Abstract
Sleep health is a multidimensional construct that includes adequate duration, quality, and appropriately timed sleep that may be influenced by environmental factors. In this review, we focus on how an individual’s living and sleeping environment, both the surrounding neighborhood physical and social features and the atmosphere around them, may impact their sleep health. We explore the associations of the physical environment (urban density, recreational facilities, green space, mixed land use, and healthy food stores), neighborhood deprivation (disadvantage and disorder), and the social environment (social cohesion, safety, and stigma) with sleep in both adult and pediatric populations. We investigate how physical and social environmental features may lead to alterations in the timing, duration, and quality of sleep and contribute to the most prevalent sleep disorders: insomnia, sleep apnea, and circadian rhythm disorders. We also review how ambient factors such as artificial light, environmental noise, and air pollution may contribute to sleep pathology. We have included key studies and recent emerging data regarding how the differential distribution of environmental factors that may affect sleep health may contribute to sleep health disparities.
Key Words: built environment, sleep apnea, sleep health, social environment
Abbreviations: AHI, apnea hypopnea index; GIS, geographic information system; SES, socioeconomic status; WASO, wakefulness-after-sleep-onset
Sleep, as integral to health as food and water, is intrinsically sensitive to the external environment—ambient sounds, light, air quality, and the contextual features around the sleeping space. The ability to relax the body and mind to allow sleep may be affected by the sense of comfort and safety of the surrounding environment. Obtaining adequate, restorative, healthy sleep—appropriate in timing, quantity, and quality/satisfaction1—is essential for well-being. Poor sleep health reflects sleep disorders and insufficient, fragmented, nonrestorative, or delayed sleep, which may be out of synch with internal circadian rhythms or social obligations. Vulnerable populations such as racial/ethnic minorities or individuals of lower socioeconomic status (SES) have a higher burden of poor sleep health, largely because of socially patterned disparities.2 This may reflect differences in environmental exposures related to neighborhood segregation.3
In this review, we will detail how detrimental physical and social environmental conditions may worsen sleep health and contribute to sleep pathology including insomnia, circadian rhythm disorders, sleep apnea, and chronic insufficient sleep. We limit the scope of our discussion to the environment surrounding the home—primarily focusing on neighborhood-level features. We will not explore school or work, institutionalization (eg, prison, nursing homes, homeless shelters), or transportation and commute lengths, which all may impact sleep opportunity and timing. We also exclude discussion of the many within-home factors that contribute to sleep health, which are beyond the scope of this focused review.
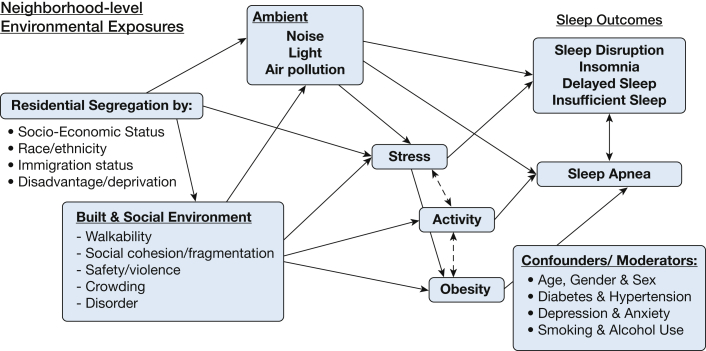
The physical environment includes the built environment, the natural environment, and the ambient environment. The built environment consists of neighborhood features constructed by humans, which encompasses city architecture, urban planning, and design; it influences how people use the neighborhood space surrounding their home, work, or school. Street connectivity, sidewalks, mixed land use (both commercial and residential zoning), healthy food stores, and social engagement destinations (eg, churches, community centers, shops) are all features of the built environment that may impact walkability, physical activity, and social cohesion.4 The ambient environment (sounds, lights, temperature, humidity, and atmosphere) is another aspect of the physical environment that may impact sleep. The social environment encompasses neighborhood social features, such as safety, crime, cohesion, and connectivity. The physical and social environment may contribute to the allostatic load and the physiological manifestation of repeated experiences of psychosocial stress including sympathetic nervous system activation and cortisol release.5 The resulting allostatic load in turn may have deleterious influences on sleep (Fig 1). In this review, we will focus first on adults and separately on the specific associations in children. Finally, we will describe potential interventions that may improve sleep health by altering the environment, through natural experiments, and policy changes.
Figure 1.
Sleep and the environment.
Adult Sleep and the Environment
Physical Environment and Adult Sleep Health
Exposure to a natural physical environment has been associated with better sleep health. Observational studies have shown that adults living in neighborhoods with access to green space or natural water features have a lower likelihood of insufficient sleep.6,7 Green vegetation has been associated with better cardiovascular biomarkers and lower sympathetic activation.8 Tree canopy was associated with longer weekday sleep duration in a survey study in Wisconsin.9 These natural environments features are more common in suburban and rural neighborhoods. Green space may promote walking and other healthy behaviors, lower stress levels, and improve mental health which could facilitate healthy sleep. Other environmental features unique to rural living have not been well studied in relation to sleep.
Built Environment and Adult Sleep Health
Prior epidemiologic research has identified an association of built environment features with obesity10 and cardiovascular and metabolic disease.11 Geographic information system (GIS) data demonstrate that lower mixed land use and higher density of fast food outlets are associated with obesity.12,13 These neighborhood obesogenic features could foster sleep apnea by promoting weight gain and sedentary behaviors. Studies have found that residential features promoting physical activity and healthier diets are associated with a lower risk of incident diabetes14 and weight loss.15 Because obesity is an established strong risk factor for sleep apnea,16 living in neighborhood environments that foster obesity may contribute to the risk of developing sleep apnea.
