer have reported conflicting results [11, 12]. Consequently, we conducted a prospective multicenter phase II study to determine the proportion of patients with high-risk or locally advanced prostate cancer who presented CTCs in peripheral blood at diagnosis and to assess the association between this finding and clinically recognized prognostic factors. We also analyzed the patterns of change in CTCs following androgen deprivation and radiotherapy in order to assess their potential impact on clinical outcome. We hypothesized that the CTC count could not only identify patients with a poorer prognosis, but also determine the degree of response to treatment (sensitivity to radiotherapy and hormone therapy) in patients with high-risk prostate cancer.
Material and methods
Patients and treatment
The study population comprised 66 treatment-naïve patients with non-metastatic prostate cancer recruited from 3 Spanish teaching hospitals between 2014 and 2016. Of these, 65 were eligible for the CTC analysis. Patients aged 18 years or older with histologically confirmed adenocarcinoma of the prostate and ≥ 1 high-risk factors (prostate-specific antigen [PSA] > 20 ng/ml, Gleason 8–10, stage T3–4), N0 or N1, a Karnofsky performance score of ≥70, and a life expectancy of more than 5 years were eligible for inclusion. The study was approved by the independent review board at each participating center and conducted according to the provisions of the Declaration of Helsinki and the Good Clinical Practice Guidelines of the International Conference on Harmonization. Patients provided their written informed consent before participating in the study.
Patients received combined modality therapy comprising high-dose radiotherapy and hormone therapy. Radiotherapy was administered using 3-dimensional conformational radiation therapy (45 patients) or intensity-modulated radiation therapy (20 patients) at a median dose of 76.3 Gy (range, 74.8–79.2) and 81.7 Gy (range, 70.6–82-8), respectively. Hormone therapy consisted of 4 months of neoadjuvant and concomitant androgen deprivation followed by adjuvant androgen deprivation for a median of 26 (17–36) months.
Procedures
Peripheral blood samples were collected prospectively and analyzed to detect CTCs at 4 timepoints: 1) baseline or before starting treatment (visit 1); 2) after neoadjuvant androgen deprivation and before radiotherapy (visit 2); 3) at the end of radiotherapy (visit 3); and 4) 6–12 months after the end of radiotherapy in those patients with 0 CTCs in the first determination and conversion to positive CTCs in the following determinations (visit 4). One tube (7.5 mL) of peripheral blood was obtained from each patient at each sampling point. We used the CELLSEARCH assay (Menarini, Silicon Biosystems Inc., Bologna, Italy), which is the only CTC detection method approved by the United States Food and Drug Administration. Therefore, peripheral blood was analyzed using the CELLSEARCH Circulating Tumor Cell kit at the Liquid Biopsy Analysis Unit of the Health Research Institute of Santiago de Compostela. The system immunoisolated cells that were positive for epithelial cell adhesion molecule (EpCAM). Enriched cells were then labelled with phycoerythrin-conjugated anti-cytokeratins antibodies, allophycocyanin-conjugated anti-CD45 antibodies, and 4,6-diamino-2-phenylindole to identify the nucleus. Digital images of the 3 different fluorescent dyes were acquired using the CELLTRACKS Analyzer and a 12-bit camera. The images were reviewed by trained operators in order to determine the CTC count (Fig. 1). Round-oval, DAPI+, CD45−, and CK+ cells were considered CTCs.
Fig. 1.
