Abstract
Objectives:
Our hands play a remarkable role in our activities of daily living and the make-up of our identities. In the United States, an estimated 41,000 individuals live with upper limb loss. Our expanding experience in limb transplantation—including operative techniques, rehabilitation, and expected outcomes—has often been based on our past experience with replantation. Here, we undertake a systematic review of replantation with transplantation in an attempt to better understand the determinants of outcome for each and to provide a summary of the data to this point.
Methods:
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines, we conducted PubMed searches from 1964 to 2013 for articles in English. In total, 53 primary and secondary source articles were found to involve surgical repair (either replantation or transplantation) for complete amputations at the wrist and forearm levels. All were read and analyzed.
Results:
Hand replantations and transplantations were compared with respect to pre-operative considerations, surgical techniques, post-operative considerations and outcomes, including motor, sensation, cosmesis, patient satisfaction/quality of life, adverse events/side effects, financial costs, and overall function. While comparison of data is limited by heterogeneity, these data support our belief that good outcomes depend on patient expectations and commitment.
Conclusion:
When possible, hand replantation remains the primary option after acute amputation. However, when replantation fails or is not possible, hand transplantation appears to provide at least equal outcomes. Patient commitment, realistic expectations, and physician competence must coincide to achieve the best possible outcomes for both hand replantation and transplantation.
Keywords: Vascularized composite allotransplantation, upper extremity, functional outcomes
Introduction
Hands are essential to our identities and activities of daily living (ADL). Yet, approximately 41,000 Americans suffer upper extremity (UE) loss.1 Many have lost their extremity as Service Members in the Middle East, where improved body armor has increased the number of those surviving previously fatal improvised explosive device injuries.2
UE replantation dates back to 1964,3 with over 300 major UE replants documented since.4 The literature mostly contains case studies combining replantations at multiple levels and/or complete and partial amputations and offers few standardized metrics of comparison or long-term outcomes.5 We have restricted our review to replants and transplants between the elbow and wrist to improve the validity of comparison.
Although replantation of extremities shortly after traumatic amputation may be technically feasible, it is often impossible due to the state of the amputated limb(s), the clinical stability of the patient, and/or the need for reperfusion within hours. Until the advent of hand transplantation in 1998, the only option for these UE amputees was the use of insensate prostheses.6 However, as of May 2013, the International Registry on Hand and Composite Tissue Transplantation (IRHCTT) reported that 45 patients received 68 UE transplants at levels between the wrist and proximal forearm (22 unilateral and 23 bilateral). Follow-up ranged from 0.5 to 14 years, with 94% of transplants surviving.7 These data exclude 15 transplants performed in China, of which 7 were lost 1–2 years post-operatively to rejection and necrosis, 6 of them in patients who were non-adherent with immunosuppression.8
Although the surgical techniques, rehabilitation, and outcomes of UE transplantation are based on replantation experience, there are important and significant differences. Given the limited and heterogeneous data available, a rigorous scientific comparison is not possible. However, our rationale in this review was to provide insights for the treatment of both patient groups, with similar goals to achieve limb survival and useful long-term function.
Methods
Following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we conducted PubMed searches as described in Table 1. We retrieved 512 articles, from 1964 to 2013 and read all abstracts. We excluded 459 primary and secondary source articles with amputations distal to the wrist and proximal to the elbow. Of the remaining articles, 53 were thoroughly reviewed.
Table 1.
Parameters for PubMed search.
| Keywords | Hand; replantation; replant; vascularized composite tissue; transplantation; transplant; allotransplantation; outcomes |
| Dates of publication | 1964 to 2013 |
| Languages | English |
Results
Pre-operative considerations
Replantation is inherently an acute and urgent operation, with little predictability or option for planning, and often significant warm ischemia time. Conversely, transplantation allows time for more thorough pre-operative planning, preparation, and optimization. This may include pre-operative medical and radiological work-up, psychiatric and psychological evaluation, and immunosuppression considerations which aim at improving success. The need for a donor in UE transplantation introduces numerous challenges not present in replantation, such as size, gender, and aesthetic matching, and the potential for limiting overall ischemic time and planned cold ischemia (which is not an option when replanting an UE).7
Surgical techniques
Excess tissue and “spare parts” available in UE transplantation provide opportunities for refinements not available in replantation. Excess length of tendons allows coaptation using techniques, such as Pulvertaft weaves and junctures at a variety of levels. This may maximize the strength and reliability of tenorrhaphy and may minimize adhesions, compared with end-to-end junctures at pre-determined locations in replants. The potential procurement of more arteries and veins at more proximal sites in transplantation provides extra vessel length, allowing anastomoses without tension or grafting and the use of larger (and potentially more reliable) vessels. Transplanted skin incisions and closures may be carefully planned to create a more acceptable scar and minimize contractures when compared with replantation. Furthermore, bone shortening is not typically needed in transplants since more soft tissue may be procured, whereas bone shortening is often necessary in replants to minimize tension on repairs and allow avoidance of surgery in the “zone of injury.” Stated another way, bone shortening is soft tissue lengthening and vice versa, and not typically needed in transplantation.
Bone fixation is most often achieved with plates and screws in both UE replantation and transplantation. The time courses of bony union are equivalent in UE transplants and replants; however, both are delayed compared with normal fracture healing.9 This may be related to the comparative degree of “trauma” and de-vascularization.
Nerves in limb amputees have often been shortened by traction neurectomy and often must be transected even more proximally while preparing a recipient limb for transplantation to remove distal neuromas. This introduces a longer distance for nerve regeneration in transplantation.