Features of the built environment, such as street connectivity, parks and recreational facilities, and bike lanes, can promote activity; these same features may also influence sleep-disordered breathing. Walkability is higher in neighborhoods with sidewalks, traffic calming, pleasant aesthetic features, and social and recreational destinations4,17 Neighborhood walking environment, assessed via survey, has been associated with sleep apnea independent of individual sociodemographic characteristics.18 Residing in a neighborhood with a less favorable walking environment (rated in the lowest 25% of neighborhoods) was associated with 2.7 events/h higher apnea hypopnea index (AHI), more substantially in those with obesity. Greater actigraphy-measured activity was associated with a 3.4 events/h lower AHI in men, partially mediated by BMI, independent of age, race/ethnicity, comorbidities, education, and income.18 Exercise has been associated with reduced incidence and lower severity of sleep apnea.19 It is hypothesized that exercise reduces lower extremity fluid accumulation; sedentary behaviors lead to rostral fluid buildup and the subsequent upper airway narrowing once supine and the fluid shifts.20 Therefore, built environmental features that promote physical activity may reduce sleep-disordered breathing severity.
However, these urban environment characteristics favorable for activity have also been associated with less sleep. Using data from the Multi-Ethnic Study of Atherosclerosis (MESA), researchers demonstrated that a higher walk score (a measure of neighborhood walkability), a larger population and intersection density, and more social destinations were associated with a shorter sleep duration after adjustment for individual- and neighborhood-level sociodemographic characteristics and individual health behaviors and depressive symptoms.21 These associations were more pronounced in blacks and were partially explained by self-reported noise.21 Although these urban features may promote physical and mental health by encouraging activity and social interactions, and potentially reduce the risk of sleep apnea, this may be at a cost of sleep duration.
Neighborhood Disadvantage and Adult Sleep Health
Neighborhood disadvantage refers to a summary measure of the socioeconomic features of the neighborhood residents, and is often calculated using census data such as high rates of poverty, female-headed households, unemployment, public assistance, and low home ownership. Neighborhood disadvantage has been associated with increased odds of restless sleep in women,22 and longer wakefulness-after-sleep-onset (WASO) among urban dwelling adults.23 In a twin study, area deprivation, a measure of neighborhood disadvantage, was independently associated with shorter sleep duration.24 However, other studies have shown no association between neighborhood disadvantage and sleep duration, sleep quality, or latency.25, 26, 27 Sleep duration differences were associated with neighborhood social environment rather than SES in models adjusting for individual sociodemographics, comorbidities, and health behaviors in one study including participants from Los Angeles, California, and New York, New York, neighborhoods.25 Inconsistent findings across studies may reflect the correlation of disadvantage with other causative neighborhood social factors contributing to sleep health such as the development of trust, social ties, and collective efficacy.
Neighborhood disorder reflects questionnaire-based assessments of neighborhood aesthetics (eg, broken windows, graffiti, litter) and/or perceived neighborhood quality. Disorder is tightly associated with disadvantage and both may impact sleep outcomes. Greater neighborhood disorder has been associated with more sleep disturbances, poor sleep quality, difficulty falling asleep, longer WASO, and shorter sleep duration,25,28, 29, 30 possibly related to the higher levels of fear and anxiety associated with neighborhood decay.31
Social Environment and Adult Sleep Health
The social environment can foster perceptions of safety and social support and can affect mood, anxiety, and stress, which can contribute to a state of arousal and potentially impact sleep. More specifically, an unfavorable social environment can contribute to sleep deprivation, insomnia symptoms, and circadian disruptions (eg, delayed sleep timing).32 The social environment includes perceived, often questionnaire-based, measurements of social connections/cohesion/fragmentation, stigma, safety, violence, and crime. The social environment can also be objectively assessed using the GIS, census data, and crime records. The social environment is enmeshed within the socioeconomic/racial/ethnic characteristics of the neighborhood and is associated with built environmental features, often with unfavorable features in more than one domain. For example, neighborhoods with a lower perception of safety have greater deprivation and disorder.
Living in communities with greater social cohesion is associated with better sleep health such as higher actigraphy-measured and self-reported sleep duration.26,33 Social cohesion reflects high levels of relationships, trust, and community spirit in a neighborhood. Cohesive neighborhoods have less crime, higher perceived safety, and greater social capital. Conversely, social fragmentation, the underdevelopment of connections between community residents, has been associated with shorter sleep duration, lower sleep quality, and greater sleep difficulties across diverse populations including underrepresented minority groups such as blacks, Hispanic/Latinos, and Native Hawaiian and Pacific Islanders.29,33,34
Other measures of the social environment span domains of neighborhood violence and crime, which influence perceptions of safety. Neighborhood crime reports may foster feelings of susceptibility and have potentially negative effects on sleep. Census tract-derived assessments, field observations, and perceived neighborhood violence are associated with shorter self-reported sleep duration and poorer sleep quality and habits.25,26 Living in unsafe neighborhoods may impair residents’ ability to relax and allow sleep onset. Neighborhood-level crime, defined according to police reports, has been less consistently associated with sleep. One study showed that higher crime was associated with lower actigraphy-measured sleep efficiency and longer WASO, independent of sociodemographics, any children in home, years lived in the neighborhood, psychological distress, and BMI.35 However, others have found no statistical association between neighborhood crime and daytime sleepiness and sleep quality.27,29 The difference in associations across studies is likely because of the different methodologies in measuring the neighborhood environment and sleep. Residing in neighborhoods with lower perceived safety is associated with late midpoint, daytime sleepiness, poor sleep quality, short sleep duration, and more insomnia symptoms.27,35,36 Lower perceived neighborhood safety is associated with lower sleep quality in Mexico, Ghana, South Africa, India, China, and Russia.37 Among low-income housing residents in New York, negative media perceptions of the neighborhood were associated with poor sleep quality and short sleep duration.38 Further research on neighborhood stigma and neighborhood segregation and sleep is needed.