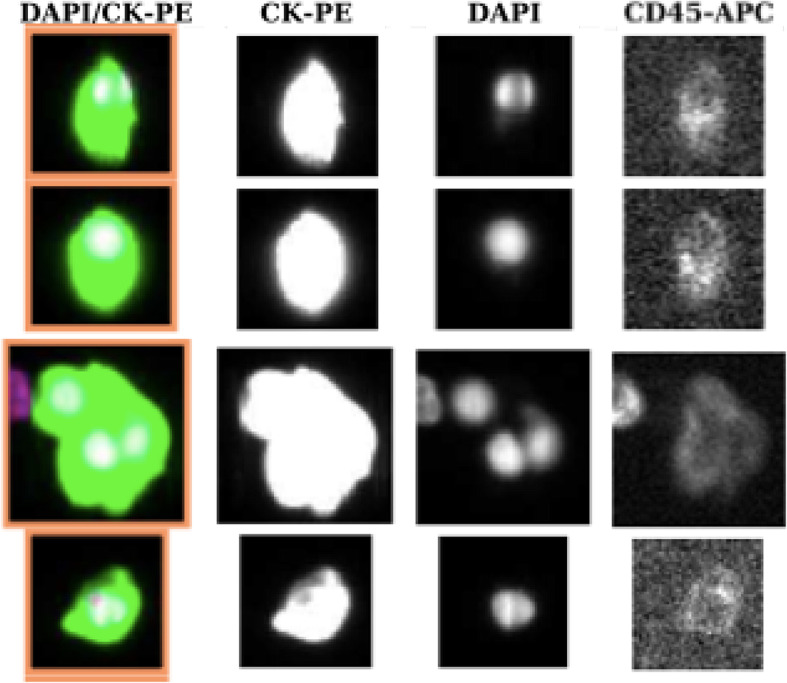
Images of CTCs obtained from a patient with prostate cancer using the CELLSEARCH system. Only round-oval, DAPI+, CD45−, and CK+ cells were considered CTCs
Statistical methods
The frequency of expression of CTCs was estimated with its 95% confidence interval (CI). Initially a cutoff point of ≥3 CTCs/7.5 mL of blood was taken as the reference baseline. Because of the low CTC counts observed and for statistical purposes, we empirically established a cut-off of 0 vs ≥1 CTCs/7.5 mL blood as the thresholds between negative and positive CTC status. The association between the presence and development of CTCs over time and well-known clinicopathological features was assessed using the χ2 test or Fisher exact test. Overall survival, metastasis-free survival, and biochemical failure–free survival were estimated using the Kaplan-Meier method. The curves were compared using the log-rank test. All events were defined as time until death from any cause (OS), distant metastasis (MFS), biochemical failure (bFS), or date of last follow-up visit. Cox regression models were constructed to estimate the hazard ratio and 95% CI as a measure of the effect and were adjusted for potential confounding variables (P ≤ 0.20)..All hypothesis tests were performed using 2-tailed alternatives. Statistical significance was set at P < 0.05.
Results
The initial study sample comprised 66 high-risk patients, of whom 65 were evaluable for the analysis (1 patient was lost to follow-up before completing the CTC study). The median age was 71 years (range, 53–79), and the median pretreatment PSA value was 12.6 ng/mL (range, 3.2–68.7). The Gleason score was ≥8 in 28 patients, and 48 patients were in clinical stage T3. The median interquartile range (IQR) follow-up was 55 (23–64) months. Patient and treatment characteristics are summarized in Table 1.
Table 1.
Summary of patient and treatment characteristics
| N = 65 | |
|---|---|
| Median (range) age, years | 71 (53–79) |
| > 65 | 16 (25%) |
| ≤ 65 | 49 (75%) |
| Median follow-up, months (range) | 55 (10–40) |
| Median PSA, ng/mL (range) | 12.6 (3.2–68.7) |
| < 10 | 22 (34%) |
| 10–20 | 20 (31%) |
| > 20 | 23 (35%) |
| Gleason Group 1 | 5 (8%) |
| Group 2 | 13 (20%) |
| Group 3 | 19 (29%) |
| Group 4 | 20 (31%) |
| Group 5 | 8 (12%) |
| T stage T1 | 1 (2%) |
| T2 | 17 (26%) |
| T3 | 47 (72%) |
| Number of high-risk factors 1 | 35 (54%) |
| 2 | 28 (43%) |
| 3 | 2 (3%) |
| N stage N0 | 52 (80%) |
| N1 | 13 (20%) |
| Technique 3DCRT | 44 (68%) |
| Technique IMRT | 21 (32%) |
| Median dose 3DCRT, Gy (range) | 76.3 (74.78–79.16) |
| Median dose IMRT Gy (range) | 81.7 (70.6–82-8) |
PSA prostate-specific antigen, 3DCRT 3-dimensional conformal radiation therapy, IMRT intensity-modulated radiation therapy
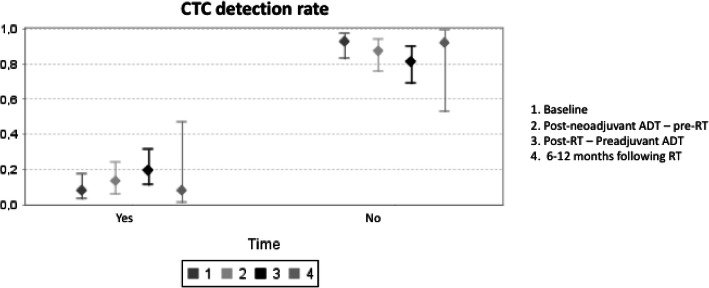
The median CTC count/7.5 mL at all of the timepoints was 1 (1–136). The changing pattern of detection over time is summarized in Table 2 and Fig. 2. At diagnosis (visit 1), CTCs were detected in only 5/65 patients (7.5%). Of these, 3 became negative at visit 2 (following neoadjuvant androgen deprivation), and the remaining 2 patients became negative following radiotherapy (visit 3). At visit 2, CTCs were analyzed in 62 patients (3 patients did not complete the analysis), and de novo CTC positivity was detected in 6 patients whose values became negative at visits 3 and 4. We also observed de novo CTC positivity at visit 3 (end of radiotherapy) in 8 patients. Only 1 patient presented positive CTC results 9 months after radiotherapy.