Finally, transplant surgeons encounter a larger degree of fibrosis and muscle atrophy secondary to the time between limb loss and transplantation and relative to the acute replantation situation.
Post-operative considerations
Hand transplant recipients typically receive more complex post-operative management when compared with replant recipients, including immunosuppression, intense rehabilitation, extended occupational therapy, and psychological support.7 They usually remain close to the transplant center for 3–6 months post-operatively. We were unable to find any data or protocols detailing similar information for replantation patients.
Outcomes
We compared seven outcome categories for hand replantation and transplantation (Table 2).
Table 2.
Comparison of similarities and differences between hand replantation and transplantation.
| Hand replantation | Hand transplantation | |
|---|---|---|
| 1. Motor | ● No cognitive therapy required | ● Nerve regeneration stimulated by immunosuppressive
medications ● Cognitive therapy required |
| ● Similar recovery of digit and wrist ranges of
motion ● Faster and improved extrinsic muscle recovery versus intrinsic ● Avulsion/crush amputations associated with worse outcomes in comparison with sharp | ||
| 2. Sensation | ● Near 100% protective sensation ● 30%–60% tactile and discriminatory |
● 100% protective sensation ● 80%–90% tactile and discriminatory |
| ● 2-PD < 10 mm ● More distal amputation associated with faster recovery ● Common cold intolerance | ||
| 3. Cosmesis | ● No tissue matching required ● More significant scarring with less restoration of soft tissues ● Higher risk of unequal UE lengths due to bone shortening |
● Size, gender, age, and skin color matching
issues ● Less significant scarring with better restoration of soft tissues ● Lower risk of unequal lengths |
| 4. Patient satisfaction/quality of life | ● Majority with improved self-reported quality of
life ● Lower patient satisfaction |
● 75% self-reported improvements in quality of
life ● Higher patient satisfaction |
| ● Many resumed suitable work without primary use of injured hand | ||
| 5. Adverse events/complications | ● Most common cause of replantation failure is arterial
insufficiency (60%) ● Second most common cause is venous insufficiency (20%) ● Overall higher rates of failure |
● Most common cause of transplantation failure is rejection
secondary to treatment non-compliance (China) ● One reports of chronic rejection ● Four other reported failures due to severe infection, intimal hyperplasia, and acute rejection (Western countries) ● 85% of reported cases have an episode of acute rejection (all but one case reversed with treatment) ● Immunosuppression-related side effects |
| ● Similar delays in bone union ● Common long-term complications include neuroma formation and tendon adhesions | ||
| 6. Financial costs | ● Unilateral lifetime
cost = US$42,561 ● (range = US$784–US$596,457) |
● Unilateral lifetime cost = US$509,275 ● Bilateral lifetime cost = US$529,395 |
| ● Difficult to evaluate and compare costs accurately due to the variety of components | ||
| 7. Overall function | ● Improvements after 5 years limited to cold intolerance and
SW monofilament sensation ● Majority return to at least 50% of overall original function |
● Improving HTSS and DASH scores over
12–13 years ● HTSS scores are generally excellent ● DASH scores generally show significant reductions in disabilities |
| ● Majority of Chen scores are Grades II (good) to III (fair) | ||
UE: upper extremity; HTSS: Hand Transplantation Score System; DASH: Disabilities of the Arm, Shoulder, and Hand; 2-PD: two-point discrimination.
Motor
The functions of the hand most important to ADLs are those related to pinch and grip. Nerve regeneration (prior to motor endplate senescence at around 18 months) is clearly a key factor in motor recovery, taking place at a rate of approximately 1 mm per day. Immunosuppressive medications used in transplant recipients have been shown to accelerate this rate.10,11
In a single-center study comparing five replants and one transplant, all at the forearm level,12 the replants had 17% greater grip strength but no motor reinnervation of the intrinsic muscles. In contrast, despite weaker grip strength, the transplants had hypothenar and interosseous muscle contractions by 21 months. Another study showed six replanted UE had 32% and 19% of pinch and grip power, respectively, of the contralateral uninjured hands at 29 months follow-up.13
Most transplanted forearm UE to date have preserved native extrinsic muscles with intact innervation, but reports of intrinsic reinnervation have been more variable.7,14 One study reports all 39 UE transplant recipients able to perform grip and pinch activities by 12 months and showing intrinsic recovery by 9–15 months,7 while another study states that by 1–10 years post-transplant, 57% of 28 recipients showed intrinsic motor function.15
An examination of 79 replantations found that motor outcomes were better for sharp versus diffuse crush or avulsion UE amputations.16 We infer that this applies to transplant too, but patient selection bias prohibits meaningful data. Stated another way, replantations are a heterogeneous group—some with sharp amputations but many with other mechanisms that predispose to poorer outcomes. All transplantations are, by definition, prepared to remove and sharply dissect damaged tissues, making these comparable with only the ideal replantation candidates.
Finally, cortical integration of a limb may be lost during prolonged time living as an amputee. Reintegration must occur for a recipient to gain control of a transplanted limb.17 Cognitive therapy is used to optimize this process, and post-transplant recovery of cortical motor activity has been demonstrated in multiple patients, but rigorous study of this factor is in its infancy.18–21 This is intrinsically not such an issue in replantation.