Features of the neighborhood social environment often interact and are collinear. For example, neighborhoods that are cohesive are likely to have higher perceptions of neighborhood safety. Therefore, examining social environment in aggregate is informative for defining how the culmination of these factors is associated with sleep. Data from the Multi-Ethnic Study of Atherosclerosis (MESA) demonstrate that an increase in the social environment (higher levels of social cohesion and safety) is associated with actigraphy-based and subjective reports of longer sleep duration, earlier sleep timing, and lower daytime sleepiness scores.26,33 However, the social environment was not associated with insomnia.26
Ambient Environment and Adult Sleep Health
Ambient features (light, noise, air quality, humidity, and temperature) are often correlated with built features such as urbanicity, population, and intersection density with more detrimental ambient features in denser urban areas. The ambient physical environment is also often patterned by SES and race/ethnicity, that is individuals of lower SES and minorities may be more likely to live in environments that have more pollution (ie, air, noise, light) and greater density.39
A prominent feature of urban environments is exposure to artificial light.40 Light pollution resulting from street and commercial building lights can produce inopportune light exposure at night, which may cause delayed sleep onset.41 Light affects circadian rhythms; exposure to artificial bright light during the nighttime can suppress melatonin secretion, and can delay sleep onset.42 Higher exposure to inopportune light is associated with prolonged sleep latency, circadian phase delay, and insufficient sleep.43
Neighborhood noises from disorderly bar patrons, night club music, police sirens, traffic jams, construction work, and other sources may create arousals that can interfere with sleep.44 Louder neighborhood noise and greater traffic noise has been associated with insomnia, shorter sleep duration, fragmented sleep architecture, lower sleep efficiency, poor sleep quality, and delayed sleep onset and may contribute to early awakenings and daytime sleepiness.44,45 In a study in Germany, road traffic noise had the strongest association with objectively measured sleep latency and continuity, whereas subjective sleep quality was most strongly associated with air and rail traffic noise exposure.46 This may reflect the differences in sound qualities (intensity, frequency, and consistency). Noise may potentially worsen sleep apnea by contributing to sleep instability through arousals. Additionally, road traffic, in addition to generating traffic noise, has the additional impact of traffic-related air pollution which is less than with air and rail traffic.
Ambient air pollution has been associated with sleep apnea, likely through effects on the upper airway. Upper airway inflammation in response to inhaled smoke may be the mechanism. Higher annual exposure to fine particulate matter < 2.5 micrometers or fine particles (PM2.5) and nitrogen oxides has been associated with greater odds of moderate to severe sleep apnea in studies in the United States and Taiwan.47,48 In the United States, a 10 ppb increase in nitrous dioxide was associated with a 39% increase in odds of sleep apnea.47 A study in Thailand found similar associations of AHI with indoor particulate matter >2.5 but <10 micrometers (PM10) levels.49 Living near roadways, with greater exposure to traffic noise and traffic-related air pollution, has also been linked to sleep apnea symptoms in Europe.50
Pediatric Sleep and the Environment
Physical Environment and Pediatric Sleep Health
A growing literature has demonstrated that neighborhood density, disadvantage, and local amenities for physical activity are all associated with sleep health outcomes among youth. For example, youth that reside in more urban or more densely populated areas have shorter sleep durations,51,52 higher odds of inadequate sleep,52,53 and higher rates of sleep-disordered breathing54 than those living in less dense areas. Obesogenic built environment features (lack of healthy food stores, low street connectivity, and mixed land use) which promote weight gain and sedentary behavior, as observed in adults, are also associated with BMI in children.55,56
Built Environment and Pediatric Sleep Health
Another mechanism through which neighborhood built environment may affect sleep health could be through the promotion of physical activity, which can be beneficial for sleep.57,58 Singh and Kenney53 found that children 6 to 17 years of age residing in neighborhoods lacking amenities (eg, parks/playgrounds, recreation/community center, access to a library/bookmobile) had higher odds of inadequate sleep than their peers living in neighborhoods with these amenities. A study of adolescents living in semirural communities in Alabama found that recreation facilities located closer to the adolescent’s home are associated with higher physical activity, which in turn predicted more daily sleep minutes, better quality sleep, and less variability in sleep schedules.59
Neighborhood Disadvantage and Pediatric Sleep Health
Children’s sleep may be more vulnerable to disadvantaged neighborhoods compared with adults. Furthermore, youth that live in lower SES neighborhoods exhibit poorer sleep health, including shorter nightly sleep durations60,61 and greater odds of inadequate sleep,53 than children and adolescents living in more advantaged neighborhoods. Notably, one study of children 5 to 10 years of age living in urban counties of California found that children living in neighborhoods with 40-year histories of consistently high poverty have higher odds of insufficient sleep than youth consistently residing in neighborhoods of low or moderate poverty.62 Teens living in more disadvantaged neighborhoods also have more variable sleep times63 and more sleep problems64,65 than those living in more advantaged neighborhoods.