Table 2.
CTC counts before and after treatment
| CTC Timing | CTC Positivity/Determinations |
|---|---|
| CTC1 | |
| ≥1 cells/7.5 ml (%) (range) | 5/65 (7.5%) (1-6) |
| 0 cells /7.5 ml | 60 |
| CTC2 | |
| ≥1 cells/7.5 ml (range) |
8/62(12.9%) (1-1) New presentation in 6 |
| 0 cells /7.5 ml | 54 |
| Not performed | 3 |
| CTC3 | |
| ≥1 cells/7.5 ml (range) |
11/59 (18.6%) (1-136) New presentation in 10 |
| 0 cells /7.5 ml | 48 |
| Not performed | 6 |
| CTC4 | |
| ≥1 cells/7.5 ml (range) | 1/13 (7.6%) (1) |
| 0 cells /7.5 ml | No new: persistence from CTC3 12 |
CTC 1: Baseline; CTC 2: After neoadjuvant androgen deprivation therapy and before radiotherapy; CTC 3: After radiotherapy; CTC 4: 6-12 months after radiotherapy in patients with new positivity at CTC 2 or CTC 3
Fig. 2.
CTCs detection rate at 4 timepoints: 1) baseline; 2) after neoadjuvant androgen deprivation therapy; 3) at the end of radiotherapy; and 4) 6–12 months after the end of radiotherapy in those patients with 0 CTCs in the first determination and a change to positive CTCs in the following determinations. CTC, circulating tumor cell; ADT, androgen deprivation therapy
Positive CTC status (at any timepoint) was not significantly associated with clinical and pathologic factors (patient age, pre-treatment PSA, T stage, N stage, Gleason score, and number of positive cores). Similarly, we did not find an association between positive CTC status and the presence of secondary tumors (Table 3). However, when we analyzed the variation pattern of positive CTC results following treatment, we observed a significant association between CTC conversion and stages T3 (P = 0.044) and N1 (P = 0.002).
Table 3.
CTC positivity and association with prognostic factors
| CTC1+ | CTC2+ | CTC3+ | CTC4+ | |
|---|---|---|---|---|
| Age, y ≤65 | 1 | 2 | 2 | 0 |
| >65 | 4 | 6 | 9 | 1 |
| p value | 1.000 | 1.000 | 0.712 | 1.000 |
| PSA <10 ng/mL | 2 | 1 | 4 | 1 |
| 10-20 ng/mL | 2 | 5 | 4 | 0 |
| >20 ng/mL | 1 | 2 | 2 | 0 |
| p value | 0.852 | 0.128 | 0.711 | 1.000 |
| Gleason <8 | 3 | 7 | 5 | 1 |
| sum ≥ 8 | 2 | 1 | 6 | 0 |
| p value | 1.000 | 0.128 | 0.502 | 1.000 |
| T Stage | ||||
| <T3 | 0 | 1 | 6 | 0 |
| ≥T3 | 5 | 7 | 5 | 1 |
| p value | 0.312 | 0.668 | 0.062 | 1.000 |
| N Stage | ||||
| 0 | 5 | 7 | 7 | 1 |
| 1 | 0 | 1 | 4 | - |
| p value | 0.574 | 1.000 | 0.053 | |
| Secondary tumors | ||||
| Yes | 3 | 6 | 9 | 0 |
| No | 2 | 2 | 2 | 1 |
| p value | 0.621 | 1.000 | 0.484 | 0.231 |
PSA prostate-specific antigen
Only 1 patient experienced biochemical relapse and metastatic disease (at 31 months) and is currently alive (no positive CTCs at any timepoint). Six patients died, none of them from prostate cancer. Detection of CTCs at diagnosis and following treatment was not significantly associated with overall survival (P = 0.40).