Sensation
Sensory recovery is most often tested by Semmes–Weinstein and two-point discrimination (2-PD) testing. These are reported as the degree of return of sensation (protective, tactile, or discriminatory) or a numerical 2-PD result, respectively. Normal 2-PD ranges from 2–4 mm on the finger pads to 8–15 mm on the palms. Immediately post-replantion or transplantion, all sensory functions in the surgical specimen are absent, and they only begin to reappear following nerve regeneration to sensory organs. Nerve biopsies of replanted versus intact hands show mean losses of sensory immunoreactivity and sympathetic immunoreactivity of 30% and 60%, respectively, after replantation.22 Outcomes are better in younger patients and those with more distal and sharp amputations.
Of 26 major UE replants with mean follow-up, 11.3 years,23 77%, 50%, and 27% had protective, tactile, and discriminatory sensation, respectively, and 67% had 6–10 mm 2-PD. In nine hand replants followed for an average 18 years, protective, tactile, and discriminatory sensation were 100%, 100%, and 56%, respectively, at 10–12 years, whereas 2-PD plateaued at 6–10 mm at 5 years.4 Approximately 50%–70% of hand replants regained 2-PD of less than 10–15 mm within months to years.8,16,24
As for UE transplant recipients, when followed long enough, 100% have recovered protective sensation, whereas 90% and 83% recovered tactile and discriminatory sensation, respectively. As in replantation, transplantation at more distal levels yielded better sensorimotor recovery, with persistent improvement beyond 2 years. In the previously noted single-center comparison,12 superior 2-PD was recorded in a transplant recipient compared with five replants (⩽12 mm versus 12–15 mm). Of the 12 successful hand transplants in China, 2-PD was reported to range from 1.5 to 6 mm.8
Common to both replants and transplants is cold intolerance of the affected extremity. While not quantified, this may be attributable to reduced thermal modulation capacities in the fingertips from microcirculatory deficiency.25
Cosmesis
Bone shortening and soft tissue injuries or loss contribute to significant detriments in cosmetic outcomes of UE replantation.26 Conversely, hand transplantations allow for as much bony and soft tissue procurement as necessary, thus allowing optimal relative bone length and minimized scarring. Most recipients express “satisfaction” with cosmetic results.27 The Hand Transplantation Score System (HTSS) includes cosmetic measures but no qualitative analysis of cosmesis.26
Patient satisfaction/quality of life
Global measures of satisfaction are critically important but difficult to quantify. This flaw is magnified by the lack of pre-amputation standardized data for both groups, while often using a surrogate of pre-transplant status in transplantation patients. At best, we are often comparing post-operative data with pre-injury data for replant patients and with post-injury data for transplant patients. The most common quality of life (QoL) instruments for this patient population are the short form (SF)-36 and Disabilities of the Arm, Shoulder, and Hand (DASH).
In the replant group, QoL correlated strongly with functional outcomes measured by Chen’s classification (Table 2) in wrist and forearm replants. The majority of recipients were satisfied with functional and cosmetic outcomes.28 QoL improved throughout a 4.2-year post-operative follow-up in 30 replant recipients with sharp amputation mechanisms.29 QoL studies over a longer period of follow-up were not found.
Several transplantation studies qualitatively report patient satisfaction.27,30 The majority (75%) of transplant recipients note improvements in QoL from pre-transplantation and the ability to perform most ADL. Although no degree of magnitude is specifically reported for QoL, the HTSS scoring system shows gradual improvements through 12–13 years post-transplant, with bilateral recipients only slightly more satisfied than unilateral recipients (Figures 1 and 2).7 The most significant determinants of QoL in replants and transplants were patient motivation, degree of psychological distress, personality, and support systems.31
Figure 1.
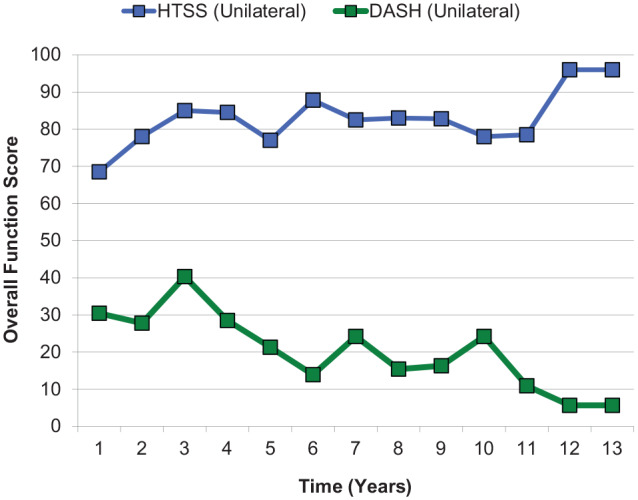
2013 International Registry on Hand and Composite Tissue Transplantation: unilateral transplant follow-up of overall function.32
Hand Transplantation Score System (HTSS): Higher score = improved function.
Disabilities of the Arm, Shoulder, and Hand (DASH): Lower score = decreased disability.
Figure 2.
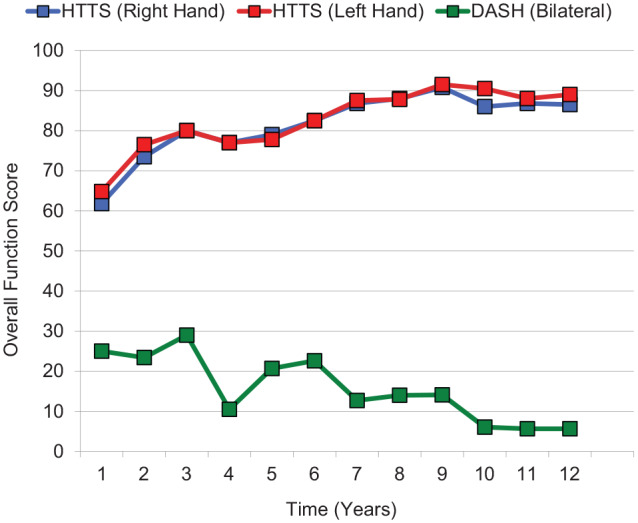
2013 International Registry on Hand and Composite Tissue Transplantation: bilateral transplant follow-up of overall function.32
Hand Transplantation Score System (HTSS): Higher score = improved function.