Several epidemiologic studies have identified neighborhood disadvantage as an independent risk factor for childhood sleep apnea.54,66 Children who live in neighborhoods with low SES markers, such as higher unemployment rates, lower rates of higher education, higher proportion of poverty, and lower rates of home ownership, have greater odds of sleep apnea and more severe sleep apnea.54,66 Living in and growing up in deprived neighborhoods has been linked to childhood allergies and asthma outcomes, through effects on inflammatory pathways and stress response.67,68 This chronic inflammation coupled with obesity may explain the observed link of neighborhood SES with sleep apnea in children.
Social Environment and Pediatric Sleep Health
The association between neighborhood factors and sleep health may partially operate through exposure to neighborhood violence. Concern about violence is associated with a range of sleep problems and inadequate sleep among children and adolescents.65,69 Acute exposure to violent events is also associated with delayed sleep timing and shorter duration as assessed using diary and wrist-worn activity trackers.70 Using a rigorous within-person study design in a small sample of adolescents, Heissel et al70 found that adolescents go to sleep 30 min later and sleep for 39 min less on the night after a violent crime occurred within half a mile of their home.
Ambient Environment and Pediatric Sleep Health
Ambient environmental features such as indoor and outdoor air pollution may contribute to sleep and sleep disorders through inducing physiological changes in the developing upper and lower airways. Indoor air pollution from burning of biofuels has been associated with pediatric sleep apnea symptoms.71 Children had less snoring, sore throats, and nasal congestion when biomass was replaced with less polluting stoves.71 Children residing in neighborhoods with worse air quality in Iran had higher prevalence of snoring.72 However, to date, few studies have assessed for objective evidence of sleep apnea in children exposed to air pollution.
Conclusions and Future Directions
Growing epidemiologic data demonstrate that environmental features have a strong association with a range of sleep outcomes, as summarized in Table 1. The symptoms of restless sleep, delayed sleep onset, disrupted sleep, and snoring collected in many population surveys are not diagnostic for sleep disorders. However, these sleep outcomes associated with adverse neighborhood environments may be a harbinger of insomnia, insufficient sleep, circadian rhythm disorders, and sleep-disordered breathing pathology in the at-risk individual, Many of these environmental features are patterned by race and SES, with vulnerable populations—lower SES and racial minorities— experiencing a greater burden of air pollution, neighborhood disorder, lower social cohesion, more crime, and less proximity to green space. These contextual features are linked with poorer quality of sleep, less sleep opportunity, and more sleep-disordered breathing. The resulting sleep health disparities may contribute to socially patterned differences in self-reported health28 and the observed socioeconomic differences in cardiovascular health.73
Table 1.
Relationship of Physical (Natural and Built), Social, Ambient, and Neighborhood Environmental Features to Sleep Outcomes
| Environmental Feature | Longer Sleep Duration | ↑ Efficiency/↑ Quality | Short Latency | ↑OSA/BMI/AHI | Reference(s) |
|---|---|---|---|---|---|
| Natural | |||||
| Water | ↑ | 6 | |||
| Green space | ↑/↑a | 7, 9, 53 | |||
| Built | |||||
| Obesogenic | ↓a | ↑/↑a BMI | 10, 11, 12, 13, 55, 56 | ||
| ↑ Recreation | ↑a | ↑a | ↓ BMI | 15, 53, 59 | |
| Urban disorder | ↓ | ↓ | ↓ | 25, 28, 29, 30 | |
| ↑ Walkability | ↓ | ↓ AHI | 18, 21 | ||
| Density | ↓a | ↑ OSAa | 21, 51, 52, 53, 54 | ||
| Social | |||||
| ↑ Cohesion | ↑ | ↑ | 26, 33 | ||
| ↑ Fragmentation | ↓ | ↓ | ↓ | 29, 32, 33, 34 | |
| ↓ Safety/↑ Violence | ↓/↓a | ↓/… | ↓/↓a | 25, 26, 27, 35, 36, 37, 65, 69, 70 | |
| Ambient | |||||
| Artificial light | ↓ | 41, 42, 43 | |||
| Air pollution | ↑ OSA | 47, 48, 49, 50, 71, 72 | |||
| Noise | ↓ | ↓ | ↓ | 44, 45, 46 | |
| Neighborhood | |||||
| Disadvantage ↓ SES/↑ Deprivation | ↓/…/↓a | ↓/…/↓a | … | ↑ OSAa | 22, 23, 24, 25, 26, 27, 54,60, 61, 62, 63, 64, 65, 66 |
Obesogenic environment: ↓ street connectivity, ↓ mixed land use, and ↓ healthy food stores. ↑ = favorable effect on sleep outcomes (longer sleep duration, higher efficiency, and shorter latency), except for OSA/BMI/AHI outcome where ↑ indicates worse OSA and higher BMI and AHI; ↓ = unfavorable effect on sleep outcomes (lower sleep duration, worse efficiency and longer latency), exception of OSA/BMI/AHI where ↓ indicates less or decrease in; AHI = apnea hypopnea index.
Pediatric finding.