Discussion
The main objective of the present study was to assess the viability of detecting CTCs in non-metastatic high-risk prostate cancer patients. Our findings revealed a low count and incidence of CTCs. Only 5 out of 65 patients (7.5%) harbored CTCs at diagnosis, that is, at the bottom range of the detection rates of other studies. The few published reports using the CELLSEARCH system in patients with localized prostate cancer showed positivity rates of 5–27% [13–15]. These studies were carried out in patients treated predominantly with radical prostatectomy or brachytherapy and included early stages of prostate cancer. In an attempt to improve the CTC detection rate, we focused the design of the study on including only patients with locally advanced, high-risk disease (13 patients had N1 disease and 30 patients had 2 or more risk factors). To our knowledge, this is the first prospective study performed in this subgroup of patients treated homogeneously with high-dose radiotherapy plus androgen deprivation and with repeated CTC determinations at predetermined intervals to monitor treatment response.
The many methods used to detect CTCs range from real-time polymerase chain reaction to cell size–based separation or immunomagnetic beads conjugated with anti-EpCAM antibodies [16–19], each of which is subject to intrinsic limitations, including reproducibility. For metastatic prostate cancer, the CELLSEARCH system was shown to provide prognostic information in several large clinical trials [7, 8, 20, 21]. Nevertheless, in localized prostate cancer, the CELLSEARCH methodology is now believed to underestimate the actual number of CTCs, perhaps owing to fragmentation of conventional CTCs and the inability to detect the less epithelial CTCs [13]. Data from recent studies have shown that EpCAM-based enrichment alone could not detect all CTC subpopulations [22].
Several attempts have been made to overcome this limitation. Theil et al. [23] used a new system, CellCollector to isolate in vivo CTCs from patients with different stages of prostate cancer and found more frequent detection of CTCs than with the CELLSEARCH system. Kuske et al. [24] also reported improved detection of CTCs in nonmetastatic prostate cancer patients by combining 3 independent CTC assays: the CELLSEARCH system, CellCollector, and EPISPOT (an EpCAM-independent enrichment method). Peripheral blood samples were screened for CTCs before radical prostatectomy in 86 high-risk prostate cancer patients and 3 months after radical prostatectomy in 52 patients. The cumulative positivity rate of all 3 CTC assays was 81.3% (87/107), with 21.5 (23/107) of patients harboring ≥5 CTCs per blood sample. The authors hypothesize that the correlation observed with established risk factors and the persistence of CTCs 3 months after surgery could suggest the potential clinical relevance of CTCs as markers of minimal residual disease in prostate cancer.
The second objective of the present study was to analyse whether the variation in the CTC count at predetermined intervals during the treatment regimen would predict outcome and enable a real-time response. We expected a decline in the numbers of CTCs following treatment. Unpredictably, an increasing and transient CTC count was detected de novo after androgen deprivation and radiotherapy. The CTC detection rate was 7.5% at diagnosis, which increased to 12.9% following neoadjuvant androgen deprivation and 18.6% at the end of radiotherapy before decreasing again to 7.5% at 9 months after the end of radiotherapy. When we investigated this changing pattern of CTC positivation more specifically, we observed a significant association with locally advanced disease (T3–4 stage, p = 0.044; and N1 stage, p = 0.002). Although we do not have a clear explanation for this finding, we believe that it could be due to a passive mechanism associated with the destruction of the tumor. A further analysis with longer follow-up is required to clearly determine the relevance of CTC positivation during the treatment.
Importantly, other authors have reported similar findings. Stott et al. [25] observed that of 11 patients with preoperative CTCs counts below the cutoff, 4 had transient elevations in CTCs during the follow-up period. Tsumura et al. [12] evaluated whether prostate brachytherapy procedures had a potential risk for hematogenous spillage of prostate cancer cells in 59 patients using the CELLSEARCH system. The authors detected CTCs from samples immediately after the brachytherapy procedure in 7 patients (intraoperative CTC detection rates were significantly higher than preoperative ones), although they did not repeat the CTC analysis during follow-up to evaluate whether those CTCs could actually survive and proliferate at distant sites.