Disabilities of the Arm, Shoulder, and Hand (DASH): Lower score = decreased disability.
Adverse events/complications
The most common causes of replantation failure are arterial (58%) and venous (17%) insufficiency, according to a 1974 study.32 Late complications include neuroma formations, tendon adhesions, and cold intolerance.
Four Western UE transplant recipients have lost five transplanted hands as of 2013 as described in Table 3.33 Early post-transplant complications are typically thrombosis or small areas of skin necrosis, reported in 9% and 18% of patients in early IRHCTT reports. In total, 85% of UE transplant recipients experienced at least one episode of acute rejection within the first year; all were reversible when promptly treated. Recipients have been maintained on immunosuppression therapy most commonly consisting of steroids, tacrolimus, and mycophenolic acid,14 although a variety of reduced-immunosuppression regimens are becoming popular. Table 4 depicts IRHCTT-documented immunosuppressant-related complications as of May 2013, including 42 metabolic (53%), 36 opportunistic infections (45%), and 2 non-life-threatening malignancies (2.5%).33
Table 3.
Upper extremity transplant losses in Western recipients.
| Time elapsed between transplantation and loss | Reason(s) for allograft loss | Bilateral or unilateral loss | Other comments |
|---|---|---|---|
| 5 days | Necrosis secondary to sepsis | Bilateral | Patient received combined face and hand transplantation |
| 15 days | Poor revascularization | Bilateral | Amputation of distal phalanges |
| 23 months | Arterial acute ischemia with intimal hyperplasia | Unilateral | |
| 29 months | Rejection | Bilateral | Attributed to immunosuppression non-compliance |
| 45 days | Bacterial infection and bleeding | Unilateral | Patient received combined face and hand transplantation and died on day 65 post-transplant from cerebral anoxia secondary to airway obstruction |
Table 4.
IRHCTT documented complications as of May 2013 (percentage of total complications).33
| Metabolic complications (52.5%) | |
|---|---|
| Hyperglycemia | 20 |
| Increased creatinine values | 9 |
| Arterial hypertension | 6 |
| Avascular necrosis of the hip | 2 |
| Leukopenia | 2 |
| Cushing syndrome | 1 |
| Hyperparathyroidism | 1 |
| End-stage renal disease | 1 |
| Opportunistic infections (45%) | |
| Bacterial | 14 (one osteitis, three graft connective tissue infections) |
| Cytomegalovirus (CMV) | 10 |
| Cutaneous mycosis | 5 |
| Herpes virus (HSV) | 3 |
| Clostridium difficile | 2 |
| Herpes zoster virus (HZV) | 1 |
| Epstein-Barr virus (EBV) | 1 |
| Malignancies (2.5%) | |
| Basal cell carcinoma of nose | 1 |
| Lymphoproliferative disease | 1 |
Financial costs
Figure 3 depicts the lifetime costs of UE amputation, replantation, prosthetic adaptation, and transplantation.34–37 Although, due to immunosuppression complications, transplantation yields less quality-adjusted life years (QALYs) than prosthetic adaptation,38 patients typically favor bilateral hand transplantation over bilateral prostheses. The inherent bias in these data is that patients satisfied with prostheses are unlikely to seek out transplantation. The incremental cost-utility ratio of bilateral transplantation (versus prostheses) was US$381,961/QALY, exceeding the traditionally accepted US$50,000/QALY threshold.37 Furthermore, financial calculations projected over many years are very sensitive to changing prices and costs, decreasing costs of generic immunosuppressant medications; although the increasingly complex and expensive prostheses may change these data.
Figure 3.
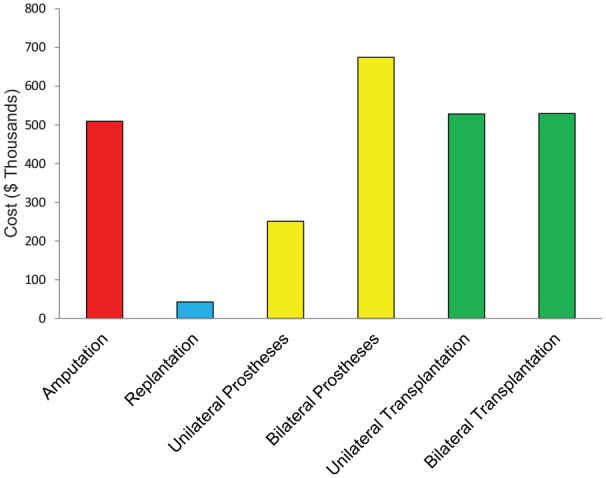
Estimated lifetime costs of UE amputation and associated procedures.
Overall function
Replantation data lack pre-morbid and pre-replant points. Conversely, transplantation data are generally replete but afford comparison to pre-transplant but not pre-amputation function. Furthermore, there is a notable lack of good instruments to measure post-operative function.