Features of the built, social, and ambient environment that are associated with adverse outcomes are more common in lower SES neighborhoods and those with higher proportions of racial and ethnic minorities. This sociodemographic clustering can make it difficult to identify whether the neighborhood-level associations with sleep health are because of a causal effect of neighborhood factors or because of compositional differences of the neighborhoods. Identifying the causal mechanisms requires the application of careful study design. Studies about environmental exposures usually require observational study methods, rather than experimental, which limits inferences; neighborhood and environmental interventions do not fit well into randomized controlled trials. However, place-based experimental and quasi-experimental studies could improve the scientific rigor of investigating the environment and sleep. Also, natural disasters (eg, earthquakes) and a change in local zoning and urban planning are also opportunities for expanding our knowledge of the environment and sleep.74 A quasi-experimental study found that neighborhood urban renewal was associated with reduced health inequalities by social class in Barcelona, Spain.75 Future research should seek to capture sleep outcome data from quasi-experimental or natural experiments resulting from public policy, city zoning laws, or environmental legislation changes to enable a better understanding of these complex relationships.
Future studies may also use the gains in objective measurement of sleep and the environment to enable a more accurate assessment of exposures and outcomes. Real-time person-level monitoring of air pollution, noise levels, and light exposure is now feasible. Additionally, more detailed GIS measures can provide objective assessments of neighborhood features including crowding, structure features, land use, and commercial properties. Consumer devices using actigraphy are now cheaper and less cumbersome, allowing population-level assessments of sleep, activity, and location. Additional developments of smartphone applications to detect sleep apnea and other sleep disorders may similarly improve population-level assessments of sleep health. Mobile devices with wearable technology may also allow for a more granular assessment of environmental exposures, capturing work, school, commuting, and residential ambient features such as light, noise, and air quality throughout the day.
The observational data reviewed regarding the associations of the environment on sleep health indicate that neighborhood-level interventions in the form of urban planning and policy changes may affect sleep outcomes and possibly reduce sleep disparities. Further studies are needed to assess if reducing urban noise, reducing artificial light, improving aesthetic qualities, and improving walkability yield improvements to sleep. Additionally, longitudinal studies investigating how environmental exposures across the life span influence sleep are needed. We propose evaluating interventions such as increasing green space with parks, trees, and water to improve the neighborhood built environment and possibly foster social cohesion as neighbors use the parks and build connections. Policy interventions in the form of taxes and incentives to reduce use of gasoline-combustion vehicles may improve air quality, reduce traffic-related noise pollution, and promote activity as more people walk, bike, or use public transportation. We hypothesize that the downstream effects of these neighborhood improvements, in part through better sleep health, may yield a healthier, less obese population with less cardiovascular and metabolic disease.
In conclusion, features of the physical and social environment may contribute to sleep health and may play a role in the development of sleep disorders. Policies that improve environmental conditions, from reducing air pollution to improving neighborhood safety, may reduce sleep health disparities and improve population sleep health.
Acknowledgments
Financial/nonfinancial disclosures: None declared.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Footnotes
FUNDING/SUPPORT: Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K01HL138211. Dr Hale also receives an honorarium from that National Sleep Foundation for her role as Editor-in-Chief of Sleep Health.
References
- 1.Buysse D.J. Sleep health: Can we define it? Does it matter? Sleep. 2014;37(1):9–17. doi: 10.5665/sleep.3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grandner M.A., Williams N.J., Knutson K.L., Roberts D., Jean-Louis G. Sleep disparity, race/ethnicity, and socioeconomic position. Sleep Med. 2016;18:7–18. doi: 10.1016/j.sleep.2015.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams D.R., Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116(5):404–416. doi: 10.1093/phr/116.5.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Christian H., Knuiman M., Divitini M. A longitudinal analysis of the influence of the neighborhood environment on recreational walking within the neighborhood: results from RESIDE. Environ Health Perspect. 2017;125(7):077009. doi: 10.1289/EHP823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McEwen B.S. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 6.Grigsby-Toussaint D.S., Turi K.N., Krupa M., Williams N.J., Pandi-Perumal S.R., Jean-Louis G. Sleep insufficiency and the natural environment: results from the US Behavioral Risk Factor Surveillance System survey. Prev Med. 2015;78:78–84. doi: 10.1016/j.ypmed.2015.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Astell-Burt T., Feng X., Kolt G.S. Does access to neighbourhood green space promote a healthy duration of sleep? Novel findings from a cross-sectional study of 259 319 Australians. BMJ Open. 2013;3(8) doi: 10.1136/bmjopen-2013-003094. pii: e003094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yeager R., Riggs D.W., DeJarnett N. Association between residential greenness and cardiovascular disease risk. J Am Heart Assoc. 