We were unable to show a significant association between positive CTC status at diagnosis and known clinical and histologic prognostic factors. This lack of correlation has been extensively observed in studies carried out in localized prostate cancer [11, 16, 25]. The small sample size and the low CTC detection rate might limit the relevance of these results.
In one of the longest prospective series (152 patients analysed using the CELLSEARCH platform), Meyer et al. [26] did not observe a significant relationship with PSA, Gleason score, or pT stage. The CTC detection rate in their series was only 11%. Pal et al. [27] used a modified isolation procedure on the CELLSEARCH platform in 35 patients with high-risk, localized prostate cancer. With a CTC detection rate of 49% prior to surgery, they did not observe any correlation between the presence of CTCs and clinicopathological prognostic features. In contrast, Kuske et al. [24] used the EPISPOT method before radical prostatectomy and found a significant association between CTCs and PSA and clinical T stage. The detection rate with EPISPOT was 58.7%. However, they failed to show any clinical correlation with the other assays (the CELLSEARCH system and the in vivo CellCollector).
Only 1 patient in our series experienced biochemical and distant failure, and 6 patients have since died, none of them from prostate cancer. Again, we did not observe any association between CTC count and overall survival. Although some authors report a trend towards shorter recurrence times [28], no studies to date have proved the predictive value of CTCs in disease-free or overall survival.
Our study is subject to the limitations inherent to an observational feasibility study, namely, the small sample size and short follow-up. The main strengths are its prospective design with pre-established CTC determinations at predetermined intervals to monitor treatment response.
In conclusion, the data obtained from this study showed a low detection rate for CTCs in patients with high-risk prostate cancer. The finding of de novo positive CTC counts after androgen deprivation and radiotherapy (mostly with very low levels and not maintained over time) may be due to a passive mechanism associated with destruction of the tumor. Further studies with a longer follow-up period, larger samples with more events and a more acute assessment method are needed to determine the potential prognostic and therapeutic value of detection of CTCs in nonmetastatic prostate cancer.
Acknowledgements
We thank Thomas O’Boyle for his editorial assistance.
Abbreviations
- CTCs
Circulating tumor cells
- CI
Confidence interval
- Gy
Gray
- IMRT
Intensity-modulated radiation therapy
- IQR
Interquartile range
- PSA
Prostatic specific antigen
- 3DCRT
3-dimensional conformal radiation therapy
Authors’ contributions
A.Z., A.G.C, M.A.C, CO and L.M.R. were responsible for the concept and design of the protocol trial and the interpretation of the results. L.M.R and A.A. were responsible for liquid biopsy analysis and biological interpretation of data. A.Z., A.G.C, M.A.C, C.M.V., L.L.M and P. C participated in the enrollment and, treatment of patients. L.V.P. was the responsible person for the statistical analysis. A.Z. wrote the manuscript and all authors read and approved the final manuscript.
Authors’ information
A.Z is Senior Consultant of the Department of Radiation Oncology and Head of Laboratory of Health Research Institute of IIS-IP at Hospital Universitario de la Princesa, Madrid, Spain.
A.G.C is Head of the Department of Radiation Oncology at Hospital Universitario de Santiago de Compostela, Spain, and President of SEOR (Spanish Society of Radiation Oncology).
L.M.R is the person in charge for the Liquid Biopsy Analysis Unit, Health Research Institute of Santiago (IDIS), CIBERONC, Santiago de Compostela, Spain.
L.V.P is the responsible person of the Methodology Unit, Health Research Institute of Hospital Universitario de La Princesa, Madrid, Spain.
Funding
Funded by a grant from Janssen- Pharmaceuticals, number: 212082PCR4005.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study has been approved by the Ethics Committee in Clinical Research of Hospital Universitario de La Princesa, reference number 2045.
Consent for publication
Not applicable.