A retrospective analysis of 347 hand replants showed overall success rates were better for guillotine (77%) versus crush amputations (49%).39 Recently, Chen I scores were reported in four forearm-level replants followed for a mean of 18 years (Table 5).4 Chen I and II scores were noted in 8 distal forearm replantations,40 and Chen I, II, and III recoveries in 2, 5, and 3 mid-forearm replants, respectively. Over 11.5 years after hand replantation, Chen scores were 23% Grade IV, 12% Grade III, and 65% Grade II.23 There was increased patient satisfaction and improved use of the replant as a helper hand. Grossly, approximately 50% of function may be recovered with replantation.
Table 5.
Chen functional recovery score.
| Grade | Qualification | Description |
|---|---|---|
| I | Excellent | Able to resume original work with the injured hand, ROM > 60% of original, complete sensory recovery, and M4–5 motor power |
| II | Good | Able to resume suitable work without injured hand, ROM > 40%, near complete sensibility, and M3–4 motor power |
| III | Fair | Able to carry on daily life, ROM > 30%, partial recovery of sensibility, and M3 motor power |
| IV | Poor | Poor, almost non-useful function of limb |
ROM: range of motion.
In 28 transplants followed from 1 to 10 years, DASH scores dropped a mean of 27.6 points from pre- to post-transplant.1 Chen scores were recorded for all 17 patients, pre- and post-transplantation.15 All were Chen Grade IV pre-transplantation. In post-transplantation, 6% remained at Grade IV, 41% improved to Grade III, 47% Grade II, and 6% Grade I. HTSS and DASH scores for bilateral and unilateral transplants at 12–13 years follow-up represented “excellent” outcomes (Figures 2 and 3).33 Functional recovery enabled patients to perform most ADLs. Compliance with rehabilitation and immunosuppression was paramount for good results.
Discussion
Despite imperfect literature and limited experience, we believe that comparison between replantation and transplantation offers an opportunity to learn (Table 6). Our experience in reviewing this topic highlights the need for better data recording and better tools to assess outcomes and determinants thereof. The comparison is complex and complicated by heterogeneous data, most often presented as case reports or small case series. As expected, there is a paucity of data for bilateral (versus unilateral) UE replants, whereas bilateral transplantation is relatively common.
Table 6.
Lessons that can be learned from replantation and transplantation.
| 1. Motor | ● More extensive occupational therapy is likely
beneficial ● Immunosuppression may help nerve recovery independent of anti-rejection effects ● Balancing muscle and tendon lengths is difficult but important ● Upper limbs are very helpful to lower limb rehabilitation |
| 2. Sensation | ● Discriminatory sensation is frequently
attainable ● Sensory recovery continues for years |
| 3. Cosmesis | ● Significant psychosocial benefit from being seen to have
hands ● Ensuring appropriate and similar length limbs is important |
| 4. Patient Satisfaction/quality of life | ● There is an exponential disability with bilateral versus
unilateral limb loss ● Setting realistic expectations is important ● Patients may have goals that are not obvious to the medical/surgical team (e.g. improved balance, temperature regulation, fitting clothing) |
| 5. Adverse events/complications | ● Complications are very common ● Hands are very susceptible to ischemia as they are “end organs” ● Patient selection is critical to minimize adverse outcomes ● Planning is essential to limit complications ● A well-trained medical/surgical team who work well together is enormously helpful ● Ischemia likely causes poor later function (contributes to muscle fibrosis) ● Always consider life over limb when deciding whether to proceed |
| 6. Financial costs | ● Financial costs of limb restoration are on par with other
complex medical/surgical interventions ● The cost of a disability may be much higher than that of direct medical care |
| 7. Overall function | ● Absolute scores on functional assessments are not as important as the change in score (i.e. more disabled patients stand to gain more from replantation/transplantation) |
While we often cannot alter the circumstances of limb loss, we may apply some of the lessons learned. For example, when performing a revision amputation, leaving a longer UE stump without significant nerve shortening at this primary surgery may be less optimal for prosthetic fitting. However, if these patients proceed to future transplantation, they can be expected to have improved functional recovery due to the reduced distance for nerve re-growth and the maintenance of more native tissues, including innervated muscle. In addition, we recognize that vein and nerve grafts, commonly used in replantation, may help a surgeon from performing a tight anastomosis or neurorrhaphy. There is ample opportunity to procure these grafts from an organ donor, and we have obtained these in several transplantation cases.
Motor outcomes are critically related to what muscle is maintained in the proximal stump (and which works immediately) and to the degree and speed of nerve regeneration into a replanted or transplanted limb (allowing the part’s muscles to function). Hand replants appear to experience slower nerve regeneration compared with transplants; the later may benefit from accelerated nerve regeneration facilitated by immunosuppresive medications. There is debate as to whether these drugs should be used in the replant population for this benefit alone. Replants show a faster recovery of grip strength, most likely explained by less muscle atrophy at baseline, thus providing data to encourage transplantation closer to the time of amputation when practicable. Avulsion and crush amputations result in worse outcomes than sharp amputations for both groups.
Transplant patients have, additionally, often undergone a very extensive and planned occupational therapy program and demonstrate a selection bias favoring those patients likely to be compliant with therapy. While the contribution of this to outcomes has not been well studied and is limited by the retrospective nature of this review, it may contribute to reduced adhesions and better function. An interesting finding when researching this article was how infrequently reported is the amount and type of occupational therapy. This is especially true of replantation patients. The importance of occupational therapy is well-documented in hand surgery, and this is an opportunity to encourage better reporting of this aspect of data in our replantation and transplantation patients.