2018;7(24) doi: 10.1161/JAHA.118.009117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Johnson B.S., Malecki K.M., Peppard P.E., Beyer K.M.M. Exposure to neighborhood green space and sleep: evidence from the Survey of the Health of Wisconsin. Sleep Health. 2018;4(5):413–419. doi: 10.1016/j.sleh.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayne S.L., Auchincloss A.H., Michael Y.L. Impact of policy and built environment changes on obesity-related outcomes: a systematic review of naturally occurring experiments. Obes Rev. 2015;16(5):362–375. doi: 10.1111/obr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brown A.F., Liang L.J., Vassar S.D. Neighborhood disadvantage and ischemic stroke: the Cardiovascular Health Study (CHS) Stroke. 2011;42(12):3363–3368. doi: 10.1161/STROKEAHA.111.622134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li F., Harmer P.A., Cardinal B.J. Built environment, adiposity, and physical activity in adults aged 50-75. Am J Prev Med. 2008;35(1):38–46. doi: 10.1016/j.amepre.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Auchincloss A.H., Mujahid M.S., Shen M., Michos E.D., Whitt-Glover M.C., Diez Roux A.V. Neighborhood health-promoting resources and obesity risk (the Multi-Ethnic Study of Atherosclerosis) Obesity (Silver Spring) 2013;21(3):621–628. doi: 10.1038/oby.2012.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Christine P.J., Auchincloss A.H., Bertoni A.G. Longitudinal associations between neighborhood physical and social environments and incident type 2 diabetes mellitus: the Multi-Ethnic Study of Atherosclerosis (MESA) JAMA Intern Med. 2015;175(8):1311–1320. doi: 10.1001/jamainternmed.2015.2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barrientos-Gutierrez T., Moore K.A.B., Auchincloss A.H. Neighborhood physical environment and changes in body mass index: results from the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2017;186(11):1237–1245. doi: 10.1093/aje/kwx186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peppard P.E., Young T., Barnet J.H., Palta M., Hagen E.W., Hla K.M. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol. 2013;177(9):1006–1014. doi: 10.1093/aje/kws342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith M., Hosking J., Woodward A. Systematic literature review of built environment effects on physical activity and active transport - an update and new findings on health equity. Int J Behav Nutr Phys Act. 2017;14(1):158. doi: 10.1186/s12966-017-0613-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Billings M.E., Johnson D.A., Simonelli G. Neighborhood walking environment and activity level are associated with OSA: the Multi-Ethnic Study of Atherosclerosis. Chest. 2016;150(5):1042–1049. doi: 10.1016/j.chest.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Awad K.M., Malhotra A., Barnet J.H., Quan S.F., Peppard P.E. Exercise is associated with a reduced incidence of sleep-disordered breathing. Am J Med. 2012;125(5):485–490. doi: 10.1016/j.amjmed.2011.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mendelson M., Lyons O.D., Yadollahi A., Inami T., Oh P., Bradley T.D. Effects of exercise training on sleep apnoea in patients with coronary artery disease: a randomised trial. Eur Respir J. 2016;48(1):142–150. doi: 10.1183/13993003.01897-2015. [DOI] [PubMed] [Google Scholar]
- 21.Johnson D.A., Hirsch J.A., Moore K.A., Redline S., Diez Roux A.V. Associations between the built environment and objective measures of sleep: the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2018;187(5):941–950. doi: 10.1093/aje/kwx302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bassett E., Moore S. Neighbourhood disadvantage, network capital and restless sleep: Is the association moderated by gender in urban-dwelling adults? Soc Sci Med. 2014;108:185–193. doi: 10.1016/j.socscimed.2014.02.029. [DOI] [PubMed] [Google Scholar]
- 23.Fuller-Rowell T.E., Curtis D.S., El-Sheikh M., Chae D.H., Boylan J.M., Ryff C.D. Racial disparities in sleep: the role of neighborhood disadvantage. Sleep Med. 2016;27-28:1–8. doi: 10.1016/j.sleep.2016.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Watson N.F., Horn E., Duncan G.E., Buchwald D., Vitiello M.V., Turkheimer E. Sleep duration and area-level deprivation in twins. Sleep. 2016;39(1):67–77. doi: 10.5665/sleep.5320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson D.A., Lisabeth L., Hickson D. The social patterning of sleep in African Americans: associations of socioeconomic position and neighborhood characteristics with sleep in the Jackson Heart Study. Sleep. 2016;39(9):1749–1759. doi: 10.5665/sleep.6106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Desantis A.S., Diez Roux A.V., Moore K., Baron K.G., Mujahid M.S., Nieto F.J. Associations of neighborhood characteristics with sleep timing and quality: the Multi-Ethnic Study of Atherosclerosis. Sleep. 2013;36(10):1543–1551. doi: 10.5665/sleep.3054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson D.A., Brown D.L., Morgenstern L.B., Meurer W.J., Lisabeth L.D. The association of neighborhood characteristics with sleep duration and daytime sleepiness. Sleep Health. 2015;1(3):148–155. doi: 10.1016/j.sleh.2015.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hale L., Hill T.D., Burdette A.M. Does sleep quality mediate the association between neighborhood disorder and self-rated physical health? Prev Med. 2010;51(3-4):275–278. doi: 10.1016/j.ypmed.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 29.DeSantis A., Troxel W.M., Beckman R. Is the association between neighborhood characteristics and sleep quality mediated by psychological distress? An analysis of perceived and objective measures of 2 Pittsburgh neighborhoods. Sleep Health. 2016;2(4):277–282. doi: 10.1016/j.sleh.2016.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chen-Edinboro L.P., Kaufmann C.N., Augustinavicius J.L. Neighborhood physical disorder, social cohesion, and insomnia: results from participants over age 50 in the Health and Retirement Study. Int Psychogeriatr. 2015;27(2):289–296. doi: 10.1017/S1041610214001823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ross C.E., Mirowsky J. Neighborhood disadvantage, disorder, and health. J Health Soc Behav. 2001;42(3):258–276. [PubMed] [Google Scholar]