Competing interests
Other than the grant from Janssen-Cilag, the authors declare no potential conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bolla M, Maingon P, Carrie C, Villa S, Kitsios P, Poortmans P, et al. Short androgen suppression and radiation dose escalation for intermediate- and high-risk localized prostate Cancer: results of EORTC trial 22991. J Clin Oncol. 2016;34(15):1748–1756. doi: 10.1200/JCO.2015.64.8055. [DOI] [PubMed] [Google Scholar]
- 2.James ND, de Bono JS, Spears MR, Clarke NW, Mason MD, Dearnaley DP, et al. Abiraterone for prostate Cancer not previously treated with hormone therapy. N Engl J Med. 2017;337(4):338–351. doi: 10.1056/NEJMoa1702900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.James ND, Sydes MR, Clarke NW, Mason MD, Dearnaley DP, Spears MR, et al. Addition of docetaxel, zoledronic acid, or both to first-line long-term hormone therapy in prostate cancer (STAMPEDE): survival results from an adaptive, multiarm, multistage, platform randomised controlled trial. Lancet. 2016;387:1163–1177. doi: 10.1016/S0140-6736(15)01037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fehm T, Sagalowsky A, Clifford E, Beitsch P, Saboorian H, Euhus D, et al. Cytogenetic evidence that circulating epithelial cells in patients with carcinoma are malignant. Clin Cancer Res. 2002;8(7):2073–2084. [PubMed] [Google Scholar]
- 5.Danila DC, Heller G, Gignac GA, Gonzalez-Espinoza R, Anand A, Tanaka E, et al. Circulating tumor cell number and prognosis in progressive castration-resistant prostate cancer. Clin Cancer Res. 2007;13(23):7053–7057. doi: 10.1158/1078-0432.CCR-07-1506. [DOI] [PubMed] [Google Scholar]
- 6.de Bono JS, Scher HI, Montgomery RB, Parker C, Miller MC, Tissing H, et al. Circulating tumor cells predict survival benefit from treatment in metastatic castration-resistant prostate cancer. Clin Cancer Res. 2008;14(19):6302–6309. doi: 10.1158/1078-0432.CCR-08-0872. [DOI] [PubMed] [Google Scholar]
- 7.Olmos D, Arkenau H, Ang JE, Ledaki I, Attard G, Carden CP, et al. Circulating tumour cell (CTC) counts as intermediate end points in castration-resistant prostate cancer (CRPC): a single-Centre experience. Ann Oncol. 2009;20(1):27–33. doi: 10.1093/annonc/mdn544. [DOI] [PubMed] [Google Scholar]
- 8.Scher HI, Jia X, de Bono JS, Fleisher M, Pienta KJ, Raghavan D, et al. Circulating tumour cells as prognostic markers in progressive, castration-resistant prostate cancer: a reanalysis of IMMC38 trial data. Lancet Oncol. 2009;10(3):233–239. doi: 10.1016/S1470-2045(08)70340-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heller G, McCormack R, Kheoh T, Molina A, Smith MR, Dreicer R, et al. Circulating tumor cell number as a response measure of prolonged survival for metastatic castration-resistant prostate Cancer: a comparison with prostate-specific antigen across five randomized phase III clinical trials. J Clin Oncol. 2018;36(6):572–580. doi: 10.1200/JCO.2017.75.2998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorente D, Olmos D, Mateo J, Bianchini D, Seed G, Fleisher M, et al. Decline in circulating tumor cell count and treatment outcome in advanced prostate Cancer. Eur Urol. 2016;70(6):985–992. doi: 10.1016/j.eururo.2016.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chalfin HJ, Glavaris SA, Malihi PD, Sperger JM, Gorin MA, Lu C, et al. Prostate Cancer disseminated tumor cells are rarely detected in the bone marrow of patients with localized disease undergoing radical prostatectomy across multiple rare cell detection platforms. J Urol. 2018;199(6):1494–1501. doi: 10.1016/j.juro.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tsumura H, Satoh T, Ishiyama H, Tabata K, Takenaka K, Sekiguchi A, et al. Perioperative Search for Circulating Tumor Cells in Patients Undergoing Prostate Brachytherapy for Clinically Nonmetastatic Prostate Cancer. Int J Mol Sci. 2017;18(1). [DOI] [PMC free article] [PubMed]
- 13.Davis JW, Nakanishi H, Kumar VS, Bhadkamkar VA, McCormack R, Fritsche HA, et al. Circulating tumor cells in peripheral blood samples from patients with increased serum prostate specific antigen: initial results in early prostate cancer. J Urol. 2008;179:2187–2191. doi: 10.1016/j.juro.2008.01.102. [DOI] [PubMed] [Google Scholar]