Transplants show better sensory return than replants.33 Tactile and discriminatory sensation are better recovered in transplants, but both groups present good 2-PD and near-total protective sensation recovery. Recovery is improved in both groups with more distal amputations and in younger patients.
Patients in both groups report adequate satisfaction with cosmetic results. Cosmetic outcome measurements, however, are intrinsically subjective and thus difficult to compare. Although neither surgery produces a “normal” appearance, outcomes may be optimized in transplantation thanks to optimal matching and planning. The use of “spare parts” in each type of surgery may further allow best possible results. Of note, a Polish man with bilateral amputations who received female UEs later expressed satisfaction with function and cosmesis despite the gender mismatch.41 Thus, patient preferences on cosmetic matching should be given consideration, particularly when matching is difficult and alternatives are limited.
Although both replant and transplant data demonstrate improved QoL, satisfaction appears greater among transplant recipients and is heavily based on pre-operative expectations. Direct comparison is difficult, given that replant recipients are only assessed post-operatively. Transplant recipients would be expected to experience higher satisfaction as they have had more time to experience the alternatives (such as prostheses), consider realistic outcomes, and understand post-operative rehabilitation. This is in contrast to replant recipients who deal with the intervention immediately after a traumatic injury often wrought with psychological trauma.31
Replant recipients have never experienced life without a limb. We consider the analogy of replant versus transplant recipients to recipients of immediate versus delayed breast reconstruction after mastectomy. In this group, satisfaction with appearance appears higher among the delayed group who have experienced the alternative of no reconstruction.42 Transplant recipients have experienced the difficulties of upper limb loss for months to years. Transplantation grants them new freedoms and physical abilities. In addition, they may receive greater psychological support. Understanding the role of this psychological support and potential media and public interest allowing better adaption may allow us to better help replantation patients through this experience.
Replantation patients may experience a higher overall rate of failure than transplantation patients, with vascular trauma being a large contributor. In contrast, the top cause of transplant failure is rejection due to non-adherence with immunosuppression. There is clearly a selection bias in these data, and lower failure rates in transplantation may be attributed to the ability to “hand pick” the best transplant candidates, a luxury not available in hand replantations. Furthermore, many surgeons will attempt replantation even if failure seems likely, as a high chance of failure may be better than no attempt at replantation at all. We may be reminded from our experience with transplantation how important the use of spare parts and tissue grafts can be. Immunosuppression-related side effects are common in the transplant group; however, general reductions in steroid use by many groups would be expected to decrease many of these complications. Both groups experience similar, yet delayed, rates of bone union. The most common long-term side effect in both groups is cold intolerance.
Although neither procedure is lifesaving, UE transplantation spurs more controversy than replantation because it imposes an absolute requirement for lifelong immunosuppression with potentially serious side effects.43 In contrast, replantation is perceived as an option where the patient is unlikely to be worse-off afterwards. Hand transplantation is also perceived as costly, specifically because of the long-term costs of immunosuppression, and the potential for dramatically increased costs in the setting of perioperative complications. Generic immunosuppressants may mitigate these costs somewhat. Rehabilitation is a significant cost contributor to both replantation and transplantation; but ongoing experience with transplantation would be expected to better elucidate the key and most efficient elements of rehabilitation.
Generally, replants have been scored using the Chen Functional Recovery Score, while transplants have used the HTSS. Only transplantation patients are registered with the IRHCTT. This limits direct comparisons of overall function. Nevertheless, both groups appear to regain at least 50% of original function. When compared with the emergent nature of replantation, the pre-operative transplantation process may increase the likelihood of successful post-operative compliance and cooperation. The use of better standardized measures with reliable recording will help elucidate further important determinants of outcome, and these are in the process of development.
Finally, given that donor hands must be rationed appropriately for transplantation, outcomes from replant data suggest that younger patients with guillotine-type injury to the distal forearm/wrist should be expected to have the best outcome from a mechanism of injury perspective. Transplant data further suggest that co-morbidities, mental health, medication compliance, and patient commitment to rehabilitation are also vital in making hand transplant allocation decisions.
The limitations of this article are vast. Foremost, the heterogeneity of data with respect to patient demographics, types of injury, amputation level, geographical location, clinical definitions, study design, and outcome measures makes direct comparisons difficult. Most of the replant literature includes digits, partial hands, and other levels of the UE, with limited numbers of distal forearm replants for comparison to transplants. Selection bias is inherent in transplantation since poor candidates (such as older, unfavorable level, or poorly compliant patients) will typically not be listed for this surgery, whereas the opportunity to select patients for replantation is more limited. Publication bias presumes that centers performing replants and/or transplants report their best results. Furthermore, most replantation articles were published in the 1970s–1980s versus the 2000s for transplantation, contributing a cohort effect to results. Surgical technology and knowledge have since evolved, thus it is likely that replantation outcomes have improved but have not been published secondary to the decreased novelty and publish-ability. The small number of transplants makes powered comparisons impossible.
Conclusion
Given the limitations of our retrospective literature review, it is difficult to draw firm conclusions, especially the cause-and-effect relationships, to outcomes. The purpose of this article is not to develop guidelines, but rather to draw our attention to the interesting similarities and differences. By taking a broad view of replantation and transplantation, we can identify aspects to be learned from one to benefit the other. In addition, certain common threads run through both patient groups. For instance, commitment to rehabilitation and patient expectations will often determine outcomes and satisfaction. Table 6 documents where we believe lessons can be learned from both replantation and transplantation.