- 32.Johnson D.A., Billings M.E., Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Curr Epidemiol Rep. 2018;5(2):61–69. doi: 10.1007/s40471-018-0139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Johnson D.A., Simonelli G., Moore K. The neighborhood social environment and objective measures of sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep. 2017;40(1) doi: 10.1093/sleep/zsw016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Young M.C., Gerber M.W., Ash T., Horan C.M., Taveras E.M. Neighborhood social cohesion and sleep outcomes in the Native Hawaiian and Pacific Islander National Health Interview Survey. Sleep. 2018;41(9) doi: 10.1093/sleep/zsy097. [DOI] [PubMed] [Google Scholar]
- 35.Troxel W.M., DeSantis A., Richardson A.S. Neighborhood disadvantage is associated with actigraphy-assessed sleep continuity and short sleep duration. Sleep. 2018;41(10) doi: 10.1093/sleep/zsy140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simonelli G., Dudley K.A., Weng J. Neighborhood factors as predictors of poor sleep in the Sueno Ancillary Study of the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sleep. 2016;40(1) doi: 10.1093/sleep/zsw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hill T.D., Trinh H.N., Wen M., Hale L. Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med. 2016;18:56–60. doi: 10.1016/j.sleep.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 38.Ruff R.R., Ng J., Jean-Louis G., Elbel B., Chaix B., Duncan D.T. Neighborhood stigma and sleep: findings from a pilot study of low-income housing residents in New York City. Behav Med. 2018;44(1):48–53. doi: 10.1080/08964289.2016.1203754. [DOI] [PubMed] [Google Scholar]
- 39.Evans G.W., Marcynyszyn L.A. Environmental justice, cumulative environmental risk, and health among low- and middle-income children in upstate New York. Am J Public Health. 2004;94(11):1942–1944. doi: 10.2105/ajph.94.11.1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chepesiuk R. Missing the dark: health effects of light pollution. Environ Health Perspect. 2009;117(1):A20–A27. doi: 10.1289/ehp.117-a20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ohayon M.M., Milesi C. Artificial outdoor nighttime lights associate with altered sleep behavior in the American general population. Sleep. 2016;39(6):1311–1320. doi: 10.5665/sleep.5860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cho Y., Ryu S.-H., Lee B.R., Kim K.H., Lee E., Choi J. Effects of artificial light at night on human health: a literature review of observational and experimental studies applied to exposure assessment. Chronobiol Int. 2015;32(9):1294–1310. doi: 10.3109/07420528.2015.1073158. [DOI] [PubMed] [Google Scholar]
- 43.Koo Y.S., Song J.Y., Joo E.Y. Outdoor artificial light at night, obesity, and sleep health: cross-sectional analysis in the KoGES study. Chronobiol Int. 2016;33(3):301–314. doi: 10.3109/07420528.2016.1143480. [DOI] [PubMed] [Google Scholar]
- 44.Halperin D. Environmental noise and sleep disturbances: A threat to health? Sleep Sci. 2014;7(4):209–212. doi: 10.1016/j.slsci.2014.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Frei P., Mohler E., Roosli M. Effect of nocturnal road traffic noise exposure and annoyance on objective and subjective sleep quality. Int J Hyg Environ Health. 2014;217(2-3):188–195. doi: 10.1016/j.ijheh.2013.04.003. [DOI] [PubMed] [Google Scholar]
- 46.Basner M., Muller U., Elmenhorst E.M. Single and combined effects of air, road, and rail traffic noise on sleep and recuperation. Sleep. 2011;34(1):11–23. doi: 10.1093/sleep/34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Billings M.E., Gold D., Szpiro A. The association of ambient air pollution with sleep apnea: the Multi-Ethnic Study of Atherosclerosis. Ann Am Thorac Soc. 2019;16(3):363–370. doi: 10.1513/AnnalsATS.201804-248OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shen Y.L., Liu W.T., Lee K.Y., Chuang H.C., Chen H.W., Chuang K.J. Association of PM2.5 with sleep-disordered breathing from a population-based study in Northern Taiwan urban areas. Environ Pollut. 2017;233:109–113. doi: 10.1016/j.envpol.2017.10.052. [DOI] [PubMed] [Google Scholar]
- 49.Lappharat S., Taneepanichskul N., Reutrakul S., Chirakalwasan N. Effects of bedroom environmental conditions on the severity of obstructive sleep apnea. J Clin Sleep Med. 2018;14(4):565–573. doi: 10.5664/jcsm.7046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gislason T., Bertelsen R.J., Real F.G. Self-reported exposure to traffic pollution in relation to daytime sleepiness and habitual snoring: a questionnaire study in seven North-European cities. Sleep Med. 2016;24:93–99. doi: 10.1016/j.sleep.2016.08.007. [DOI] [PubMed] [Google Scholar]
- 51.Bottino C.J., Rifas-Shiman S.L., Kleinman K.P. The association of urbanicity with infant sleep duration. Health Place. 2012;18(5):1000–1005. doi: 10.1016/j.healthplace.2012.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Patte K.A., Qian W., Leatherdale S.T. Sleep duration trends and trajectories among youth in the COMPASS study. Sleep Health. 2017;3:309–316. doi: 10.1016/j.sleh.2017.06.006. [DOI] [PubMed] [Google Scholar]