- 14.Thalgott M, Rack B, Horn T, Heck MM, Eiber M, Kübler H, et al. Detection of circulating tumor cells in locally advanced high-risk prostate Cancer during Neoadjuvant chemotherapy and radical prostatectomy. Anticancer Res. 2015;35(10):5679–5685. [PubMed] [Google Scholar]
- 15.Loh J, Jovanovic L, Lehman M, Capp A, Pryor D, Harris M, et al. Circulating tumor cell detection in high-risk non-metastatic prostate cancer. J Cancer Res Clin Oncol. 2014;140(12):2157–2162. doi: 10.1007/s00432-014-1775-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gewanter RM, Katz AE, Olsson CA, Benson MC, Singh A, Schiff PB, et al. RT-PCR for PSA as a prognostic factor for patients with clinically localized prostate cancer treated with radiotherapy. Urology. 2003;61(5):967–971. doi: 10.1016/S0090-4295(02)02581-5. [DOI] [PubMed] [Google Scholar]
- 17.Panteleakou Z, Lembessis P, Sourla A, Pissimissis N, Polyzos A, Deliveliotis C, et al. Detection of circulating tumor cells in prostate cancer patients: methodological pitfalls and clinical relevance. Mol Med. 2009;15(3–4):101–114. doi: 10.2119/molmed.2008.00116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miyamoto DT, Lee RJ. Cell-free and circulating tumor cell-based biomarkers in men with metastatic prostate cancer: tools for real-time precision medicine? Urol Oncol. 2016;34(11):490–501. doi: 10.1016/j.urolonc.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 19.Gorin MA, Verdone JE, Van der Toom E, Bivalacqua TJ, Allaf ME, Pienta KJ. Circulating tumour cells as biomarkers of prostate, bladder, and kidney cancer. Nat Rev Urol. 2017;14(2):90–97. doi: 10.1038/nrurol.2016.224. [DOI] [PubMed] [Google Scholar]
- 20.Goldkorn A, Ely B, Quinn DI, Tangen CM, Fink LM, Xu T, et al. Circulating tumor cell counts are prognostic of overall survival in SWOG S0421: a phase III trial of docetaxel with or without atrasentan for metastatic castration-resistant prostate cancer. J Clin Oncol. 2014;32(11):1136–1142. doi: 10.1200/JCO.2013.51.7417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zheng Y, Zhang C, Wu J, Cheng G, Yang H, Hua L, et al. Prognostic value of circulating tumor cells in castration resistant prostate Cancer: a meta-analysis. Urol J. 2016;13(6):2881–2888. [PubMed] [Google Scholar]
- 22.Schneck H, Gierke B, Uppenkamp F, Behrens B, Niederacher D, Stoecklein NH, et al. EpCAM-independent enrichment of circulating tumor cells in metastatic breast Cancer. PLoS One. 2015;10(12):e0144535. doi: 10.1371/journal.pone.0144535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Theil G, Fischer K, Weber E, Medek R, Hoda R, Lücke K, et al. The Use of a New CellCollector to Isolate Circulating Tumor Cells from the Blood of Patients with Different Stages of Prostate Cancer and Clinical Outcomes - A Proof-of-Concept Study. PLoS One. 2016;11(8):e0158354. doi: 10.1371/journal.pone.0158354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuske A, Gorges TM, Tennstedt P, Tiebel AK, Pompe R, Preißer F, et al. Improved detection of circulating tumor cells in non-metastatic high-risk prostate cancer patients. Sci Rep. 2016;6:39736. doi: 10.1038/srep39736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stott SL, Lee RJ, Nagrath S, Yu M, Miyamoto DT, Ulkus L, et al. Isolation and characterization of circulating tumor cells from patients with localized and metastatic prostate cancer. Sci Transl Med. 2010;2(25):25ra23. doi: 10.1126/scitranslmed.3000403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meyer CP, Pantel K, Tennstedt P, Stroelin P, Schlomm T, Heinzer H, et al. Limited prognostic value of preoperative circulating tumor cells for early biochemical recurrence in patients with localized prostate cancer. Urol Oncol. 2016;34(5):235. doi: 10.1016/j.urolonc.2015.12.003. [DOI] [PubMed] [Google Scholar]
- 27.Pal SK, He M, Wilson T, Liu X, Zhang K, Carmichael C, et al. Detection and phenotyping of circulating tumor cells in high-risk localized prostate cancer. Clin Genitourin Cancer. 2015;13(2):130–136. doi: 10.1016/j.clgc.2014.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Friedlander TW, Welty C, Anantharaman A, Schonhoft JD, Jendrisak A, Lee J, et al. Identification and characterization of circulating tumor cells in men who have undergone prostatectomy for clinically localized, high risk prostate Cancer. J Urol. 2019;202:732–741. doi: 10.1097/JU.0000000000000393. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.