Finally, this article serves as a reminder that we must continue to improve measurement and documentation of results if we are to improve outcomes. We hope that ongoing research into planning, techniques, rehabilitation, and outcomes in these distinct groups of patients will continue to improve the lives of future patients.
Acknowledgments
The authors thank the Brigham and Women’s Hospital Medical Library and Francis A. Countway Medical Library for their support in acquiring multiple articles. They also thank Dr Palmina Petruzzo and the International Registry on Hand and Composite Tissue Transplantation (IRHCTT) for kindly sharing the updated hand transplantation data.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The authors of this article, J.H., E.M.B., H.K., M.J.C., C.E.S., J.J.P., B.P., and S.G.T., state that all procedures followed in the studies described here were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 and 2008. The Hand Transplantation study at Brigham and Women’s Hospital is approved by the Partners Human Research Committee (Protocol #2012P000073).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Bohdan Pomahac  https://orcid.org/0000-0003-3703-8240
https://orcid.org/0000-0003-3703-8240
References
- 1. Ziegler-Graham K, MacKenzie EJ, Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008; 89(3): 422–429. [DOI] [PubMed] [Google Scholar]
- 2. Eskridge SL, Macera CA, Galarneau MR, et al. Injuries from combat explosions in Iraq: injury type, location, and severity. Injury 2012; 43(10): 1678–1682. [DOI] [PubMed] [Google Scholar]
- 3. Lee WP, Mathes DW. Hand transplantation: pertinent data and future outlook. J Hand Surg Am 1999; 24(5): 906–913. [DOI] [PubMed] [Google Scholar]
- 4. Gulgonen A, Ozer K. Long-term results of major upper extremity replantations. J Hand Surg 2012; 37(3): 225–232. [DOI] [PubMed] [Google Scholar]
- 5. Hoang NT. Hand replantations following complete amputations at the wrist joint: first experiences in Hanoi, Vietnam. J Hand Surg Br 2006; 31(1): 9–17. [DOI] [PubMed] [Google Scholar]
- 6. Zor F, Bozkurt M, Nair D, et al. A new composite midface allotransplantation model with sensory and motor reinnervation. Transpl Int 2010; 23(6): 649–656. [DOI] [PubMed] [Google Scholar]
- 7. Petruzzo P, Dubernard JM. The International Registry on Hand and Composite Tissue allotransplantation. Clin Transpl 2011; 2011: 247–253. [PubMed] [Google Scholar]
- 8. Pei G, Xiang D, Gu L, et al. A report of 15 hand allotransplantations in 12 patients and their outcomes in China. Transplantation 2012; 94(10): 1052–1059. [DOI] [PubMed] [Google Scholar]
- 9. Gabl M, Pechlaner S, Lutz M, et al. Bilateral hand transplantation: bone healing under immunosuppression with tacrolimus, mycophenolate mofetil, and prednisolone. J Hand Surg Am 2004; 29(6): 1020–1027. [DOI] [PubMed] [Google Scholar]
- 10. Chabas JF, Alluin O, Rao G, et al. FK506 induces changes in muscle properties and promotes metabosensitive nerve fiber regeneration. J Neurotrauma 2009; 26(1): 97–108. [DOI] [PubMed] [Google Scholar]
- 11. Rustemeyer J, van de Wal R, Keipert C, et al. Administration of low-dose FK 506 accelerates histomorphometric regeneration and functional outcomes after allograft nerve repair in a rat model. J Craniomaxillofac Surg 2010; 38(2): 134–140. [DOI] [PubMed] [Google Scholar]
- 12. Jablecki J, Kaczmarzyk L, Patrzalek D, et al. A detailed comparison of the functional outcome after midforearm replantations versus midforearm transplantation. Transplant Proc 2009; 41(2): 513–516. [DOI] [PubMed] [Google Scholar]
- 13. Matsuda M, Shibahara H, Kato N. Long-term results of replantation of 10 upper extremities. World J Surg 1978; 2(5): 603–612. [DOI] [PubMed] [Google Scholar]
- 14. Petruzzo P, Lanzetta M, Dubernard JM, et al. The International Registry on Hand and Composite Tissue Transplantation. Transplantation 2010; 90(12): 1590–1594. [DOI] [PubMed] [Google Scholar]
- 15. Landin L, Bonastre J, Casado-Sanchez C, et al. Outcomes with respect to disabilities of the upper limb after hand allograft transplantation: a systematic review. Transpl Int 2012; 25(4): 424–432. [DOI] [PubMed] [Google Scholar]
- 16. Tark KC, Kim YW, Lee YH, et al. Replantation and revascularization of hands: clinical analysis and functional results of 261 cases. J Hand Surg Am 1989; 14(1): 17–27. [DOI] [PubMed] [Google Scholar]
- 17. Chen R, Cohen LG, Hallett M. Nervous system reorganization following injury. Neuroscience 2002; 111(4): 761–773. [DOI] [PubMed] [Google Scholar]
- 18. Giraux P, Sirigu A, Schneider F, et al. Cortical reorganization in motor cortex after graft of both hands. Nat Neurosci 2001; 4(7): 691–692. [DOI] [PubMed] [Google Scholar]
- 19. Lanzetta M, Pozzo M, Bottin A, et al. Reinnervation of motor units in intrinsic muscles of a transplanted hand. Neurosci Lett 2005; 373(2): 138–143. [DOI] [PubMed] [Google Scholar]