- 53.Singh G.K., Kenney M.K. Rising prevalence and neighborhood, social, and behavioral determinants of sleep problems in US children and adolescents, 2003-2012. Sleep Disord. 2013;2013:394320. doi: 10.1155/2013/394320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Brouillette R.T., Horwood L., Constantin E., Brown K., Ross N.A. Childhood sleep apnea and neighborhood disadvantage. J Pediatr. 2011;158(5):789–795.e1. doi: 10.1016/j.jpeds.2010.10.036. [DOI] [PubMed] [Google Scholar]
- 55.Sharifi M., Sequist T.D., Rifas-Shiman S.L. The role of neighborhood characteristics and the built environment in understanding racial/ethnic disparities in childhood obesity. Prev Med. 2016;91:103–109. doi: 10.1016/j.ypmed.2016.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carroll-Scott A., Gilstad-Hayden K., Rosenthal L. Disentangling neighborhood contextual associations with child body mass index, diet, and physical activity: the role of built, socioeconomic, and social environments. Soc Sci Med. 2013;95:106–114. doi: 10.1016/j.socscimed.2013.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Alessi C.A., Yoon E.J., Schnelle J.F., Al-Samarrai N.R., Cruise P.A. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: Do sleep and agitation improve? J Am Geriatr Soc. 1999;47(7):784–791. doi: 10.1111/j.1532-5415.1999.tb03833.x. [DOI] [PubMed] [Google Scholar]
- 58.Foti K.E., Eaton D.K., Lowry R., McKnight-Ely L.R. Sufficient sleep, physical activity, and sedentary behaviors. Am J Prev Med. 2011;41(6):596–602. doi: 10.1016/j.amepre.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 59.Philbrook L.E., El-Sheikh M. Associations between neighborhood context, physical activity, and sleep in adolescnets. Sleep Health. 2016;2(3):205–210. doi: 10.1016/j.sleh.2016.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.McLaughlin Crabtree V., Beal Korhonen J., Montgomery-Downs H.E., Faye Jones V., O'Brien L.M., Gozal D. Cultural influences on the bedtime behaviors of young children. Sleep Med. 2005;6(4):319–324. doi: 10.1016/j.sleep.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 61.Bagley E.J., Fuller-Rowell T.E., Saini E.K., Philbrook L.E., El-Sheikh M. Neighborhood economic deprivation and social fragmentation: associations with children's sleep. Behav Sleep Med. 2018;16(6):542–552. doi: 10.1080/15402002.2016.1253011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sheehan C., Powers D., Margerison-Zilko C., McDevitt T., Cubbin C. Historical neighborhood poverty trajectories and child sleep. Sleep Health. 2018;4(2):127–134. doi: 10.1016/j.sleh.2017.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Marco C.A., Wolfson A.R., Sparling M., Azuaje A. Family socioeconomic status and sleep patterns of young adolescents. Behav Sleep Med. 2011;10(1):70–80. doi: 10.1080/15402002.2012.636298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Rubens S.L., Gudino O.G., Fite P.J., Grande J.M. Individual and neighborhood stressors, sleep problems, and symptoms of anxiety and depression among Latino youth. Am J Orthopsychiatry. 2018;88(2):161–168. doi: 10.1037/ort0000234. [DOI] [PubMed] [Google Scholar]
- 65.Rubens S.L., Fite P.J., Cooley J.L., Canter K.S. The role of sleep in the relation between community violence exposure and delinquency among Latino adolescence. J Community Psychol. 2014;42:723–734. [Google Scholar]
- 66.Wang R., Dong Y., Weng J. Associations among neighborhood, race, and sleep apnea severity in children. A six-city analysis. Ann Am Thorac Soc. 2017;14(1):76–84. doi: 10.1513/AnnalsATS.201609-662OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Keet C.A., Matsui E.C., McCormack M.C., Peng R.D. Urban residence, neighborhood poverty, race/ethnicity, and asthma morbidity among children on Medicaid. J Allergy Clin Immunol. 2017;140(3):822–827. doi: 10.1016/j.jaci.2017.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Williams D.R., Sternthal M., Wright R.J. Social determinants: taking the social context of asthma seriously. Pediatrics. 2009;123 suppl 3:S174–S184. doi: 10.1542/peds.2008-2233H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bagley E.J., Tu K.M., Buckhalt J.A., El-Sheikh M. Community violence concerns and adolescent sleep. Sleep Health. 2016;2(1):57–62. doi: 10.1016/j.sleh.2015.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Heissel J.A., Sharkey P.T., Torrats-Espinosa G., Grant K., Adam E.K. Violence and vigilance: the acute effects of community violent crime on sleep and cortisol. Child Dev. 2018;89(4):e323–e331. doi: 10.1111/cdev.12889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Castaneda J.L., Kheirandish-Gozal L., Gozal D., Accinelli R.A. Effect of reductions in biomass fuel exposure on symptoms of sleep apnea in children living in the peruvian andes: a preliminary field study. Pediatr Pulmonol. 2013;48(10):996–999. doi: 10.1002/ppul.22720. [DOI] [PubMed] [Google Scholar]
- 72.Kheirandish-Gozal L., Ghalebandi M., Salehi M., Salarifar M.H., Gozal D. Neighbourhood air quality and snoring in school-aged children. Eur Respir J. 2014;43(3):824–832. doi: 10.1183/09031936.00113113. [DOI] [PubMed] [Google Scholar]
- 73.Kingsbury J.H., Buxton O.M., Emmons K.M. Sleep and its relationship to racial and ethnic disparities in cardiovascular disease. Curr Cardiovasc Risk Rep. 2013;7(5) doi: 10.1007/s12170-013-0330-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li X., Buxton O.M., Hikichi H. Predictors of persistent sleep problems among older disaster survivors: a natural experiment from the 2011 Great East Japan earthquake and tsunami. Sleep. 2018;41(7) doi: 10.1093/sleep/zsy084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Mehdipanah R., Rodriguez-Sanz M., Malmusi D. The effects of an urban renewal project on health and health inequalities: a quasi-experimental study in Barcelona. J Epidemiol Community Health. 2014;68(9):811–817. doi: 10.1136/jech-2013-203434. [DOI] [PubMed] [Google Scholar]