- 20. Margreiter R, Brandacher G, Ninkovic M, et al. A double-hand transplant can be worth the effort! Transplantation 2002; 74(1): 85–90. [DOI] [PubMed] [Google Scholar]
- 21. Frey SH, Bogdanov S, Smith JC, et al. Chronically deafferented sensory cortex recovers a grossly typical organization after allogenic hand transplantation. Curr Biol 2008; 18(19): 1530–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wiberg M, Hazari A, Ljungberg C, et al. Sensory recovery after hand reimplantation: a clinical, morphological, and neurophysiological study in humans. Scand J Plast Reconstr Surg Hand Surg 2003; 37(3): 163–173. [DOI] [PubMed] [Google Scholar]
- 23. Sugun TS, Ozaksar K, Ada S, et al. Long-term results of major upper extremity replantations. Acta Orthop Traumatol Turc 2009; 43(3): 206–213. [DOI] [PubMed] [Google Scholar]
- 24. Tamai S. Digit replantation: Analysis of 163 replantations in an 11 year period. Clin Plast Surg 1978; 5(2): 195–209. [PubMed] [Google Scholar]
- 25. Klein-Weigel P, Pavelka M, Dabernig J, et al. Macro- and microcirculatory assessment of cold sensitivity after traumatic finger amputation and microsurgical replantation. Arch Orthop Trauma Surg 2007; 127(5): 355–360. [DOI] [PubMed] [Google Scholar]
- 26. Lanzetta M, Nolli R. A Comprehensive functional score system in hand transplantation. In: Lanzetta M, Dubernard JM. (eds) Hand transplantation. Milan: Springer, 2007, pp. 355–362. [Google Scholar]
- 27. Jensen SE, Butt Z, Bill A, et al. Quality of life considerations in upper limb transplantation: review and future directions. J Hand Surg Am 2012; 37(10): 2126–2135. [DOI] [PubMed] [Google Scholar]
- 28. Scott FA, Howar JW, Boswick JA., Jr Recovery of function following replantation and revascularization of amputated hand parts. J Trauma 1981; 21(3): 204–214. [DOI] [PubMed] [Google Scholar]
- 29. Syrko M, Jablecki J. Quality of life-oriented evaluation of late functional results of hand replantation. Ortop Traumatol Rehabil 2010; 12(1): 19–27. [PubMed] [Google Scholar]
- 30. Breidenbach WC, Gonzales NR, Kaufman CL, et al. Outcomes of the first 2 American hand transplants at 8 and 6 years posttransplant. J Hand Surg Am 2008; 33(7): 1039–1047. [DOI] [PubMed] [Google Scholar]
- 31. Bachmann D. Quality of life in hand transplant patients. In Lanzetta M, Dubernard JM. (eds) Hand transplantation. Milan: Springer, 2007, pp. 363–366. [Google Scholar]
- 32. O’Brien BM. Replantation surgery. Clin Plast Surg 1974; 1(3): 405–426. [PubMed] [Google Scholar]
- 33. Petruzzo P, Lanzetta M, Dubernard JM, et al. The International Registry on Hand and Composite Tissue Transplantation, https://europepmc.org/article/med/18724213 (accessed 24 May 2013). [DOI] [PubMed]
- 34. MacKenzie EJ, Jones AS, Bosse MJ, et al. Health-care costs associated with amputation or reconstruction of a limb-threatening injury. J Bone Joint Surg Am 2007; 89(8): 1685–1692. [DOI] [PubMed] [Google Scholar]
- 35. Blough DK, Hubbard S, McFarland LV, et al. Prosthetic cost projections for servicemembers with major limb loss from Vietnam and OIF/OEF. J Rehabil Res Dev 2010; 47(4): 387–402. [DOI] [PubMed] [Google Scholar]
- 36. Friedrich JB, Poppler LH, Mack CD, et al. Epidemiology of upper extremity replantation surgery in the United States. J Hand Surg Am 2011; 36(11): 1835–1840. [DOI] [PubMed] [Google Scholar]
- 37. Chung KC, Oda T, Saddawi-Konefka D, et al. An economic analysis of hand transplantation in the United States. Plast Reconstruct Surg 2010; 125(2): 589–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Farney AC, Doares W, Kaczmorski S, et al. Cost-effective immunosuppressive options for solid organ transplantation: a guide to lower cost for the renal transplant recipient in the USA. Immunotherapy 2010; 2(6): 879–888. [DOI] [PubMed] [Google Scholar]
- 39. Kleinert HE, Jablon M, Tsai TM. An overview of replantation and results of 347 replants in 245 patients. J Trauma 1980; 20(5): 390–398. [PubMed] [Google Scholar]
- 40. Battiston B, Tos P, Clemente A, et al. Actualities in big segments replantation surgery. J Plast Reconstr Aesthet Surg 2007; 60(7): 849–855. [DOI] [PubMed] [Google Scholar]
- 41. Disfigured soldier receives two hands from dead women in Poland. English Pravda.ru, 22 June 2010, http://english.pravda.ru/society/stories/22-06-2010/113963-dead_woman-0/ (accessed 11 May 2013).
- 42. Maksud D, Mooney K. Breast reconstruction: impact on timing and psychological responses. Plast Surg Nurs 1996; 16(3): 179–182. [Google Scholar]
- 43. Vicari-Christensen M, Repper S, Basile S, et al. Tacrolimus: review of pharmacokinetics, pharmacodynamics, and pharmacogenetics to facilitate practitioners’ understanding and offer strategies for educating patients and promoting adherence. Prog Transplant 2009; 19(3): 277–284. [DOI] [PubMed] [Google Scholar]


